Athlete with Overuse Foot and Ankle Injuries
Jeremy McCormick
INTRODUCTION
With increasing participation in athletics, foot and ankle injuries are becoming more prevalent. While many injuries occur with an acute incident, others are the product of repetitive stress or overuse. With these types of injuries, patients develop symptoms slowly over a period of several weeks or months. In some situations, the athlete cannot recall a specific incident, but presents because of dull pain or discomfort that has lingered for some time without improvement. The duty of the physician is to assess, diagnose, and treat these injuries as expeditiously as possible so that the athlete can return to play quickly, without compromising the healing or recovery process.
This chapter reviews some of the more common overuse foot and ankle injuries. Patients can fully recover from all of these injuries if they are properly diagnosed and treated in the early stages of their disease process. It is our hope that by reviewing these injuries with their classic signs, symptoms, and treatment regimens, an athlete will be well served with early intervention and a path toward recovery that enables full participation in return to their sport.
FUNCTIONAL ANATOMY
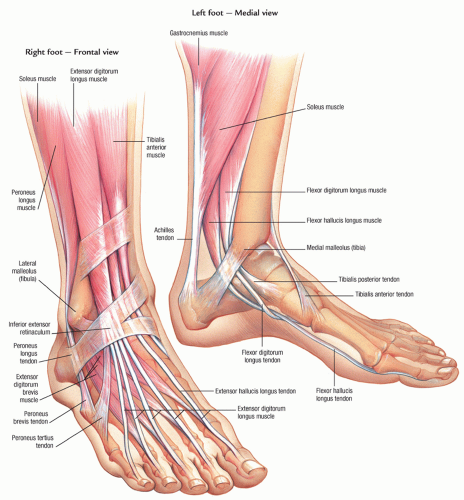
The anatomy of the foot and ankle can be very involved, and a whole chapter might be dedicated to its finest detail. However, a working knowledge of the anatomy of this region of the body is critical to proper examination and diagnosis of chronic injuries. The bony structures of the foot are divided into regions called the forefoot (phalanges, metatarsals), midfoot (cuneiforms, cuboid, navicular), and hindfoot (calcaneus, talus), and there are named joints between all of these bones (Fig. 20.1).
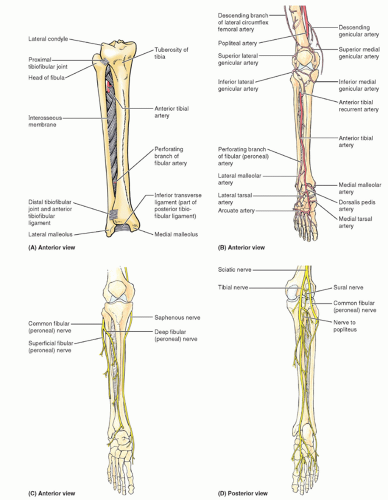
Additionally, there are numerous muscular structures intrinsic to the foot and tendons that pass across the ankle, with origin in the lower leg. Crossing on the lateral aspect of the ankle are the peroneal tendons and crossing on the medial aspect are the posterior tibialis, flexor digitorum longus, and flexor hallucis longus tendons (Fig. 20.2).
The primary nerve supply for intrinsic function in the foot comes from the tibial nerve, which passes medially and branches just beyond the ankle. There are also the deep and superficial branches of the peroneal nerve, the sural nerve, and the saphenous nerve, which all cross the ankle and enter the foot. The main vascular supply to the foot comes from the dorsalis pedis and posterior tibialis arteries (Fig. 20.3).
Within each section of this chapter, the anatomy, as it pertains to a specific chronic foot and ankle injury, is explained in greater detail.
EPIDEMIOLOGY
Millions of people play football, soccer, basketball, and baseball, and some studies have shown that up to 40% of athletes may suffer some type of foot or ankle injury during their participation in these sports.1 With that in mind, it is important to be aware of the different injuries that can exist, particularly when patients present with chronic complaints. These can be more challenging in that the complaints might be vague and there may not be a discrete source of pain. The differential diagnosis for any presenting complaint of foot or ankle pain can be broad, but with a careful history and physical examination, the list can be narrowed. The subsequent sections on specific etiologies of chronic foot and ankle injuries will help in their diagnosis and subsequent treatment and help sports physicians accurately and expeditiously treat their patients.
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
A careful history should include questions characterizing the complaint. Information such as the mechanism of injury can be extremely useful. One should also determine the severity of pain, quality of pain, location of pain, timing of pain, onset of pain, and the alleviating or exacerbating factors. It is also important to determine if a patient has ever experienced or been treated for the pain in the past. While in some measure, patients of certain age groups or activity profiles are more
predisposed to an injury, a physician should not limit themselves when investigating a patient’s complaints.
predisposed to an injury, a physician should not limit themselves when investigating a patient’s complaints.
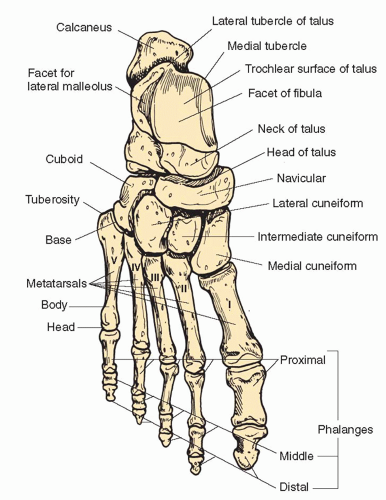 FIG. 20.1. Foot anatomy. Reprinted with permission from Anderson M, Hall SJ. Sports Injury Management. 2nd ed. Baltimore: Lippincott Williams & Wilkins; 2000. |
The subsequent sections discussing the approach to patients with specific foot and ankle complaints will help guide one down a path from a large list of possible diagnoses to the correct one. There are also classic descriptions for some disease processes, such as pain worse with the first few steps of the day in plantar fasciitis, which will be discussed.
Evidence-based Physical Examination
While gathering a detailed history regarding a patient’s complaint can provide valuable information in localizing symptoms, one should always approach the foot and ankle examination with a systematic approach so as to not miss any important detail. Using the opposite, noninjured side as a reference is always helpful as a control. As problems are presented in this chapter, we will discuss specific details of the physical examination important to diagnosing that specific problem. In general, however, the examination should proceed as follows.
Inspection
Observe for evidence of swelling, ecchymosis, or skin injury, which might be indicative of trauma. Observe for erythema, which might be indicative of infection or inflammation. Be aware of skin changes or ulcerations that could suggest vascular problems or diabetes, particularly between the toes. Areas of thickened skin could point to bony prominences. Note any foot or toe deformity, particularly in stance, which could hint at the underlying cause of a chronic foot and ankle complaint (i.e., hindfoot varus in chronic ankle instability).
Palpation
Attempt to find areas of tenderness to localize symptoms. This might be over a bony prominence in the case of a stress fracture or over a tendon sheath as in posterior tibialis dysfunction. Also, determine if malalignment or deformities are flexible or fixed as this may influence treatment options. Check for intact sensation through all distributions in the foot. This includes superficial peroneal nerve, deep peroneal nerve, sural nerve, saphenous nerve, and tibial nerve, which divides into lateral plantar and medial plantar nerves.
Range of Motion
Test both active and passive ranges of motion to assure there is no restriction. Joints that should be assessed are the ankle joint, subtalar joint, midfoot, metatarsophalangeal (MTP) joints, and interphalangeal joints. Any restriction or pain with range of motion should be noted, again helping to localize the etiology of a patient’s presenting complaint.
Strength Testing
The basic function of all muscle groups crossing the ankle and within the foot should be tested. This includes ankle dorsiflexion and plantarflexion as well as foot inversion and eversion and toe flexion and extension. In addition to proper function, their strength should be examined. Asking a patient to walk on their heels and on their tiptoes is a simple way to assure all muscle groups are functioning, and at full strength. Specific tests such as a single heel rise to look for posterior tibialis dysfunction can be helpful in localizing pathology.
Laxity Tests
Examining the joints of the foot and ankle for stability is valuable in attempting to determine a source of discomfort. When testing for laxity, comparison to the uninjured side gives a valuable frame of reference. For instance, a test such as the anterior drawer test at the ankle is helpful in trying to discern between ankle joint instability and peroneal tendon degeneration.
As with a careful history, a detailed and systematic physical examination is critical to narrowing a broad list of differential diagnoses. The examination techniques discussed earlier and those discussed in the following approaches to disease sections are all an important part of the diagnosis puzzle. As one becomes more facile with the foot and ankle and the presenting complaints and physical findings, navigating the list of possible diagnoses will become much easier. It is important, however, especially when one is unsure of the diagnosis, to be as thorough as possible so as not to bypass any critical finding. For instance, numbness and tingling of the medial foot could represent a tarsal tunnel syndrome, if accompanied by a positive nerve compression test or Tinel’s sign at the ankle. If, however, one has not attempted a straight leg raise or found similar symptoms in a stocking pattern on the other foot, one may not be able to discern a patient’s tarsal tunnel syndrome from another etiology for foot pain such as disk herniation in the spine or diabetic neuropathy.
Diagnostic Testing
Diagnostic tests acquired in investigating complaints of the foot and ankle should be ordered with a purpose. That is to say, any test that is obtained should help in delineating a diagnosis from a list of possibilities.
Laboratory
Laboratory tests are helpful when it is thought that a chronic foot and ankle injury stems from an underlying medical disease. Lab values are helpful in investigating rheumatoid arthritis or inflammatory disease as a possible cause of joint pain or inflammation. Also, if there is a concern for infection, inflammatory markers are helpful.
Imaging
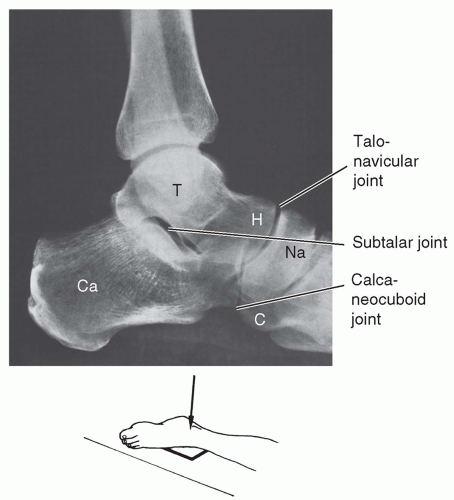
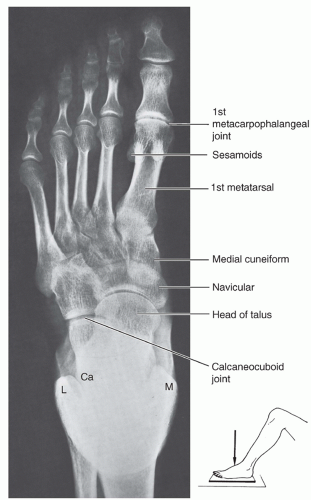
Imaging studies are the most commonly ordered and most useful studies available for investigating chronic injuries of the foot and ankle. X-rays are always the first line of imaging, where anteroposterior (AP), oblique, and lateral views of the foot and AP, mortise, and lateral views of the ankle should be obtained (Figs. 20.4, 20.5 and 20.6). The subsequent sections on specific diagnoses discuss specific x-ray findings, but in general one should look for obvious fractures, dislocations, or malalignment.
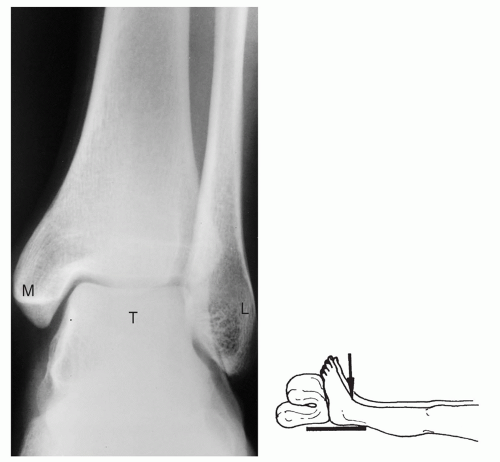 FIG. 20.4. Ankle XR, AP. From Drs. P. Bobechko and E. Becker, Department of Medical Imaging, University of Toronto, Ontario, Canada. M, medial malleolus; T, talus; L, lateral malleolus. |
In addition to x-rays, computerized tomography (CT) and magnetic resonance imaging (MRI) are helpful for additional detail. CT is most helpful for bony injury, namely, stress fracture. They can be obtained with coronal, sagittal, and axial cuts to create the geometry of a bony injury. The advantage of MRI is the ability to evaluate soft-tissue structures such as tendons and ligaments. These studies are extremely helpful in diagnosis such as for peroneal tendon subluxation where it is important to evaluate the integrity of the superficial peroneal retinaculum and determine if there is any midsubstance tendon degeneration.
Ultrasound is another imaging modality that can be used to investigate tendinous degeneration or soft-tissue lesions. It has also been helpful in investigating and diagnosing Morton’s neuromas.
Lastly, a bone scan is used in the instance where bone pathology cannot be properly seen on plain x-ray. This arises mostly in the instance of Freiberg’s infraction or stress fractures. In these circumstances, the bone scan shows increased uptake in the area of question, aiding in the diagnosis of injury with normal radiographs.
Other Testing
In cases of concern for nerve injury or compression, electromyography (EMG) can be obtained to verify the diagnosis. Problems such as tarsal tunnel syndrome can be diagnosed with history and physical examination. The added information of the EMG can help not only in reassuring proper diagnosis but also in documenting preoperative function for a means of comparison to postoperative result.
APPROACH TO THE ATHLETE WITH FUNCTIONAL ANKLE INSTABILITY
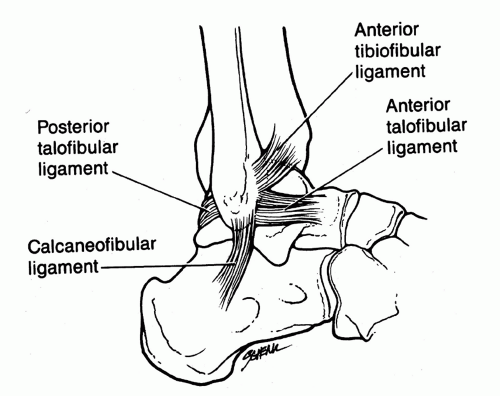
Ankle injuries are very common, accounting for 40% of all sports injuries.2 The injury often occurs on the lateral aspect of the ankle where three separate ligaments function to stabilize the joint—the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PFL) (Fig. 20.7). Also contributing to stability at the ankle through dynamic restraint are the peroneal muscles. Bony structures add a last element of stability to the ankle, particularly in dorsiflexion where the wider anterior aspect of the talus rests within the mortise.
Only about half of the patients presenting with ankle injury develop long-term sequelae, most notably chronic ankle instability. Chronic ankle instability can be mechanical, where the patient does not have any symptoms of instability, but the lateral ankle feels lax on examination, or functional, where the patient describes a history of instability.
HISTORY AND PHYSICAL EXAMINATION
Patients primarily complain of their ankle “giving way” or “rolling over,” demonstrating motion at the ankle beyond their control. One might also describe a snap or pop sound with the instability episodes that might be followed by pain and swelling. It is important, however, to determine if the pain lasts between sprains. This might suggest another source of pathology other than lateral ankle instability such as osteochondral injury to the talus, peroneal tendon instability, or synovitis.
On physical examination, one might find a varus position to the hindfoot, perhaps predisposing the ankle to lateral ankle sprains. Patients might have tenderness to palpation at the lateral ankle. The most common test is the anterior drawer test, which is performed with the leg hanging off a table at 90 degrees. With one hand stabilizing the tibia, the other attempts to translate the foot forward at the ankle, with the foot about 25 degrees plantarflexed while allowing for internal rotation of the foot with translation. If the motion is greater than 9 to 10 mm or more than 5 mm greater than the opposite side, then it is considered a positive test. Another examination is the varus instability test, where the foot is stressed to inversion to examine lateral-sided laxity. One should remember, however, to examine the entire foot and ankle as other problems such as peroneal tendon pathology can create similar symptoms.
DIAGNOSTIC TESTING
Overall, the diagnosis of chronic functional ankle instability is generally made by patient history and physical examination. X-rays should be ordered to help eliminate bony lesions such as tarsal coalition as a source of pathology for
ankle instability. There has been investigation into stress radiographs to examine the excursion of the talus with anterior drawer maneuver, but this method has been shown to not have much clinical relevance3; thus, it is not routinely used.
ankle instability. There has been investigation into stress radiographs to examine the excursion of the talus with anterior drawer maneuver, but this method has been shown to not have much clinical relevance3; thus, it is not routinely used.
Another helpful study is an MRI, which can help evaluate the ligaments of the ankle. One might find an attenuated or ruptured ATFL. Perhaps just as important is the ability of the MRI to evaluate the peroneal tendons, the dome of the talus for osteochondral lesions, and the joint space for loose bodies, all of which could cause symptoms simulating ankle instability.
TREATMENT
Nonoperative
Rest
Ice
Elevation
NSAIDs
Physical therapy (stretching, strengthening, proprioception)
Orthotics (lateral heel wedge/post)
Taping (if continuing sports)
Reusable ankle bracing
Operative
Operative treatment should only be considered when nonoperative measures fail.
Many different types of procedures exist with the Brostrom procedure (lateral ligament repair/reconstruction) being very common.
Arthroscopy can be performed to evaluate intra-articular pathology.4
Postoperatively, patients will be casted and non-weight bearing for 2 to 3 weeks followed by a weight-bearing cast or boot and gentle range of motion
At 4 to 6 weeks, patients will begin active range of motion and peroneal strengthening exercises.
By 10 to 12 weeks, patients should be nearing full recovery, and if they are not able to return to their preoperative level of function, physical therapy should resume.
Prognosis/Return to Play
The prognosis for functional ankle instability is very good.
Nonoperative intervention works well, and patients can return to play when symptoms subside, using taping or bracing as needed.
Should nonoperative management not be successful, the operative options are many and very successful. Whether an anatomic or nonanatomic repair, patients recover from surgery to near preinjury status.
Assuming postoperative management proceeds without complication, athletes can start returning to their sport by 12 weeks, with return to competition when there is no limitation to function.
Athletes may tape their ankles or brace postoperatively. Patients who may not do as well with functional ankle instability are those with long-standing instability, those with generalized ligament laxity, and those with underlying osteoarthritis in the ankle.
Complications/Indications for Referral
With functional ankle instability, patients should be referred to a surgeon when they have failed conservative measures and are still experiencing episodes of instability. Even patients with severe ankle sprains do well with late stabilization surgery,5 so nonoperative measures should be exhausted. Postoperative complications include sural nerve or superficial peroneal nerve irritation. In addition, those patients who have had a stabilization procedure and present with a new instability episode should be sent to see their surgeon. Other indications for referral to a surgeon include patients whose workup for ankle instability revealed another pathology that needs more timely intervention, such as a fracture.
APPROACH TO THE ATHLETE WITH PERONEAL TENDON STRAIN/SUBLUXATION
The peroneal tendons function as the main everters of the foot. They are located on the lateral aspect of the ankle, posterior to the fibula. The peroneus brevis (PB) and peroneus longus (PL) run within the posterior fibular groove and are contained by the superior peroneal retinaculum (SPR), which runs from the fibula to the calcaneus.
Acute injury can cause strain of the tendons or injury to the SPR, which over time could lead to chronic subluxation or degeneration of the peroneal tendons. Generally, the mechanism of injury is sudden dorsiflexion of a plantarflexed, inverted foot. An attenuation or rupture of the SPR in this setting would allow the peroneal tendons to sublux out of the fibular groove and slowly cause tendinosis or tearing of the tendon over time. Additionally, stenosis within the peroneal tendon sheath can lead to development of pathology within the tendons themselves. A peroneus quartus tendon (a normal variant) can cause injury to the PB tendon by compressing it within a narrower space.
HISTORY AND PHYSICAL EXAMINATION
In an acute setting, patients will complain of lateral ankle swelling and ecchymosis, occasionally after hearing or feeling a “pop” (SPR rupture or avulsion) with sudden dorsiflexion of the foot. With chronic peroneal tendon injury, patients will most commonly present with complaint of pain
at the lateral ankle often accompanied by the uncomfortable snapping of subluxing tendons across the fibula. The patient may also complain of ankle instability or a sensation of the ankle giving way. There is not always a discrete event that led to the symptoms, and in some cases, an SPR avulsion or rupture that was previously undiagnosed will be found.
at the lateral ankle often accompanied by the uncomfortable snapping of subluxing tendons across the fibula. The patient may also complain of ankle instability or a sensation of the ankle giving way. There is not always a discrete event that led to the symptoms, and in some cases, an SPR avulsion or rupture that was previously undiagnosed will be found.
On examination, patients will have tenderness with manual pressure over the peroneal tendons. The peroneal tunnel compression test is performed with the knee flexed and the thumb applying pressure over the SPR. Pain as the foot dorsiflexes and everts from a plantarflexed and inverted position is considered positive. Further, patients may be able to voluntarily sublux the tendons with a similar maneuver of eversion and dorsiflexion, which demonstrates instability of the tendons or incompetence of the SPR. Strength examination of the tendons is most often normal; however, it may be uncomfortable for the patient.
DIAGNOSTIC TESTING
X-rays may not be helpful in diagnosing chronic peroneal tendon pathology. However, these images should be obtained, particularly in a patient who had a previous foot or ankle trauma. In an acute setting, one may see a tiny bone fragment signifying an SPR avulsion. In the chronic patient, one might be able to identify a fibular or calcaneal malunion that might have predisposed a patient to developing peroneal tendonitis.
MRI is a helpful diagnostic study as one can see longitudinal split tears of the PB tendon and other tendon irregularities.6 Additionally, one can see fluid in the peroneal tendon sheath or a peroneus quartus that might be creating stenosis. Lastly, MRI can help evaluate the depth of the posterior fibular groove.
TREATMENT
Nonoperative
Rest
NSAIDs
Immobilization
Activity modification
Physical therapy
Operative
Techniques for operative repair include debridement or repair of the peroneal tendons with repair or reconstruction of the SPR.
Postoperatively, patients will be non-weight bearing in a splint for 2 weeks and then weight bearing in a cast for 4 to 6 weeks.
Following this, they will wear a walking boot with gradual progression of range of motion and weight bearing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree