Athlete with Peripheral Nerve Injuries
Faren H. Williams
INTRODUCTION
Peripheral nerve injuries in athletes may serve as a diagnostic challenge for the treating clinician. They may present as acute injuries or secondary to overuse. Athletes are vulnerable due to the repetitive nature of upper- and lower-extremity movements and the superficial nature of peripheral nerves.
Peripheral nerve injuries can be underestimated in athletes due to the relative muscle hypertrophy and enhanced strength that can mask the extent of the injury. Additionally, sensory changes may not be appreciated to the same extent by athletes who are accustomed to playing with some degree of pain or discomfort. A high degree of suspicion along with an understanding of common peripheral nerve injuries in athletes will greatly enhance the proper diagnosis and treatment. Additionally, an understanding of dermatomes and peripheral nerve sensory as well as motor function is essential in differentiating peripheral nerve injuries from more central etiologies. This chapter will review the most common nerve injuries associated with different sports and address when to refer the patient for specialty electrodiagnostic consultation.
FUNCTIONAL ANATOMY
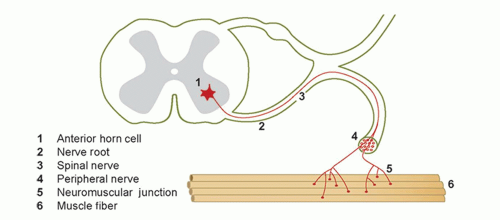
The peripheral nervous system (PNS) consists of the nerve root, the motor efferent from the anterior horn cell, the afferent sensory ganglion (usually in the neural foramina) which combines to form a spinal nerve, along with sensory and motor components. The ventral rami from these nerves coalesce to form the brachial plexus in the upper extremity and lumbosacral plexus in the lower extremity, forming trunks, divisions, and cords, which ultimately become terminal nerve branches supplying the arms or legs with motor and sensory function (Fig. 23.1).1
PATHOPHYSIOLOGY
Peripheral nerve injuries are most commonly classified according to Seddon’s scheme.2 The terms neuropraxia, axonotmesis, and neurotmesis are used by electromyographers (Table 23.1).
The mildest injury, neuropraxia, has the best prognosis for recovery, with the neurotmesis having the worst prognosis, given the disruption of axons and epineurium. The latter problem may require surgical repair by a skilled peripheral nerve surgeon, with outcomes often guarded, although the surgical approximation of nerve fibers is improving.3
There are different degrees of axonal loss, with prognosis dependent on many factors, including the age and health of the patient, the proximity of the lesion to the muscle(s) being innervated, and the integrity of the muscle itself. In general, upper-trunk brachial plexopathies have a better prognosis than lower-trunk ones, because of the length of axonal regeneration needed for the latter.4
EPIDEMIOLOGY
Of 1,167 peripheral nerve injuries seen in a single orthopaedic clinic in Japan over 18 years, 5.7% were attributed to sports and 10% of them to traumatic nerve injuries.5 Because the upper extremities are more mobile, with muscle attachments directly to the thorax, the peripheral nerves are vulnerable to injury to a greater extent than in the lower extremities. In a retrospective review of peripheral nerve injuries to athletes, 88% were to the upper extremity, with one third of the injuries being related to playing football.6 Mechanisms for nerve injury include compression, traction, ischemia, and laceration, secondary to hyperextension of the neck or limbs, or unstable fractures or dislocations.7
In general, football and other contact sports such as wrestling, hockey, and basketball contribute to the majority of upper-extremity plexus injuries, while overhead throwing sports such as volleyball result in more focal nerve injury, such as the suprascapular nerve, at the sphenoglenoid notch, affecting primarily the infraspinatous muscle. Weight lifting, while a sport by itself, is also a significant part of the training program for most sports, so it can be the etiology for nerve injuries in many athletes playing different sports.8
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
The most important part of the peripheral nerve diagnosis is the patient’s history of the present symptoms and the timing of any preceding trauma. Athletes may note gradually progressive weakness or atrophy after an acute injury such as a shoulder dislocation. Overuse peripheral nerve injuries may, however, present with no history of trauma but gradual-onset pain, weakness, and/or atrophy.
Athletes, especially as they age, may have underlying medical conditions such as diabetes and its associated peripheral neuropathy. Athletes with persistent numbness in the hands and feet may have a peripheral neuropathy or cervical or lumbar stenosis. Neck and upper-extremity symptoms may be alleviated by cervical traction, either manually or with weight. With lumbar stenosis, the symptoms will be exacerbated by walking or running and relieved by sitting. If there is radiation of pain into only one extremity, the athlete may have a radiculopathy from a herniated disc. Pain from this is usually worse with sitting and to a lesser extent standing; walking may relieve this type of pain.
Evidence-based Physical Examination
A thorough review of the neurologic examination is detailed below. Some common neurologic tests utilized to differentiate potential peripheral nerve injury from a central etiology include the Tinel’s and Phalen’s tests along with the Spurlings test. The Tinel’s sign involves percussion of a peripheral nerve to recreate the patients’ dysthesias or paresthesias. This is most often performed at the wrist for the median nerve but can be done at the elbow for the ulnar nerve, at the tarsal tunnel for the posterior tibial nerve, and at the proximal fibula for the peroneal nerve. The sensitivity and specificity of the Tinel’s sign is less than 50%, so it is not diagnostic for a nerve injury, and does not correlate well with nerve conduction studies (NCSs). Sensory testing of dermatomes and peripheral nerves, motor strength testing, and reflexes are more reliable tests.4
TABLE 23.1 Seddon’s Classification of Nerve Injuries | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
A detailed and thorough neurologic examination is warranted after a significant injury on the playing field or when the athlete presents with a suspected nerve injury. More concerning are injuries that compromise the central nervous system, which includes the spinal cord. Any athlete who has decreased motor and sensory function needs prompt evaluation, keeping in mind that a cervical injury that causes mainly symptoms in the upper extremities can be a central cord syndrome versus a cervical root or brachial plexus injury. Reflexes in a spinal cord patient acutely may be diminished due to spinal shock and become more hyperactive over time.9
Other common peripheral nerve injuries are cervical and to a lesser extent lumbar radiculopathies from an intervertebral disc applying pressure to a nerve root. While they may involve primarily motor function, the sensory dorsal root
ganglion can also be compromised in lesions that are more lateral. In these patients, the associated reflexes should be diminished compared with the contralateral side, and any sensory changes should follow a dermatomal distribution. Injuries that affect sensory may be distal to the dorsal root ganglion at the level of the brachial plexus.
ganglion can also be compromised in lesions that are more lateral. In these patients, the associated reflexes should be diminished compared with the contralateral side, and any sensory changes should follow a dermatomal distribution. Injuries that affect sensory may be distal to the dorsal root ganglion at the level of the brachial plexus.
The term “stingers” or “burners” is used for acute traction injuries involving the brachial plexus. Diminished reflexes and subjective sensory changes, not always objective ones, in a portion of the brachial plexus are detected on physical examination. Sensory changes may be loss of position and vibratory sensation and light touch, associated with conduction block of large myelinated fibers. Detailed examination of motor, sensory (dermatomal and peripheral nerve), and reflexes is key in helping to localize the lesion, but may be compromised in athletes who have a concomitant brain injury, which affects their ability to participate in the examination and may cause hyperreflexia. In athletes who have peripheral nerve injuries, up to 60% may have a traumatic brain injury.10
Diagnostic Testing
Laboratory
In the setting of an acute peripheral nerve injury, laboratory studies are rarely needed. For gradual-onset symptoms, appropriate laboratory studies may be indicated to differentiate systemic or metabolic etiology from a focal nerve injury. Complete blood count (CBC), thyroid studies, rapid plasma reagin (RPR), B12, and folate are some common tests obtained. Other serology and cultures are ordered based on clinical presentation and pretest probability.
Imaging
Appropriate radiographs are indicated in cases of trauma to rule out coexisting fractures that may be associated with peripheral nerve injuries (i.e., supracondylar fractures, proximal fibula fracture, displaced or open fractures). CT may better define complex fractures and bone fragments that may be associated with traumatic peripheral nerve injuries.
MRI may play a role in visualization of potential nerve injury from both acute or overuse mechanisms. The superiority of MRI for visualization of soft tissue may be of help for visualization of mass effect along with potential visualization of the nerve itself, although a specialized MRI neurography is needed for more useful information about the nerve.
Ultrasound is growing in use for visualization of peripheral nerves due to its high resolution of superficial soft-tissue structures and its ability to visualize nerve inflammatory changes. The dynamic capabilities of ultrasound can identify conditions of nerve subluxation as can occur at the elbow with the ulna nerve. Ultrasound, however, is operator dependent, and availability is affected by access to trained individuals who understand the applications of ultrasound to peripheral nerve problems.
Other Testing
Electrodiagnostic studies can play a significant role in the diagnosis and prognosis of peripheral nerve injuries,4 as they can assist further with prognosis. Information obtained about the integrity of the affected nerve(s) can be used to prescribe a therapeutic treatment program. Changes in amplitude occur in the motor nerve after 6 to 8 days, and the sensory nerve in 8 to 12 days; therefore, NCSs done within 1 to 2 weeks after a traumatic injury can determine whether there has been some nerve injury. Other changes with the needle electromyography (EMG) will take 3 to 4 weeks to evolve and are more suggestive of axonal loss.11 This information about the integrity of the affected nerve(s) can be used to prescribe an appropriate therapeutic treatment program. Denervated muscle cannot be strengthened, and exercises need to focus initially on maintaining the range of motion about the involved joint.
Electrodiagnosis is quite specific in the hands of a skilled electromyographer, with specificity greater than 90%.12 The electrodiagnostic results should complement the clinical history and physical examination. When inconsistencies are seen, one needs to question whether affected nerves were compared to similar ones on the contralateral limb, whether the athlete has a different underlying medical condition, or whether the electrodiagnostic study was thorough and technically competent.4 One should refer patients to someone who does a complete electrodiagnostic consultation, interpreting electrodiagnostic results in the context of the patient’s history, physical examination, and other pertinent studies such as imaging.13
Electrodiagnosis
A basic understanding of this test, what it does and does not measure status post nerve injury, helps in determining when to order it. It evaluates the large myelinated (type A) peripheral nerve fibers and is useful only with injuries to these nerves, not the smaller type C pain fibers. There are two different types of electrodiagnostic testing: (1) motor and sensory NCSs and (2) needle EMG, which analyze motor units and denervation potentials seen in selected muscles after injury to the nerve innervating them.
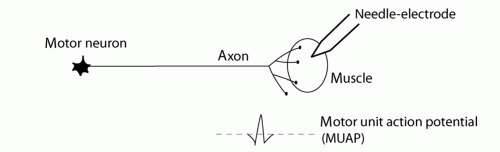 FIG. 23.3. Normal motor unit action potential (MUAP). Electrode records MUAPs from muscle fibers within the vicinity of the needle. |
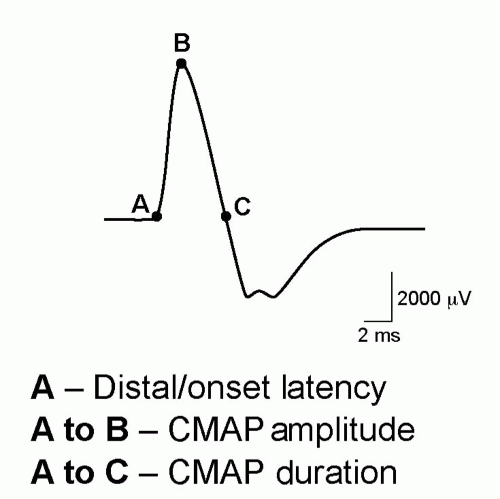
To perform NCSs, the peripheral nerve motor axons are stimulated electrically, causing depolarization of the muscles innervated by that nerve. By placing a recording electrode over the muscle, a compound motor action potential (CMAP) is visualized, with characteristic amplitude(s) and duration(s) for particular muscles (Fig. 23.2). Stimulation of the sensory axons results in a comparable sensory nerve action potential (SNAP). These responses are a composite of the motor or sensory fibers picked up by the recording electrodes. The motor result can be affected by neuromuscular junction problems and significant muscle atrophy or disease such as myopathies, but the sensory reflects direct nerve transmission and is usually seen before the motor response. Changes in the amplitude may suggest some axonal loss, and changes in the speed of conduction, or latency, may reflect slowing of conduction, associated with demyelination.4
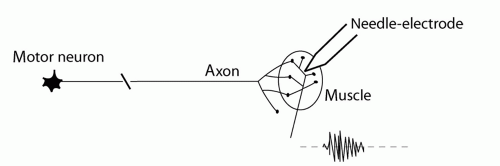
Needle EMG is performed by inserting a needle directly into a muscle and recording motor unit action potentials (MUAPs) from the muscles in the vicinity of the needle (Fig. 23.3). Different muscles have characteristic amplitudes and durations, which indicate whether the potential is a motor unit.
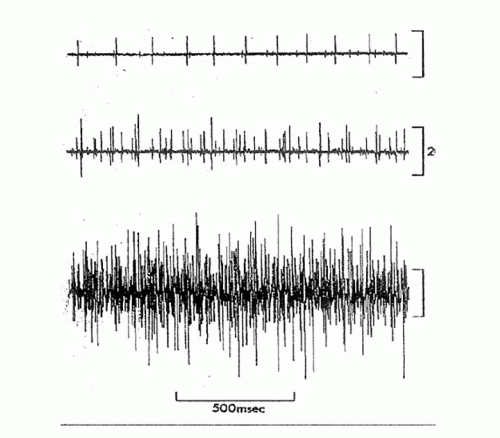
Other potentials (fibs and positive waves) referred to as spontaneous activity are recorded from muscles that have sustained denervation of their nerve axons secondary to Wallerian degeneration. Normal muscle is electrically silent at rest, so this spontaneous activity at rest suggests nerve injury. Fibs and positive waves may be graded on a 1 to 4 scale depending on their prevalence with needle testing, but any axonal loss produces fibs and positive waves. Therefore, this rating does not correlate with degree of axonal loss; only the amplitude of the CMAP is proportional to the degree of axonal loss.14
Another EMG parameter is recruitment, or the extent to which more axons can fire in response to increasing muscle contraction. Recruitment is full and spontaneous when axonal integrity is preserved but becomes more limited as axons degenerate.15 Decreased recruitment is often the first finding on needle EMG, suggesting axonal disruption, but should be used together with evidence for fibs and positive before commenting on whether there is evidence for acute axonal loss/denervation (Fig. 23.4). Nerves have the capacity to regenerate (1 in/month),4 and over time the fibs and positive waves become smaller or disappear.16 The MUAPs may have multiple phases, suggesting that immature axons are conducting at different rates, but as axons mature, the number of phases may decrease. These findings may suggest some reinnervation (Fig. 23.5).4
The changes in NCSs or needle EMG are dependent on the type of injury and time from injury. These tests will help confirm a peripheral nerve injury, the one suspected or a different one(s), and are also of benefit in explaining a different etiology for the patient’s pain and muscle atrophy/weakness. One limitation of early electrodiagnostic testing is the limited prognostic value, as there may not have been enough time for neurophysiologic changes to evolve. Unfortunately, a competitive athlete may not want to wait until the extent of neurologic involvement can be ascertained.
APPROACH TO THE ATHLETE WITH STINGER/BURNER
Brachial plexus injuries are some of the more prevalent sports injuries commonly encountered in football, wrestling, hockey, basketball, baseball, and overhead throwing sports. They are transient injuries to the brachial plexus, resulting in unilateral symptoms of numbness, tingling, burning, and weakness. The primary mechanisms are forced hyperextension and lateral bending/flexion of the neck to the opposite side with downward displacement to the ipsilateral shoulder, which causes a traction-type injury to the brachial plexus. The alternative mechanism can be a forced flexion to the affected side with compression of the brachial plexus (Fig. 23.6). Younger players may be at risk because they have more mobile necks and less well-developed neck musculature.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree