Athlete with Overuse Wrist and Hand Injuries
Patrick Guerrero
Xinning Li
INTRODUCTION
Chronic overuse injuries in the upper extremity are commonly seen in competitive or recreational athletes. It has been reported that 25% to 50% of all sports-related injuries can be attributed to overuse.1 Overuse is defined as repetitive microtrauma damage to the tissue that exceeds its ability to adapt. The term has been used in a broad spectrum of diagnosis that includes occupational, recreational, activity, or sports-related injuries. Handball, rowing, gymnastics, racquet sports, and volleyball are common sport activities involved in this injury pattern.2
FUNCTIONAL ANATOMY
Extensor Tendons
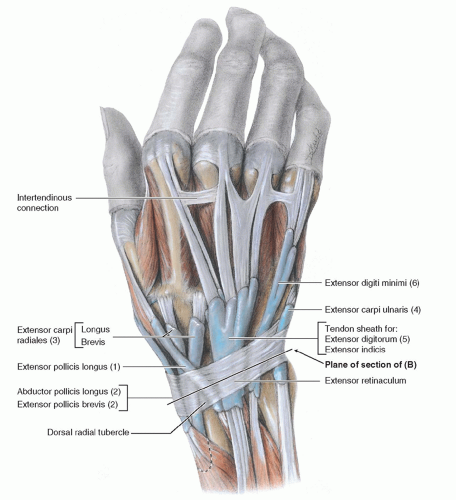
There are six dorsal compartments at the wrist level where extensor tendons gain entrance to the hand and are surrounded by a retinaculum (Fig. 14.1):
First compartment: Abductor pollicis longus (APL) and extensor pollicis brevis (EPB)
Second compartment: Extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) wrist extensors
Third compartment: Extensor pollicis longus (EPL)
Fourth compartment: Extensor digitorium communis (EDC) and extensor indicis propius (EIP) lying ulnar to the EDC
Fifth compartment: Extensor digiti minimi (EDM)
Sixth compartment: Extensor carpi ulnaris (ECU)
Another important structure is the juncturae tendinae (JT), which are interconnections between the EDC tendons that will allow finger extension in the event of extensor tendon laceration proximal to its insertion. Although there are several variations in the pattern of JT origin and insertion, the most common is from the extensor tendon of the ring finger proximal to the metacarpophlangeal (MCP) joint and inserts onto the middle and little finger extensor tendons.
Also, at this level, extensor tendons are covered by synovium. From the metacarpal heads lies the extensor hood, which blends with the common tendon and lateral bands (medial and lateral) to form the central tendons that insert into the base of the middle phalanx; this in turn affects proximal interphalangeal (PIP) joint extension. The lateral bands join together distally with fibers from the common extensor to form a triangular aponeurosis and attach to the base of the distal phalanx as the terminal tendon.
Flexor Tendons
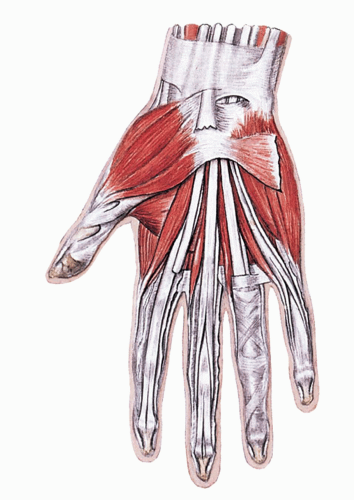
The carpal tunnel at the level of the wrist comprises nine tendons and the median nerve: four tendons from the flexor digitorum profundus (FDP), four from the flexor digitorum superficialis (FDS), and the flexor pollicis longus (FPL), which is the most radial structure (Fig. 14.2).
The brachialradialis (BR) originates on the lateral supracondylar ridge of the humerus and attaches to the distal radial styloid. The flexor carpi radialis (FCR) and flexor carpi ulnaris (FCU) are both wrist flexors and important during procedures involving tendon transfers or basal joint arthroplasty.
A series of annular (A1-A5) and cruciform (C1-C3) pullies envelop the tendons beginning slightly proximal to the metacarpal heads to maximize lever arm and minimize bowstringing. The odd-numbered pullies arise from the joint, while the even-numbered pullies are associated with the shaft. Preservation of the A2 and A4 pullies during surgery is essential in preventing bowstring of the flexor tendon. A synovial sheath envelops the FDS and FDP tendons to allow easy gliding as well as provide a source of nutrition. The FDS and FDP insert at the volar base of the middle and distal phalanx, respectively. The lumbricals are derived from the tendons of the FDP in the palm and insert on the radial lateral band of each finger. They are prime flexors of MCP joint and principal extensors of the interphalangeal joints. Laceration of the FDP tendon distal to the lumbrical insertion will result in paradoxical extension termed the “lumbrical plus” finger.
Bony and Ligamentous Anatomy
The radius articulates with the ulna via the sigmoid notch (distal radioulnar joint) at the wrist joint with a normal arc of motion ranging between 150 and 180 degrees of supination/pronation.
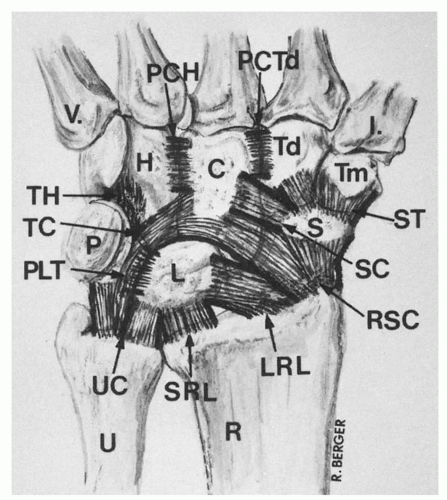
The normal arc of wrist flexion is 79 degrees, with wrist extension of 59 degrees, radial deviation of 21 degrees, and ulnar deviation of 38 degrees. The triangular fibrocartilage complex (TFCC) is the primary stabilizer of the distal radioulnar joint (DRUJ). The dorsal (Fig. 14.3) and volar (Fig. 14.4) radiocarpal and ulnocarpal (extrinsic) ligaments stabilize the wrist. In addition, multiple intercarpal and interosseous ligaments provide further stability to the wrist and aid in intercarpal motion. The MCP joints as well as the PIP and distal interphalangeal (DIP) joints are CAM shaped with varying degrees of collateral ligament tightness correlating flexion from 0 to 90 degrees (under maximum stretch with full flexion). A palm/volar plate as well as radial and ulnar collateral ligaments provide ligamentous stability during dorsal/volar and varus/valgus stresses, respectively.
The normal arc of wrist flexion is 79 degrees, with wrist extension of 59 degrees, radial deviation of 21 degrees, and ulnar deviation of 38 degrees. The triangular fibrocartilage complex (TFCC) is the primary stabilizer of the distal radioulnar joint (DRUJ). The dorsal (Fig. 14.3) and volar (Fig. 14.4) radiocarpal and ulnocarpal (extrinsic) ligaments stabilize the wrist. In addition, multiple intercarpal and interosseous ligaments provide further stability to the wrist and aid in intercarpal motion. The MCP joints as well as the PIP and distal interphalangeal (DIP) joints are CAM shaped with varying degrees of collateral ligament tightness correlating flexion from 0 to 90 degrees (under maximum stretch with full flexion). A palm/volar plate as well as radial and ulnar collateral ligaments provide ligamentous stability during dorsal/volar and varus/valgus stresses, respectively.
Triangular Fibrocartilage Complex
The TFCC stabilizes the distal radial ulna joint and provides stability at the ulnotriquetral joint. It can be prone to injury with repetitive weight-bearing activities involving ulnar deviation. The TFCC consists of a triangular cartilage disc known as the meniscus homolog as well as the dorsal and
volar ulnoradial ligaments, the ulnotriquetral and ulnolunate ligaments, and the tendon sheath of the ECU. The vascularity of the meniscus homolog is limited to the peripheral 15% to 20% and therefore prone to chronic tears.
volar ulnoradial ligaments, the ulnotriquetral and ulnolunate ligaments, and the tendon sheath of the ECU. The vascularity of the meniscus homolog is limited to the peripheral 15% to 20% and therefore prone to chronic tears.
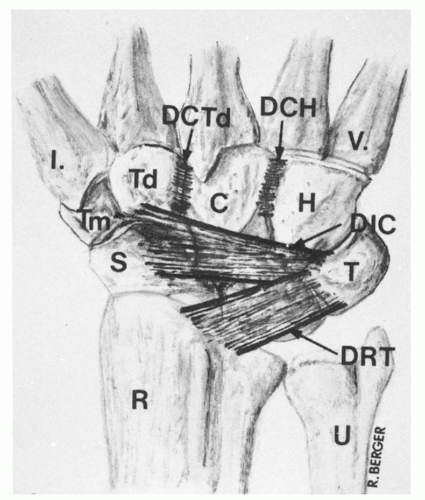 FIG. 14.3. Ligaments dorsal. From Bucholz RW, Heckman JD. Rockwood & Green’s Fractures in Adults. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001. |
Neurovascular Supply
The median nerve runs inside the carpal tunnel superficial and radial to the FDS for the ring and middle fingers and provides motor innervation to the thumb via the recurrent motor branch of median nerve and sensation to the radial three and one half digits. The ulnar nerve traverses the Guyon canal and supplies motor fibers to the hand intrinsics as well as sensation to the ulnar one and a half digits. It also gives a dorsal sensory branch to the dorsum of the hand. The superficial sensory branch of the radial nerve innervates the thumb, index, and occasionally middle fingers, dorsally. Blood supply is via the ulnar and radial arteries.
EPIDEMIOLOGY
Overuse hand and wrist injuries are common injuries sustained in athletes. The repetitive nature of many sports as well as the high degree of force transmitted through the hand and wrist make it particularly vulnerable. Common overuse injuries include de Quervain disease, intersection syndrome, TFCC tears, ECU tendonitis or subluxation, carpal tunnel syndrome, scaphoid fractures that may lead to nonunion, hook of hamate or pisifom fractures, and carpal instability. In the adolescent, overuse injuries may present as apophyseal inflammation. Sports associated with overuse to the hand and wrist include golf, racquet sports, gymnastics, rowing, and activities that require repetitive hand and wrist contact with a ball such as handball or volleyball.2 It has been estimated that 50% of all athletes will sustain an injury, with 25% to 50% secondary to overuse.1
Furthermore, a total of 703 golfers were retrospectively reviewed; 83% of them reported injuries involving overuse and 54% reported injuries involving the upper extremity.3 Over 85% of 518 recreational cyclists reported injury associated with overuse and 31% reported injury that involved the hand and wrist region.4 There is also a significant increase in the incidence of overuse injuries in the elite male volleyball players from 16% to 47% over a 10-year period.5 A recent epidemiology study of injury patterns in recreational rock climbers showed that 33% of 201 active climbers had suffered chronic overuse injuries.6
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
A thorough but focused history plays a crucial role in the diagnosis of overuse hand and wrist injuries. Key components include the age of the athlete, mechanism of injury, exacerbating and alleviating factors, as well as any associated symptoms. The age of the athlete is important, as more number of younger patients present with symptoms related to overuse. Also knowledge of the age of growth plate closure is important, as adolescent athlete may present with apophyseal injury. The mechanism and the acuity of onset of symptoms can also help in differentiating between overuse versus acute injuries. Asking about exacerbating and alleviating factors is essential in making the diagnosis, as pain tends to improve with rest in injuries related to overuse. The location of the presenting symptoms along with any neurologic compromise can also help in making the diagnosis. Moreover, acute pain related to a particular event/injury may be able to rule out overuse as a mechanism of injury.
Another important part of the history is asking about the level and practice time the patient spends each week on his/her respective sport. Also knowledge of factors during his/her sports activity that exacerbate his/her symptoms and which factors relieve them will be essential in making the diagnosis and direct treatment. Overuse injuries of the hand and wrist are also associated with more elite-level sports participation and prolonged training time.
Evidence-based Physical Examination
The physical examination plays a key role in the diagnosis of overuse hand and wrist injuries. The progression of one’s examination should include the following components as well as special tests:
Inspection
Inspection of the wrist and hand should first focus on visual examination. Particular attention should be paid to the area of the pain and inspection of the skin for lacerations/abrasions, chronic changes/swelling, or any deformities that will help in making the diagnosis. Furthermore, muscle atrophy in a particular region of the hand (thenar or hypothenar) may indicate chronic nerve impingement. A mass seen on the dorsal or volar surface may represent a ganglion cyst, which can indicate an underlying overuse injury to the tendon. It is also important to rule out infection with signs of erythema or warmth over the skin or joint.
Palpation
Palpation of the hand and wrist for overuse injuries involves assessing for deformities, point tenderness, swelling, and crepitus. Attention should be paid to the location of the pain, as ulnar- versus radial- or dorsal- versus volar-sided pain can help narrow the differential diagnosis. Point tenderness directly over a tendon or palpable crepitus can indicate chronic inflammation due to overuse. Tenderness over the hamate or the scaphoid may indicate an acute or stress fracture. Subluxation of the tendon with direct palpation may indicate chronic instability or overuse.
Range of Motion
Normal range of motion at the wrist is 79 degrees of flexion, 59 degrees of extension, 38 degrees of ulnar deviation, 21 degrees of radial deviation, and 80 degrees of forearm supination/pronation. A loss in the range of motion can indicate chronic inflammation of the tendon, restricting its ability to glide smoothly. Arthritis of the wrist or carpal bones due to scaphoid nonunion or lunate advance collapse may also restrict range of motion of the wrist secondary to pain.
Strength Tests
Strength testing should be performed as part of the evaluation with weakness possibility associated with muscle atrophy secondary to chronic nerve entrapment.
Special Tests
Numerous special tests exist in the evaluation of overuse hand and wrist injuries:
The Finkelstein test is a test for de Quervain tenosynovitis and involves adduction of thumb with maximal ulnar deviation of wrist which reproduces symptoms. It has 61% sensitivity and 83% specificity.7
The piano key sign involves the examiner performing a dorsal/volar motion of the distal radius and ulna with the wrist in neutral and compares for instability and pain with the contralateral side. This test is mainly for complete tears of the TFCC. It has a sensitivity of 59% and specificity of 96%.8
Ulna grind test involves passive ulnar deviation with axial loading by the examiner while the wrist is in neutral position. Pain +/− click may indicate a TFCC tear (chronic or acute).
The TFCC shear test or ulnomeniscotriquetral dorsal glide test involves the examiner to stabilize the patient’s radius with one hand and glide the pisotriquetral complex dorsally and the ulna volarly. A positive test is when this maneuver reproduces the patient’s symptoms and indicates a TFCC tear or lesion. This test has a sensitivity of 66%, specificity of 66%, positive predicative value of 58%, and negative predictive value of 69%.9
The Watson shift test for scapholunate dissociation (SLD) involves putting pressure over the scaphoid tubercle while the wrist is brought from ulnar to radial deviation. A painful clunk is felt suggesting a tear of the scapholunate ligament. This test has a sensitivity of 69%, specificity of 66%, positive predictive value of 48%, and negative predictive value of 78%.9
Diagnostic Testing
Laboratory
The majority of overuse hand and wrist injuries in athletes do not require laboratory analysis. If an autoimmune etiology is in the differential diagnosis, then sedimentation rate, C-reactive protein (CRP), antinuclear antibody (ANA), and rheumatoid factor may be considered.
Imaging
The majority of overuse hand and wrist injuries can be diagnosed by a thorough history and physical examination. When the diagnosis remains unclear, an understanding of appropriate diagnostic imaging studies is crucial.
Plain radiographs will often be the first imaging modality utilized in the setting of overuse hand and wrist injuries. Plain radiographs play a crucial role by demonstrating any degenerative changes, occult fractures, or bony abnormalities. Ulnar variance is important to assess in the presence of lateral wrist pain and can be associated with ulnar impaction syndrome as well as TFCC injuries. It is a measurement of the relative length of the ulna with respect to the radius. Neutral variance indicates equal length, with negative ulnar variance indicating shorter ulna and positive variance occurring when the ulna is longer than the radius. The mean ulnar variance is 0.9 mm, measured in posteroanterior (PA) radiograph, with the wrist in neutral supination/pronation. A 2.5-mm increase in positive ulnar variance will increase the load bearing of the ulnocarpal joint from 18% to 42%.
Computed tomography (CT) is generally reserved for evaluation of complex fractures or bone pathology (cysts, tumors, etc.) and rarely required in the setting of overuse wrist and hand pathology.
Magnetic resonance imaging (MRI) is often the test of choice with soft-tissue injuries or when the diagnosis remains unclear. Common indications include fullness in the wrist or palm with a history of slowly progressing neurologic deficit without intermittent fluctuations, point bony tenderness without evidence of fracture on plain radiographs to rule out occult or stress fractures, and ligamentous injuries or chronic wrist pain without specific diagnosis. Occult ganglions, soft-tissue tumors, tendonitis, joint effusions, as well as vascularity of the carpal bones can be accurately visualized with MRI.
Musculoskeletal ultrasound is an excellent modality for many overuse hand and wrist injuries due to the high resolution it provides of superficial soft-tissue structures as well as the dynamic/real-time imaging. Tendonosis, tenosynovitis, tendon nodules (trigger finger), and joint synovitis are common indications that are visualized to a greater degree with ultrasound than on MRI. Musculoskeletal ultrasound’s lack of ionizing radiation and relatively quick scanning time make it a good option for pediatric patients. While used extensively worldwide, musculoskeletal ultrasound’s utilization is currently limited in the United States by the availability of trained operators.
Other Testing
Electromyogram (EMG) studies may be considered in the setting of suspected peripheral nerve injury or cervical spine radiculopathy.
APPROACH TO THE PATIENT WITH DE QUERVAIN DISEASE
de Quervain disease is a tenosynovitis with inflammation in the first dorsal compartment of the wrist involving the APL and EPB, most often at the radial styloid. It is common in sports with repetitive wrist movements (weight lifters, racquet sports, handball). de Quervain disease tends to correlate with other disorders such carpal tunnel syndrome, trigger digits, epicondylitis, and subacromial bursitis, implicating a more systemic and undefined rheumatic process or predisposition. de Quervain has its highest prevalence among women in the fifth and sixth decades of life.10
HISTORY AND PHYSICAL EXAMINATION
There is gradual onset of radial-sided wrist pain exacerbated by ulnar deviation. Patients may complain of associated crepitice. Physical examination is notable for localized tenderness and swelling over the radial styloid as well as pain elicited by stretching of the first dorsal compartment (Fig. 14.5). Finkelstein test with adduction of thumb with maximal ulnar deviation of wrist will often reproduce symptoms and has 61% sensitivity and 83% specificity.7