Athlete with Acute Foot and Ankle Injuries
Daniel Osuch
Nicola DeAngelis
INTRODUCTION
The ankle is a complex joint composed of three bones, stabilized by several ligaments, and traversed by a number of tendons. It is a relatively constrained joint that is subject to complex forces and stresses. As such, it is the most commonly injured joint in the body and prone to a number of acute and chronic conditions that can lead to significant disability if not recognized or treated properly. To that end, this chapter aims to provide a relatively concise understanding of ankle joint anatomy and several commonly encountered injuries. A thorough understanding of these concepts will serve to minimize disability and help to efficiently return athletes to their sports-related activities.
FUNCTIONAL ANATOMY
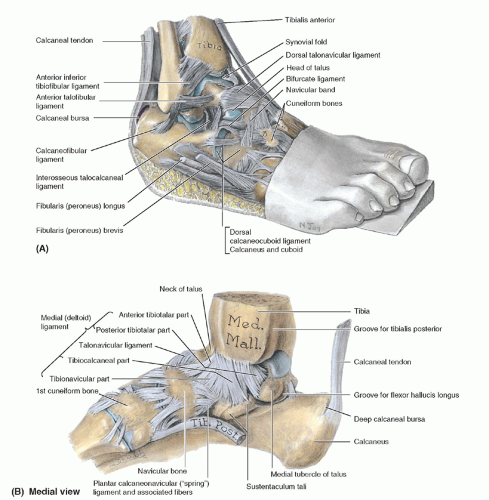
When considering the anatomy of the ankle, it is useful to break the ankle down into its three main components: bony, ligamentous, and musculotendinous. Understanding each of these individually is essential to understanding the ankle as a whole. In its simplest form, the ankle is a hinge joint composed of three bones, the tibia, fibula, and talus, and three ligamentous complexes, the medial, lateral, and syndesmotic. Its anatomic features leave the tibiotalar articulation more rigid medially than laterally, more stable in dorsiflexion than in plantar flexion, and sensitive to minor changes in biomechanical stability. Since the tibiotalar articulation is subjected to more load per unit area than any other joint in the body, understanding these relationships is paramount.1 Three bones compose the ankle joint: the tibia, fibula, and talus. The tibia and fibula form the mortise around the talus (Fig. 21.1). It is important to note that the talus also articulates with the navicular and calcaneus in the foot.
The tibia provides most of the proximal articular surface (plafond) and medial bony constraint (medial malleolus) to the ankle joint. The tibia is the larger of the long bones of the leg and flares distally, where it contributes to the tibiotalar articulation. The plafond is concave when viewed laterally, which accommodates the talar dome. The plafond is also wider medially than laterally and extends further distally posteriorly (the posterior malleolus) than anteriorly. Because of this complex shape, a minimal subluxation of the talus under the tibia can lead to significantly increased contact stresses and predispose to osteoarthritis.2,3 The medial malleolus is found anteromedially in the ankle joint and serves as the attachment site for the deltoid ligaments, an important medial stabilizer. It has two subtle prominences called colliculi: the anterior colliculus, which serves as the attachment point for the superficial deltoid ligament, and the posterior colliculus, which anchors the deep deltoid ligament.
The fibula provides lateral bony stability to the ankle joint. It is the smaller of the long bones of the leg and flares distally to form the lateral malleolus. The lateral malleolus extends more posteriorly and distally than the medial malleolus. It also slopes laterally as it comes to its tip. The medial fibula serves as the attachment point of the syndesmotic ligaments and some of the lateral ankle ligaments. The fibula must also externally rotate and migrate proximally to accommodate the talus in ankle dorsiflexion.
The talus is found distal to the tibia and fibula and within the bony confines of the medial and lateral malleoli. It is composed of three main parts: the body (or dome), neck, and head. Sixty percent to 70% of the talar surface is covered by articular cartilage. The talar body articulates with the tibial plafond and is convex in shape. It is also wider anteriorly than posteriorly, which contributes stability to the ankle in dorsiflexion. Many ligamentous attachments from the malleoli and the subtalar joint serve to anchor the talus in place. Also, since its surface is mostly articular, its blood supply is relatively sparse, leaving the talus prone to avascular necrosis, particularly when the neck is fractured.
The ankle is supported by three sets of ligaments: the medial deltoid ligaments, the lateral ligaments, and the syndesmotic ligaments (Fig. 21.1). Three ligaments make up the lateral ankle ligamentous complex, the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). Since each of these ligaments is under varied tension throughout ankle range of motion, the lateral tibiotalar articulation is somewhat flexible.
Each of these ligaments is also confluent with the ankle joint capsule. The ATFL originates from the anterior lateral
malleolus and inserts on the anterior articular facet of the talus. It provides stability to the ankle when it is plantar flexed and inverted. With the ankle in neutral, the ATFL limits rotation and anterior talar translation. Since it is the weakest of the lateral ankle ligaments, the ATFL is most commonly injured in an ankle sprain. The CFL originates just distal and posterior to the ATFL on the lateral malleolus and inserts posteriorly on the posterior-superior tubercle of the calcaneus. The CFL is taut in neutral and tightens with ankle dorsiflexion. It is susceptible to injury with ankle dorsiflexion and inversion. It also serves to help stabilize the subtalar joint. The PTFL originates on the posterior-medial
lateral malleolus and inserts broadly on the posterior talus. It is very stout, limits dorsiflexion, and is rarely injured. However, with an injured ATFL, the PTFL assumes a larger role in limiting talar internal rotation.
malleolus and inserts on the anterior articular facet of the talus. It provides stability to the ankle when it is plantar flexed and inverted. With the ankle in neutral, the ATFL limits rotation and anterior talar translation. Since it is the weakest of the lateral ankle ligaments, the ATFL is most commonly injured in an ankle sprain. The CFL originates just distal and posterior to the ATFL on the lateral malleolus and inserts posteriorly on the posterior-superior tubercle of the calcaneus. The CFL is taut in neutral and tightens with ankle dorsiflexion. It is susceptible to injury with ankle dorsiflexion and inversion. It also serves to help stabilize the subtalar joint. The PTFL originates on the posterior-medial
lateral malleolus and inserts broadly on the posterior talus. It is very stout, limits dorsiflexion, and is rarely injured. However, with an injured ATFL, the PTFL assumes a larger role in limiting talar internal rotation.
The deltoid ligament confers stability to the medial ankle. It is composed of two portions: the thinner superficial layer, which originates on the anterior colliculus and inserts on the sustentaculum tali and spring ligaments, and the thicker deep layer, which originates on the posterior colliculus and inserts on the medial talus. The deep deltoid ligament is also intra-articular and confluent with the ankle capsule. Both parts of the deltoid ligament limit ankle eversion, but the deep layer is the primary medial stabilizer.4 With lateral ligament injury, the deltoid ligament helps to stabilize anterior and lateral migration of the talus.
There are four syndesmotic ligaments which run between the tibia and fibula, and they are essential to the structural integrity of the ankle. They are the interosseous ligament, anterior-inferior tibiofibular ligament (AITFL), the posterior-inferior tibiofibular ligament (PITFL), and the transverse tibiofibular ligament. The syndesmotic ligaments maintain the relationship between the tibia and fibula throughout the arc of ankle motion and also help prevent excessive external rotation of the fibula when the lateral ankle ligaments are torn and the ankle is dorsiflexed. The most commonly injured syndesmotic ligament is the AITFL. The PITFL serves to deepen the ankle joint. The interosseous ligament is the primary connection between the tibia and fibula and is confluent proximally with the interosseous membrane. Injury to the syndesmotic ligaments generally takes a good degree of force, typically with external rotation. This injury is commonly referred to as a “high ankle sprain” and is considered serious.
A number of tendons cross the ankle joint; several of these contribute to ankle stability (Fig. 21.1). The primary dynamic stabilizers of the ankle are the peroneus longus and brevis, the tendons of which course posterior and inferior to the lateral malleolus below the superior peroneal retinaculum. Both are innervated by the deep peroneal nerve and originate on the lateral fibula. The peroneus brevis inserts on the base of the fifth metatarsal and the peroneus longus courses across the plantar aspect of the foot where it inserts on the base of the first metatarsal and medial cuneiform. They both serve to evert and stabilize the ankle and are important to ankle proprioception (an essential aspect of recovery from ankle injury).
There are a number of other important tendons about the ankle joint. The Achilles tendon runs posteriorly and inserts on the calcaneal tuberosity. It is the primary ankle plantar flexor. The tibialis posterior, flexor digitorum longus, and flexor hallucis longus are found posterior medially and are secondary ankle plantar flexors and inverters. Anteriorly, the tibialis anterior (the primary ankle dorsiflexor), extensor digitorum longus, and extensor hallucis longus also cross the ankle joint.
EPIDEMIOLOGY
Inversion ankle sprains are the most common athletic injury to the ankle. They account for up to 75% of ankle injuries.5 Occurrence rates have been quoted anywhere from 0.68 to 3.85 sprains per 1,000 person-days of exposure.6, 7, 8, 9, 10 Though traditionally considered minor, ankle sprains can lead to significant disability in the athlete.11 These injuries are classified according to severity from grade I through grade III. A grade I injury is consistent with ligament stretching or partial tear. It typically leads to mild tenderness and swelling, minimal functional loss, and no mechanical instability. A grade II injury involves an incomplete ligament tear, leading to moderate pain and swelling with ecchymoses, tenderness to palpation, loss of motion and function, and mild to moderate instability. A grade III injury involves a complete tear and loss of integrity of a ligament, leading to more severe swelling and ecchymoses, loss of function and motion, and mechanical instability on stress testing.12
Though less common than conventional ankle sprains, syndesmotic injuries or high ankle sprains represent a significant injury to the ankle that can result in prolonged disability. These injuries represent approximately 1% of all ankle “sprains.”13 Syndesmotic injuries have gained increasing attention in recent years, because they are often difficult to diagnose and are associated with prolonged recovery compared to conventional ankle sprains, and optimal management is controversial. High ankle sprains occur by an external rotation stress to the ankle that stretches/tears the syndesmotic ligaments, often in the absence of an associated fracture. They can be classified into three categories: sprain without diastasis, sprain with latent diastasis (present on stress x-rays only), and sprain with frank diastasis (present on initial x-rays).14
Ankle fractures are one of the most common skeletal injuries and are increasing in incidence, especially with an aging population.15,16 The incidence of ankle fractures is estimated at approximately 175 per 100,000 persons.17 Risk factors for ankle fractures include increased body mass index and a history of smoking.18 Though most work on ankle fractures has focused on the general population, they are also quite common in athletes. Surgical fixation of ankle fractures is the fifth most common procedure performed on prospective National Football League (NFL) players and the most common form of fracture fixation in this population.19 Improperly managed ankle fractures can lead to significant disability such as posttraumatic arthritis, especially in a young athlete.
Osteochondral lesions of the talus are relatively rare, but since the talus has a tenuous blood supply and limited capacity for healing, these can be devastating injuries to the ankle. These lesions affect the articular cartilage and subchondral bone of the talus and can lead to significant degenerative changes and loss of range of motion.20 They typically arise from previous ankle trauma and should be suspected in patients with chronic ankle pain, especially with previous
injury.21 Fractures of the talar body compose approximately 1% of all fractures and are often unrecognized because they are associated with other more obvious injuries.22 For example, 28% of these lesions have been shown to be associated with other fractures, and some authors estimate that osteochondral lesions accompany up to 6.5% of ankle sprains.23,24 Lesions are generally thought to be split nearly evenly between the medial and lateral talar dome.
injury.21 Fractures of the talar body compose approximately 1% of all fractures and are often unrecognized because they are associated with other more obvious injuries.22 For example, 28% of these lesions have been shown to be associated with other fractures, and some authors estimate that osteochondral lesions accompany up to 6.5% of ankle sprains.23,24 Lesions are generally thought to be split nearly evenly between the medial and lateral talar dome.
Achilles tendon problems represent a spectrum of overuse injuries that are multifactorial in origin and commonly related to poor training practices and advancing age. They represent common ailments, affecting up to 10% of serious runners per year, especially those who have recently stepped up a training program.25,26 The Achilles tendon is the largest tendon in the body and connects the gastrocnemius and soleus muscles to the calcaneal tuberosity. As such, it crosses the knee, ankle, and subtalar joints. During running, forces up to 10 times body weight are imparted on the Achilles tendon. It lacks a synovial sheath and instead has a paratenon, which helps with gliding. The blood supply to the Achilles tendon leaves a relative watershed region approximately 4 cm proximal to its insertion.27 With normal aging, the Achilles tendon undergoes morphologic changes that may leave it susceptible to injury.28 However, a healthy tendon possesses a strong ability to adapt to mechanical stimuli and gradual changes in athletic training. Achilles tendon injuries can be classified according to severity from paratenonitis to paratenonitis with tendinosis to tendinosis to frank rupture.29,30 In paratenonitis, the inflammation is limited to the paratenon and is accompanied by inflammatory signs over the tendon. In paratenonitis with tendinosis, one encounters the beginnings of intratendinous degeneration usually indicated by a palpable nodule in the tendon accompanied by inflammation. Tendinosis involves further intratendinous degeneration indicated by atrophy and palpable tendon nodule without inflammation. Tendinosis typically occurs 2 to 6 cm proximal to the tendon’s insertion and is consistently found in regions of frank tendon rupture.29,30
Lisfranc injuries are a relatively rare, but potentially devastating, athletic injury. The Lisfranc joint is formed by the base of the first and second metatarsal and their articulations with the medial and middle cuneiforms. A stout plantar ligament and less stout dorsal ligament between the medial cuneiform and base of the second metatarsal serve as key supporting elements to the transverse arch of the midfoot. Loss of integrity of this ligament can lead to significant distortion of the architecture of the foot, arthritis, and chronic disability. Injuries to the Lisfranc joint include damage to this ligament, fractures of the bones that comprise this joint, dislocations, or combined injuries. The mechanisms of injury commonly associated with a Lisfranc sprain are axial loading of the midfoot, twisting of the midfoot, and landing on a plantar-flexed forefoot. Lisfranc injuries can occur with most sporting activities, but are particularly common in football, especially with pileups.
Turf toe represents an injury to the forefoot at the base of the first toe. It has become more common in recent years due to the increased use of artificial turf and other relatively hard playing surfaces. Hard surfaces combined with flexible footwear that provides less forefoot stability when running and jumping have been thought to be the prime contributors to turf toe. This injury represents damage to the plantar capsule of the first-toe metatarsal-phalangeal joint. Capsular damage can be quite painful and can even lead to joint instability. Patients typically complain of pain at the base of the first toe, stiffness, and swelling. Turf toe is particularly common in sports that require running and jumping on artificial turf such as football, soccer, and lacrosse.
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
One of the most useful tools in evaluating a complaint of ankle pain is the patient’s history. Factors to consider include the patient’s age, mechanism of injury, location of pain, exacerbating and alleviating factors, associated symptoms, and past medical history.
The patient’s age is a key factor when evaluating ankle pain. Children often have ankle pain as a result of trauma. Children are also more likely to suffer avulsion fractures, as their apophyses are relatively weaker than their tendons and ligaments. A history of chronic ankle sprains in a child aged 10 to 15 years should raise the concern for a tarsal coalition. Children can also develop primary bone or soft-tissue tumors. Acute trauma is the most likely cause of ankle pain in young adults. This includes sprains, fractures, tendon injuries, and osteochondral lesions of the talus. Middle-aged adults, especially the “weekend warrior” types, commonly suffer Achilles tendon injuries, sprains, and fractures. Fractures are becoming increasingly common in osteoporotic elderly individuals. Chronic conditions such as osteoarthritis, inflammatory arthritis, posterior tibial tendon dysfunction, and metastatic neoplasms must be considered in the elderly population as well.
Another key feature of the patient’s history with ankle pain is the mechanism of injury. Typically, an inversion injury to the ankle results in a sprain. An external rotation injury commonly results in fracture and/or syndesmotic injury. A sudden eccentric contraction of the Achilles tendon accompanied by a pop is common in rupture of this tendon. Fall from a height is commonly associated with hindfoot fractures or fractures of the tibial plafond. More insidious mechanisms and gradual onset of pain suggest chronic conditions such as osteoarthritis, inflammatory arthritis, or neoplasm. The relatively sudden onset of pain in the setting of a fever or other infectious process is concerning for septic arthritis, a surgical emergency. Pain that occurs with discrete periods of exacerbations and remissions is common with
chronic ankle instability and osteochondral lesions of the talus. Night pain is especially concerning for a neoplastic process.
chronic ankle instability and osteochondral lesions of the talus. Night pain is especially concerning for a neoplastic process.
The location of ankle pain can also help narrow the differential diagnosis. Pain along the dorsum of the foot, especially if lateral, is typical with ankle sprains. Pain directly over one or both malleoli is associated with fracture and/or ligament injury. Posterior ankle pain is commonly seen with Achilles tendon or hindfoot injury. Diffuse, deepseated ankle pain is common with the different forms of arthritis. Pain distal to the lateral malleolus or along the lateral border of the foot is common with peroneal tendon instability.
Many ankle conditions have exacerbating and alleviating factors. Pain with weight bearing is common in acute trauma. Typically, there is more difficulty with weight bearing in the setting of a fracture than in the setting of a sprain. The pain associated with inflammatory arthritis is commonly worse early in the day and relieved by anti-inflammatory medications. The pain with osteoarthritis is typically worse with weight bearing, worsens as the day progresses, and responds to anti-inflammatory medications. Pain that does not respond to ice and elevation is concerning for an infectious process. Although pain with range of motion is typical with most ankle processes, the pain with a septic joint is usually markedly worse than that seen with osteoarthritis or inflammatory arthritis.
The patient’s past medical history is especially important to consider when evaluating ankle pain. A history of multiple sprains can lead to chronic ankle instability. Multiple sprains are also concerning for a tarsal coalition, particularly in a teenager or young adult. A history of trauma makes posttraumatic osteoarthritis a concern. A previous ankle infection or a history of bacteremia makes a septic joint more likely. Metastatic disease should be considered if the patient has a history of neoplasm. One should consider gout or another inflammatory arthritis if the patient has had previous exacerbations. Diabetics or patients with neuropathy are particularly prone to developing a Charcot joint, as their lack of protective sensation predisposes them to repeat injury.
Evidence-based Physical Examination
Inspection
The examination of the ankle begins with visual inspection. Compare the symptomatic ankle with the unaffected contralateral ankle, as this can give a nice approximation of the baseline appearance of the symptomatic ankle. Observe the affected ankle from midtibia down to the foot. Be sure to look at the bony and tendinous prominences for evidence of cutaneous trauma and/or swelling. Localized swelling serves to help determine the area(s) of maximal injury. Examples of common areas of localized swelling include the anterior/lateral ankle and proximal dorsal foot for ankle sprains, the malleoli for fractures, and just proximal to the ankle for syndesmotic injuries. Generalized foot/ankle swelling suggests more severe trauma. Bruising and other color changes can help to assess the chronicity of the injury as well. It is also useful to assess the patient’s gait and weight-bearing ability to help narrow the potential area(s) of injury/pain. Assessment of overall alignment, especially compared to the contralateral ankle, is also important.
Palpation
Palpate the ankle to assess the various areas of bony anatomy and ligament and tendon origin and insertion. A consistent systematic approach is advised. Palpate the prominent medial malleolus and distal tibia medially. Moving toward the plantar aspect of the foot, palpate the medial talus as well as the prominent sustentaculum tali of the calcaneus. The medial tubercle of the talus is also palpable just posterior to the medial malleolus. The deltoid ligament is palpable as a firm band just inferior to the medial malleolus. Posterior to the deltoid ligament in a soft spot anterior to the Achilles tendon lay the tibialis posterior tendon, flexor digitorum longus tendon, posterior tibial artery and nerve, and flexor hallucis longus tendon. Moving posteriorly, palpate the Achilles tendon down to its insertion on the calcaneus. Laterally, start with bony palpation of the lateral malleolus. Palpation of the proximal/lateral foot includes the prominence of the base of the fifth metatarsal. The peroneal tendons are palpable, tracing back proximally from the base of the fifth metatarsal inferior and lateral to the distal fibula. The lateral ligamentous structures are more difficult to palpate, but tenderness anterior/distal to the lateral malleolus suggests ATFL injury. Similarly, tenderness posterior/medial to the lateral malleolus suggests PTFL or CFL injury. Anterior and medial to the lateral malleolus is a soft area often referred to as the sinus tarsi. In addition to the ATFL, it is also possible to palpate the tibiofibular articulation and dome of the talus in this area. Further anteriorly, palpate the prominent tibialis anterior tendon. Just lateral to this tendon on the dorsum of the foot is the dorsalis pedis artery.
Range of Motion
Range of motion of the ankle can be simplified to plantar flexion and dorsiflexion (which primarily occur through the tibiotalar joint) and inversion and eversion (which primarily occur through the subtalar joint). Passive range of motion is most easily assessed with the patient sitting with the legs dangling over the side of the table. Assess ankle range of motion with the knees bent because the gastrocnemius crosses both the ankle and knee joints. It is important to stabilize the subtalar joint by holding the calcaneus when assessing plantar flexion and dorsiflexion. While grasping the midfoot/forefoot with the other hand, one can assess plantar flexion and dorsiflexion, which averages 50 and 20 degrees,
respectively. The shape of the talus leaves the ankle with more medial and lateral motion in plantar flexion than in dorsiflexion. A decrease in range of motion can be caused by prolonged immobilization (e.g., casting), intra- or extraarticular swelling, joint fusion, joint capsule contracture, or impingement due to osteophyte formation seen with osteoarthritis. A loss of dorsiflexion is particularly debilitating because it can lead to difficulty clearing the floor with the toes during the swing phase of gait, which can cause frequent stumbles and/or falls. Assessing subtalar motion through inversion and eversion requires stabilizing the tibia with one hand and using the contralateral hand to hold the calcaneus and hindfoot. There is usually 5 degrees each of subtalar inversion or eversion. Decreased inversion and eversion is seen in conditions such as osteoarthritis, joint fusion, and tarsal coalition. A loss of inversion and eversion makes it particularly difficult to walk on uneven surfaces. Active range of motion can be assessed with the patient sitting as above or standing. Asking the patient to stand/walk on the toes, heels, lateral foot, or medial foot assesses ankle plantar flexion, dorsiflexion, and subtalar inversion and eversion, respectively.
respectively. The shape of the talus leaves the ankle with more medial and lateral motion in plantar flexion than in dorsiflexion. A decrease in range of motion can be caused by prolonged immobilization (e.g., casting), intra- or extraarticular swelling, joint fusion, joint capsule contracture, or impingement due to osteophyte formation seen with osteoarthritis. A loss of dorsiflexion is particularly debilitating because it can lead to difficulty clearing the floor with the toes during the swing phase of gait, which can cause frequent stumbles and/or falls. Assessing subtalar motion through inversion and eversion requires stabilizing the tibia with one hand and using the contralateral hand to hold the calcaneus and hindfoot. There is usually 5 degrees each of subtalar inversion or eversion. Decreased inversion and eversion is seen in conditions such as osteoarthritis, joint fusion, and tarsal coalition. A loss of inversion and eversion makes it particularly difficult to walk on uneven surfaces. Active range of motion can be assessed with the patient sitting as above or standing. Asking the patient to stand/walk on the toes, heels, lateral foot, or medial foot assesses ankle plantar flexion, dorsiflexion, and subtalar inversion and eversion, respectively.
Strength Testing
Strength testing about the ankle involves assessing the function of the main ankle dorsiflexor and inverter (tibialis anterior), plantar flexors (gastrocsoleus complex), and everters (peroneus longus and brevis). Strength testing is a nonspecific test that examines musculotendinous integrity, intact neurologic function, and the ability to move a joint. It is important in assisting the evaluation of the cause of a patient’s complaint. To assess the tibialis anterior, observe the patient walking on his/her heels and resist dorsiflexion/inversion by stabilizing the tibia and pushing the foot into plantar flexion/eversion by pressing on the first metatarsal. As mentioned earlier, a weak tibialis anterior and loss of ankle dorsiflexion make it difficult to clear the floor with the toes during swing phase of gait and can contribute to a steppage or drop foot gait. To assess the gastrocsoleus complex, observe the patient walking on his/her toes, hopping up and down on one foot, and resisting plantar flexion by stabilizing the tibia with one hand and pressing up on the dorsum of the foot with the contralateral hand. Weakness with plantar flexion may suggest Achilles tendon injury/inflammation. To assess the peroneus longus and brevis, observe the patient walking on the medial border of the foot and resisting eversion by stabilizing the calcaneus with one hand and providing an inversion/plantar flexion force with the other hand pressing along the fifth metatarsal. Pain with resisted eversion or inability to evert the foot suggests derangement of the peroneal tendons such as tendonitis, sprain, or subluxation. There are also a number of tests to assess the other musculotendinous structures that cross the ankle joint, but these perform a secondary function with ankle joint motion and are not covered in this chapter.
Laxity Tests
A number of different maneuvers are designed to assess the various structural elements of the ankle for stability.31 One such test is the talar tilt test, which assesses the integrity of the ATFL and CFL. It is performed with the patient seated and the foot unsupported. With the foot in 10 to 20 degrees of plantar flexion (which tests the ATFL primarily), stabilize the leg just above the medial malleolus and supply an inversion force to the hindfoot with the contralateral hand. Normally an angle of approximately 5 degrees is achieved between the tibial plafond and talar dome. An increase in this tilt is suggestive of injury to both the ATFL and CFL. However, there is a lack of consensus on just how much talar tilt is indicative of injury to both ligaments. Comparison to the contralateral ankle is useful in this circumstance.32, 33, 34
Another test useful for assessing the integrity of the ATFL is the anterior drawer test. This test can be performed with the patient either sitting or supine. In the sitting position, have the knee flexed over the side of the table and let the ankle fall into plantar flexion. Stabilize the distal tibia with one hand and provide an anteriorly directed force on the calcaneus with the other. If the patient is supine, hyperflex the knee, place the ankle in plantar flexion, fix the foot in one hand (or against the table), and apply a posteriorly directed force to the anterior aspect of the distal tibia. This is often called the modified anterior drawer test.35 A positive test involves pain and/or translation of 8 mm or greater compared to the contralateral side. In a study comparing physical examination to surgical and arthrography findings, the anterior drawer test was found to have a positive predictive value of 91% and a negative predictive value of 51%, with a sensitivity of 80% and specificity of 74%.36
Special Tests
Two tests are commonly cited for assessment of injury to the syndesmosis. The first of these is often called the squeeze test, which is performed by squeezing the fibula against the tibia at the midcalf level. A positive test produces pain distally at the level of the syndesmosis just proximal to the ankle joint and indicates severe syndesmotic injury. This test has shown moderate interrater reliability.13,37 The second test is the external rotation test. In this test, the tibia is stabilized and the foot externally rotated through the ankle joint, thereby stressing the syndesmosis. A positive test causes pain at the level of the syndesmosis in the setting of syndesmotic ligament injury. This test has demonstrated high interrater reliability and significant association with ankle pathology.37,38
If the patient has lateral ankle pain, especially with a sensation of popping, it is important to test for peroneal tendon subluxation. This occurs with loss of superior peroneal retinaculum integrity. To perform this test, have the patient further dorsiflex the ankle from a position of slight dorsiflexion and eversion. A positive test recreates the popping
sensation and may allow visual observation or palpation of the tendons actively subluxing.
sensation and may allow visual observation or palpation of the tendons actively subluxing.
Another test to consider when evaluating ankle pain is the Thompson test for a ruptured Achilles tendon. This test is performed with the patient prone and both feet extending past the end of the table. Squeezing the calf muscles should produce plantar flexion of the ankle if the tendon is intact. The foot should not plantar flex if the tendon is ruptured. This test was found to have a positive predictive value of 98%, with a 96% sensitivity and 93% specificity.39 False positives may be present if the secondary ankle plantar flexors remain intact.
Diagnostic Testing
Laboratory
Laboratory studies are not commonly obtained in the setting of acute ankle injury. If there are concerns for infectious or inflammatory arthritis, obtaining a white blood cell count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and uric acid level is suggested. Specific markers for inflammatory disease such as rheumatoid factor or antinuclear antibody should also be considered. A Lyme titer should also be considered, given the appropriate history and demographic considerations.
Imaging
One of the best-studied areas in evaluating ankle pain surrounds whether or not to obtain plain x-rays. In the setting of acute injury, the Ottawa ankle rules have proven to be nearly 100% sensitive for detecting clinically significant ankle fractures while reducing the need for x-ray by 30% to 40%.40,41 The Ottawa ankle rules suggest that ankle x-rays are indicated if there is tenderness over the inferior or posterior pole of either malleolus, including the distal 6 cm, or if there is the inability to bear weight (four steps taken independently, even if limping) at the time of injury and at the time of evaluation. If there is tenderness over the base of the fifth metatarsal or navicular bone, foot x-rays are indicated. X-rays should also be considered in the setting of more chronic ankle pain to evaluate for degenerative changes, osteochondral lesions, or the possibility of neoplasm.
A typical x-ray series of the ankle involves three views: the anteroposterior (AP), mortise, and lateral. On each view, a systematic approach should be employed, looking at all visualized bone and spaces between bones, especially sites of ligament/tendon attachment and joint surfaces. The AP radiograph is taken in the long axis of the foot. Areas of particular importance on the AP radiograph include the tibiofibular clear space and tibiofibular overlap. A clear space of less than 5 mm and an overlap of greater than 10 mm indicate a normal syndesmotic relationship. The mortise radiograph is taken with the foot in 15 to 20 degrees of internal rotation so that the x-ray beam is perpendicular to the intermalleolar line. On a well-taken mortise x-ray, there should be a universal amount of clear space around the talus and minimal overlap of the tibia and fibula. An increase in the clear space, especially greater than 4 mm medially, suggests lateral talar shift and either medial ligamentous or syndesmotic injury. Talar tilt can be assessed on the mortise x-ray by drawing lines parallel to the tibial plafond and talar articular surface. These lines should be parallel, and greater than 2 degrees of angulation indicates talar tilt. Another important aspect of the mortise view is the talocrural angle. This angle is formed by a line drawn from the tip of one malleolus to the other and a line drawn parallel to the tibial plafond and usually measures 8 to 15 degrees. A smaller angle suggests fibular shortening. Lastly, less than 1 cm of tibiofibular overlap and greater than 1 mm of talar shift are considered abnormal on the mortise view. The final view in an ankle series is the lateral view. On this view, the dome of the talus should be centered under the tibia and congruous with the tibial plafond.16
Computed tomography (CT) scans are useful in the 3-dimensional evaluation of bony structures. The use of CT scan is fairly limited in the evaluation of acute ankle pain. CT scan may reveal a tarsal coalition or an osteochondral lesion of the talus that is not appreciated on plain x-ray. CT is also useful to delineate complex fracture patterns or complex bony anatomy for preoperative planning purposes.
Magnetic resonance imaging (MRI) scans are another means of obtaining 3-dimensional information about the ankle. MRI is useful in assessing soft-tissue injury or bony edema about the ankle. MRI is often indicated in the setting of pain or disorders refractory to conservative therapy. MRI has traditionally been used in the evaluation of chronic conditions, but has become increasingly more common in the setting of acute injury. Indications for MRI in acute ankle injury are still being worked out. MRI should be considered when working up suspected Achilles tendon injury, chronic ankle instability, osteochondral lesions of the talus, stress fractures, or peroneal tendon subluxation as outlined in the sections that follow. MRI is also useful in the evaluation of infectious processes. An MRI may also be considered in the evaluation of a potential neoplastic process.
Other Testing
An aspiration of the ankle joint may be considered to help distinguish inflammatory from infectious arthritis. The aspirate should be sent for cell count, Gram stain, culture and sensitivity, and crystal analysis. An ankle aspiration is most easily performed by directing a needle posterior laterally in the soft spot found just lateral to the medial malleolus and medial to the tibialis anterior tendon.
Ultrasound is also of limited utility in evaluating ankle pain. The main indication for ultrasound exists in the dynamic evaluation of a suspected Achilles tendon rupture
to assess if the tendon ends reapproximate or not with ankle plantar flexion. Ultrasound is relatively quick and inexpensive, but carries a steep learning curve for those performing and interpreting the test.
to assess if the tendon ends reapproximate or not with ankle plantar flexion. Ultrasound is relatively quick and inexpensive, but carries a steep learning curve for those performing and interpreting the test.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree