INTRODUCTION
Back pain is a symptom often encountered by athletes of all ages and levels of sports participation. Chronic back pain is the most common reason for missed playing time.
1 Although certain sports such as gymnastics, wrestling, and rowing have a higher prevalence of low back pain due to repetitive mechanical loads placed on the spine, any athlete is at risk. Other factors such as position played, level of training, and gender may also play a role.
1,
2,
3 The majority of back pain among active individuals is self-limited and is usually not associated with underlying structural abnormalities; however, back pain may be a symptom of a more serious disease process. An awareness of sport-specific demands, age-related conditions, risk factors, and warning signs can help narrow the wide differential diagnosis, guide the evaluative process, and lead to proper treatment and return-to-play decisions.
FUNCTIONAL ANATOMY
Bony and soft-tissue elements are integral components of the spine that provide strength and stability, and both are vulnerable to injury. Coordinated movement of the spine is highly complex and is governed by neurologic and biomechanical processes. Any disruption in the process can lead to injury, altered function, and may generate a pain response due to mechanical or chemical sources. A fundamental knowledge of the anatomy of the spine and the biomechanical demands of each sport can help to correctly identify the etiology of back pain in active individuals.
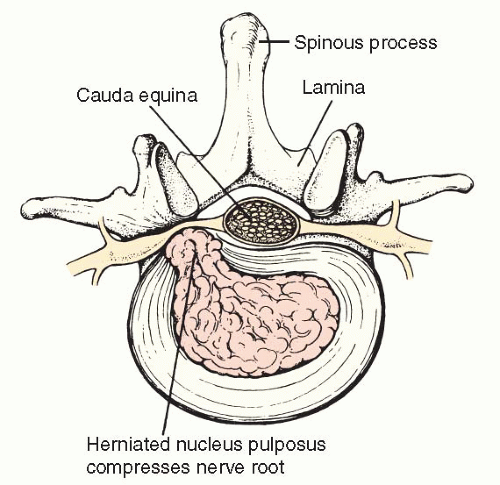
The functional unit of the thoracolumbar spine is the vertebrae and intervertebral discs and is located in the anterior column of the thoracolumbar spine. The intervertebral discs separate two vertebrae and are composed of an inner nucleus pulposus and an outer annulus that is attached to the vertebral endplate. The annulus has sensory innervation, while the nucleus pulposus does not. The nucleus pulposus acts as a shock absorber between adjacent vertebrae. Although it is composed primarily of water at birth, age-related desiccation makes the disc increasingly vulnerable to degeneration or failure caused by acute or chronic mechanical forces. The connection between low back pain and degenerative disc disease is somewhat unclear but is believed to be caused by leakage of inflammatory factors within the nucleus pulposus through annular tears where it comes in contact with nociceptive nerve fibers (
Fig. 16.1).
Radicular back pain is often generated from the spinal nerves which exit through the intervertebral foramina. While the lumbar spinal nerves increase in size descending down the spine, the intervertebral foramina become smaller. Any process that causes additional narrowing of the intervertebral foramen including loss of disc height and osteoarthritis can lead to symptomatic compression of the spinal nerve roots (
Table 16.1).
The posterior column of the thoracolumbar spine consists of the bony vertebral arch, including the pedicles, lamina, pars interarticularis, transverse and spinous processes, and the facet joints (zygapophyseal). The spinal cord is contained within the vertebral arch. The pars interarticularis is particularly vulnerable to injury in young athletes playing sports that involve repetitive trunk rotation and lumbar hyperextension due to the presence of ossification centers in the posterior region of the spine until age 25 and ongoing remodeling and bone growth (
Fig. 16.2). A facet joint is
formed by the inferior articular process of the vertebrae above and the superior articular process of the vertebrae below. This region is innervated with proprioceptive and nociceptive fibers.
Supporting soft-tissue structures include paraspinal muscles, ligaments, and thoracolumbar fascia. Maintenance of posture and functional spinal movement depends on the strength and integrity of the intrinsic muscles of the back. The erector spinae muscle group is the predominant extensor of the lumbar spine and includes the spinalis, semispinalis, longissimus, and iliocostalis muscles. The deepest layer includes the multifidus, semispinalis, and the rotatores that act to extend, rotate, and control deceleration of forceful spinal flexion. The intertransversarii and interspinalis intersegmental muscles allow for ipsilateral side bending and extension, respectively.
Other important supporting structures include the anterior longitudinal ligament that covers the anterior aspect of the spine throughout its course and prevents hyperextension. It is twice as strong as its posterior counterpart, the posterior longitudinal ligament, which helps to prevent hyperflexion. The posterior longitudinal ligament narrows as it approaches the lumbar region, providing only central support and an area of relative weakness in the posterolateral aspect overlying the lumbar disc, therefore accounting for the higher prevalence of posterolateral lumbar disc herniations in the lumbar spine. Both the anterior and posterior longitudinal ligaments have nociceptive fibers.
EPIDEMIOLOGY
Although low back pain is a common complaint in the general population with a prevalence of 85% to 95%, comparison studies between athletes and nonathletes indicate that athletes had significantly higher rates.
1 Low back pain, however, was found to be less common among former elite athletes compared to nonathletes, suggesting that sports involvement is not a risk factor for chronic back pain and may even be protective.
4 Muscle strain is the most common
cause of back pain among athletes.
1,
5 The most common structural etiologies associated with low back pain in athletes are degenerative disc disease and spondylolysis.
1The incidence and anatomic location of back pain vary not only with each sport but also with gender, position played, and level of training.
1,
2,
3 Divers (63%), wrestlers (54%), gymnasts (32%), and rowers have the highest prevalence of severe low back pain.
1,
5 Female rowers (25%) having a higher prevalence of back pain compared to males.
1 Athletes involved in sports requiring repetitive trunk rotation such as golf and racquet sports also frequently experience back pain.
5 Pars interarticularis stress fractures of the spine (spondylolysis) comprise 45% of all stress fractures in female gymnasts.
6 Football lineman have a high prevalence of spondylolysis and spondylolisthesis. Among college and professional players with spondylolisthesis, lineman accounted for nearly 50% in both groups.
5The incidence of spondylolysis seems to be bimodal. The first peak is somewhere from age 3 to 7 years. The majority of cases go undetected, are asymptomatic, and are likely due to normal childhood activity. The prevalence in this age group may be as high as 6% to 10% of all children. The second peak of spondylolysis is in early adolescence. It is most frequently seen in athletes participating in sports that involve repetitive lumbar loading in hyperextension and trunk rotation such as gymnastics, diving, wrestling, weight lifting, and rowing, with a prevalence ranging from 23% to 47%.
1,
7Lumbar disc herniation is a common cause of acute, chronic, or recurrent low back pain, and most frequently occurs at the L5-S1 level.
1 A comparison study of lumbar disc degenerative changes in elite gymnasts versus nonathletes showed a prevalence of 75% and 35%, respectively.
1 Among Olympic athletes studied, 58% had lumbar disc bulging. In contrast, clinically significant thoracic disc herniations comprise less than 1% of all disc ruptures.
8 The prevalence and level of disc degeneration are influenced by the age of the athlete, and type and intensity of the sport.
4,
5 Soccer players have degenerative changes almost exclusively at L4 to S1 levels, whereas weight lifters have more severe degenerative changes in the upper lumbar spine.
4 Among weight lifters older than 40 years, 65% of women and 80% of men demonstrated disc degeneration.
5 The association between radiographic degenerative changes and the prevalence of back pain is unclear.
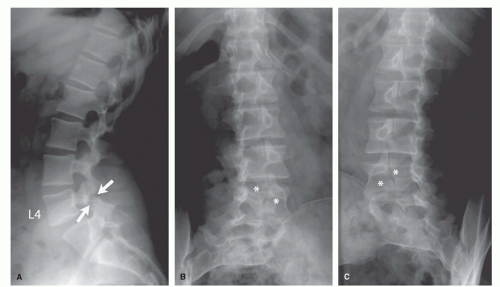
1 Decreased disc space height was the radiographic finding most strongly associated with low back pain and was more strongly correlated with the greater number of levels involved (
Table 16.2).
1