Athlete with Diabetes
Gregory Czarnecki
Jake D. Veigel
INTRODUCTION
For patients with both type 1 and type 2 diabetes mellitus, exercise has been and continues to be an integral component of disease management. While exercise has shown improvements in comorbidities often associated with diabetes, including improved cholesterol profile, reduced blood pressure, and weight control or reduction, knowledge of the effects of exercise on glucose regulation is imperative for both the physician and the athlete. In high-risk subjects, lifestyle modifications have been shown to prevent type 2 diabetes.1 Exercise improves insulin sensitivity and thus may be of great benefit in most diabetics; however, this increased sensitivity may also put a diabetic athlete at increased risk of a hypoglycemic event. While tight glycemic control is paramount in preventing long-term complications of diabetes, caution must be taken during exercise.
PATHOPHYSIOLOGY
Type 1 diabetes is characterized by insulin deficiency from destruction of the pancreatic β cells, most commonly from an autoimmune process. Typical presentation and diagnosis is before age 30, but this is not absolute. Progression to requirement of exogenous insulin is the natural course of type 1 diabetes. Because of the ultimate reliance on exogenous insulin, hypoglycemic events are common, and despite aggressive management, such events may place the athlete at significant risk. While exercise may be of limited benefit in reducing hemoglobin A1c values, in part due to risk of hypoglycemia, in the type 1 diabetic it may provide significant benefits, including improved cardiovascular fitness, reduced resting systolic and diastolic blood pressures, and improved lipid profile.2,3
Type 2 diabetes is characterized by insulin resistance, impaired insulin secretion, and increased glucose production. A period of impaired glucose tolerance may be present for months to years preceding type 2 diabetes. Progression to requirement of exogenous insulin is not always the case in type 2 diabetes. Exercise has been shown in part to prevent or delay progression from insulin resistance to overt type 2 diabetes.4,5 A recent Cochrane review on exercise in type 2 diabetics showed significant improvements in glycemic control as well as reductions in plasma triglycerides and visceral fat with exercise programs irrespective of weight loss.6
Serum blood glucose levels in an otherwise healthy individual remain tightly controlled through the actions of both insulin and its counterregulatory hormones including glucagon, adrenaline, cortisol, and growth hormone. Fatty acids give greatest fuel contribution to skeletal muscle at rest. Initial fuel source during exercise begins with glycogen stores in skeletal muscle, followed by blood glucose and increasing fatty acid utilization. As serum blood glucose levels fall in response to tissue uptake, insulin secretion decreases. As this happens, there is an increase in the counterregulatory hormones, most notably glucagon and epinephrine. Through liver gluconeogenesis and glycogenolysis, there is increased glucose production to maintain serum levels as skeletal muscle continues its glucose uptake. Fatty acid mobilization is also increased through actions of the counterregulatory response, increasing through hepatic production.7
Two concerns that arise in diabetic athletes, type 1 or those with type 2 on insulin or secretagogue therapy, are of exercise-induced hypoglycemia and late-onset hypoglycemia. The first effect may occur as early as 30 minutes with exercise or for several hours following exercise. This occurs in part due to the inability to suppress insulin that has already been administered and alteration of the counterregulatory response as described in the following paragraphs. The second effect may continue to be realized up to 24 hours following the exercise activity and is due to enhanced insulin sensitivity.
GLUT4, a transport protein in skeletal muscle, is upregulated with both exercise and insulin and is responsible for increased uptake of blood glucose, thus improving sensitivity. Following exercise, glycogen stores need replenishment in both the liver and skeletal muscle. In this state, there is a period of hyperglycemia and hyperinsulinemia. GLUT4 contributes to the increased insulin sensitivity. It is important to avoid aggressive correction of blood glucose during this time due to the enhanced action of insulin. Following prolonged exercise, complete replacement of muscle glycogen may take up to 24 hours.8 Exogenous glucose is often necessary during prolonged or moderate-high-intensity exercise and in the recovery period.
Failure of the regulatory system in maintaining euglycemia and preventing hypoglycemia is a common concern and reality in the diabetic athlete. In type 1 diabetics and type 2 patients on insulin therapy, there is an inability to suppress exogenous insulin levels once administered. With an insulin excess, the body’s initial response of lowering serum insulin in the setting of falling blood glucose levels during exercise is lost. On the other hand, insulin deficiency during exercise may lead to further augmentation of the counterregulatory response with resultant hyperglycemia. This, in turn, may lead to precipitating diabetic ketoacidosis or a hyperosmolar nonketotic state.
Type 1 diabetics have been shown to lose the counterregulatory glucagon response to hypoglycemia early in the course of the disease. However, this glucagon response in type 1 diabetics is preserved with exercise, but this may also be lost with recent hypoglycemia prior to exercise.9 With the loss of the glucagon response to hypoglycemia, an increase in serum epinephrine becomes the next defense in the setting of decreasing serum glucose levels. This response may additionally become blunted in the setting of recent hypoglycemia. As noted earlier, through exercise with upregulation of GLUT4, insulin’s action is enhanced, and this effect may last hours after exercise. Two concepts that have been introduced to explain failed counterregulatory mechanisms in those with diabetes include hypoglycemia-associated and exercise-associated autonomic failures.
Hypoglycemia-associated autonomic failure occurs in response to recent hypoglycemia and puts the athlete at significant risk of precipitating further hypoglycemia, especially with repeated exercise. This failure has been shown in clinical studies in both nondiabetics and type 1 diabetics. The first failure as noted earlier is the loss of glucagon response to hypoglycemia. This may be followed by diminished epinephrine response to repeated hypoglycemia. With this blunted response, there is a decreased manifestation of autonomic symptoms that may present, and with this an unawareness by the patient of their hypoglycemia. With repeated exposures to hypoglycemia, this hypoglycemia unawareness edges to a lower and lower threshold. This counterregulatory failure has also been shown in moderate-intensity exercise following a period of hypoglycemia the previous day.9 Exercise-associated autonomic failure has been demonstrated with impaired counterregulatory response following prolonged exercise and next-day hypoglycemia, with the recent bout of exercise leading to impaired response to exposure of hypoglycemia.10 Counterregulatory failure may occur as early as 30 minutes into exercise with recent experience of hypoglycemia.9,10
EPIDEMIOLOGY
The prevalence of diabetes is estimated at 20.8 million in the United States, with 6.2 million of these being yet undiagnosed. Even more staggering is the 54 million estimated to have prediabetes, or insulin resistance. One in six overweight adolescents aged 12 to 19 are prediabetic, while 1 in 400 to 600 children and adolescents have type 1 diabetes. For those aged 60 years and older, roughly one in five have diabetes.11 Athletes with diabetes have successfully competed and succeeded at the highest levels in their sports. Successes include Olympic gold medals in swimming, grand slam titles in tennis, heavyweight boxing championships, and competitions in the Major League Baseball (MLB), the National Hockey League (NHL), and the National Football League (NFL) to name a few sports.12
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
History in the diabetic patient should focus not only on duration of disease, current level of glycemic control, and medications but also on potential complications of diabetes. Neuropathy, retinopathy, and microvascular disease are well-known complications of diabetes. Duration of disease is helpful in the screening of such conditions as is long-term and current level of glycemic control. Questioning should include a thorough history of hypoglycemic events including frequency, setting/timing, associated symptoms, severity, and level of treatment required, that is, self-administered or reliance on another individual. Patients on insulin or insulin secretagogues are at the greatest risk for hypoglycemic events with or without exercise. A history of diabetic ketoacidosis or hyperglycemic nonketotic coma is equally important. Is the athlete up to date on routine screenings such as ophthalmologic examinations and urine microalbumin? Symptoms associated with hypoglycemia may vary from patient to patient and include palpitations, anxiety, tremor, sweating, hunger, and possibly paresthesias. Fatigue, behavioral change, seizure, and loss of consciousness may occur. Additional symptoms that may be suggestive of hypoglycemia include decreased self-confidence, vivid dreams/nightmares, and disturbed sleep.7,10 These latter symptoms are especially important in obtaining history for nocturnal hypoglycemic events of which the athlete may be unaware. Has the athlete noted a change in or lack of symptoms of hypoglycemia?
When managing a diabetic athlete, an important start is determining the athlete’s current level of self-monitoring of blood glucose, exercise, and dietary regimens. Does the athlete have a sugar source readily available when exercising? Do they keep their glucometer nearby? What other medications is the athlete taking, including supplements? Medications such as β-blockers may blunt the adrenergic symptoms associated with hypoglycemia. What does the athlete know about foot care? Does the athlete routinely inspect their feet, preferably daily and before and after exercise? The physician should inquire about history of callus, ulcerations, blisters, or fissures. Symptoms of nausea and vomiting or early satiety may indicate underlying gastroparesis.
Is there a known history of diabetic retinopathy or nephropathy? Are there symptoms of peripheral or autonomic neuropathy? A well-known complication of microvascular disease is erectile dysfunction, which may give clues to the presence of other neuropathic diseases. Additionally, comorbidities, especially hypertension and hyperlipidemia, and smoking and family histories should be ascertained.
Evidence-based Physical Examination
Inspection should include assessment of skin integrity, especially at injection sites and the feet. Pay particular attention to identifying callus, ulcerations, blisters, or fissures. Acanthosis nigricans (Fig. 8.1) is associated with insulin resistance.
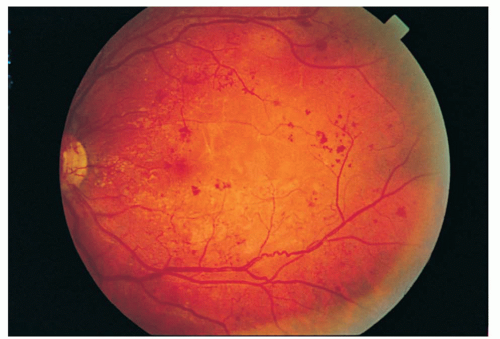
Perform a fundoscopic examination looking for microaneurysms, deep hemorrhages, or hard exudates that may be found with nonproliferative stage of retinopathy (Fig. 8.2). In the proliferative stage, findings may include neovascularization, vitreous hemorrhage, and proliferating fibrous tissue13 (Fig. 8.3).
 FIG. 8.1. Acanthosis nigricans. Reprinted with permission from Goodheart HP. Goodheart’s Photoguide of Common Skin Disorders. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2003. |
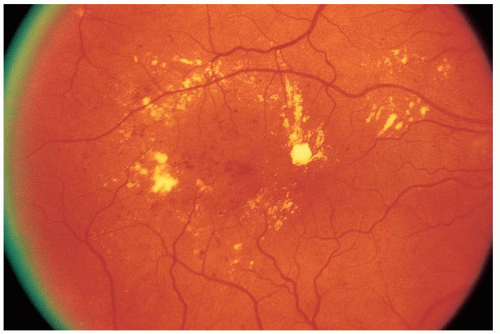 FIG. 8.2. Nonproliferative retinopathy. Reprinted with permission from Gold DH, Weingeist TA. Color Atlas of the Eye in Systemic Disease. Baltimore: Lippincott Williams & Wilkins; 2001. |
Thyroid palpation should also be routine. A thorough cardiac examination should be done, including blood pressure and, when indicated, orthostatic testing. Assess neurovascular status, noting strength of peripheral pulses and presence or absence of sensation via light touch, vibratory testing, or 10-g monofilament. Proprioception sense and reflexes should also be noted.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree