Athlete with Acute Knee Injuries
Nicola DeAngelis
Robert Nascimento
INTRODUCTION
The knee plays a distinct role in a multitude of athletic activities. With the growing participation in competitive and recreational sports, injuries of the knee can affect a broad range of individuals. The general approach to the knee and its associated injuries is best accomplished in a systematic way using a proper history, physical exam, and diagnostic evaluation.
This chapter will review the functional anatomy of the knee as well as the pathophysiology behind various common acute knee injuries in the athlete. With this knowledge, practitioners should have a solid foundation for the diagnosis, initial treatment, and proper reasons for referral, which will best serve and help guide an athlete down the path of a timely recovery.
FUNCTIONAL ANATOMY
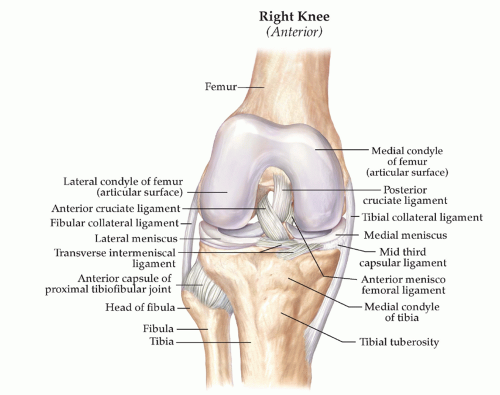
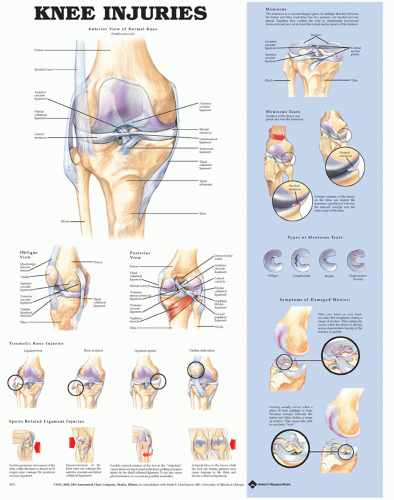
The knee is an exceedingly complex hinged (ginglymus) joint, and its anatomy lends to its sophisticated biomechanical function. Bony and ligament balance provide joint stability in a range of knee motions. In the simplest understanding, the bony architecture of the knee consists of three articulations: the patellofemoral, the medial, and the lateral joint space. The medial compartment contains the medial femoral condyle, the medial tibial plateau, and the medial meniscus. The lateral compartment contains the lateral femoral condyle, the lateral tibial plateau, and the lateral meniscus (Fig. 18.1).
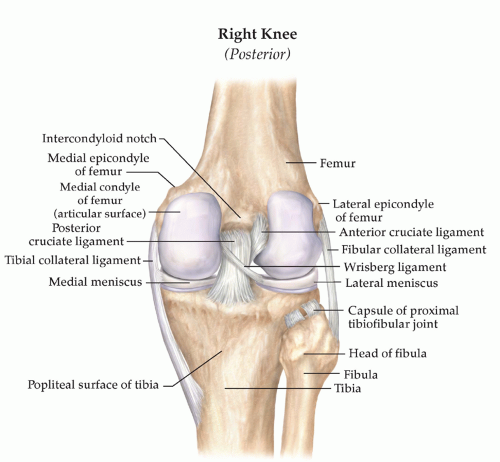
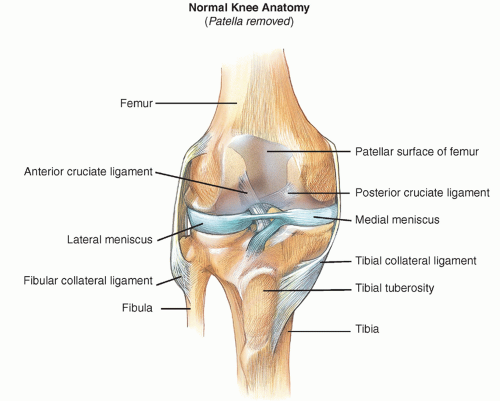
The four primary ligamentous stabilizers of the knee include the anterior and posterior cruciates and the medial and lateral collateral ligaments. Combined, these four ligaments give stability in multiple planes of motion (Figs. 18.2 and 18.3).
The medial collateral ligament (MCL) is divided into three distinct layers. The most superficial layer consists of the deep fascia of the patellar tendon anteriorly and the popliteal fascia posteriorly. The second layer is the superficial MCL, and the third layer is the deep MCL or the medial capsular ligament. The medial structures of the knee are the primary stabilizers for valgus force and act as secondary stabilizers to anterior translation. The MCL contributes 78% to the restraining force on the medial side of the knee.1 It also works in concert with the anterior cruciate ligament (ACL) to allow for external rotation stability. An injury to the MCL increases the stress on the ACL in valgus forces, and thus, ACL-deficient knees rely on the MCL as a secondary stabilizer to anterior translation.2
The ACL is the primary restraint to anterior tibial translation throughout the arc of knee motion. The ACL also is a secondary restraint to varus and valgus stress. The tibial insertion of the ACL is along the anterior portion of the lateral tibial plateau—medial to the anterior horn of the lateral meniscus anteriorly and 2 mm anterior to the posterior cruciate ligament (PCL) posteriorly (Fig. 18.4). On the femoral side, it attaches on the posteromedial aspect of the lateral femoral condyle. The ACL contains two bundles—the anteromedial and the posterolateral. The anteromedial bundle is tight in flexion, while the posterolateral bundle is tight in extension.
The PCL originates along the lateral border of the medial femoral condyle and inserts on the posterior cortical surface approximately 1 to 1.5 cm inferior to the articular surface. Along with the PCL are two meniscofemoral ligaments, the ligament of Humphrey and the ligament of Wrisberg (Fig. 18.5). The PCL is the primary restraint to posterior tibial translation.
The lateral structures of the knee include the lateral collateral ligament, the popliteus muscle and tendon, the popliteofibular ligament, the popliteomeniscal attachment, the iliotibial tract, and the arcuate ligament (Fig. 18.1). Combined, these lateral structures comprise the posterolateral corner (PLC) of the knee and are responsible for a variety of knee restraints, namely, posterior, lateral, and rotatory. The lateral collateral ligament is the knee’s primary restraint to varus load. Injuries to the lateral collateral ligament in isolation are rare, and therefore, other injuries should be suspected when a lateral knee injury occurs.
The menisci, made of predominantly type I cartilage, are semicircular or C-shaped structures that have multiple functions in the knee. The medial meniscus covers less space over the plateau than its lateral counterpart. Both have attachments to the tibial plateau as well as soft-tissue structures within the knee. They derive their blood supply from a perimeniscal capillary plexus as branches from the genicular arteries. Only the outer 10% to 25% of the lateral and 10% to 30% of the medial menisci have direct blood supply; the inner two thirds of the menisci receive nutrition via diffusion. The menisci, in the simplest of senses, function as shock absorbers to the knee. They also participate in load sharing, passive stabilization, reduction in contact stresses within the joint, proprioception, and joint congruity via increased contact surface.
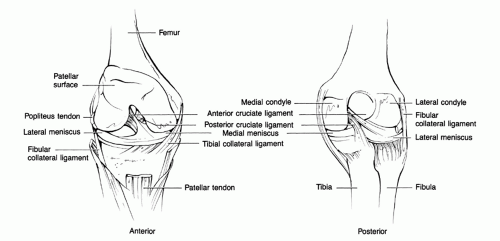 FIG. 18.1. Knee anatomy. Reprinted with permission from Harwood-Nuss A, Wolfson AB, et al. The Clinical Practice of Emergency Medicine. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. |
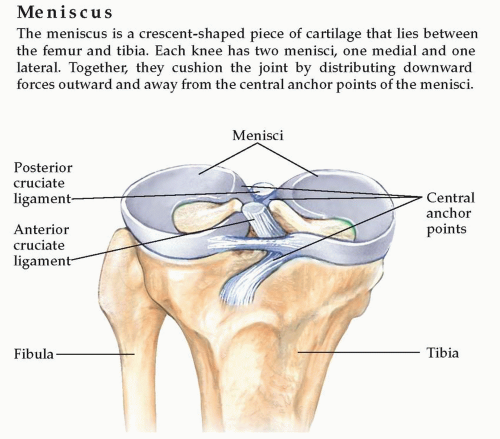 FIG. 18.5. Meniscal Anatomy demonstrating meniscal attachment points and relationship to the cruciate ligaments. |
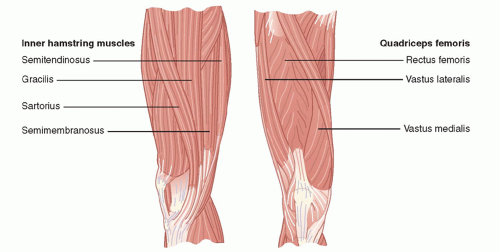
Muscular attachments about the knee also lend to the stability of the joint. The quadriceps musculature anteriorly in conjunction with the patella and patellar tendon, known as the extensor mechanism, is responsible for extension of the knee (ability to straight leg raise). The posterior musculature, and particularly the hamstrings complex, is responsible for flexion of the knee (bending) (Fig. 18.6).
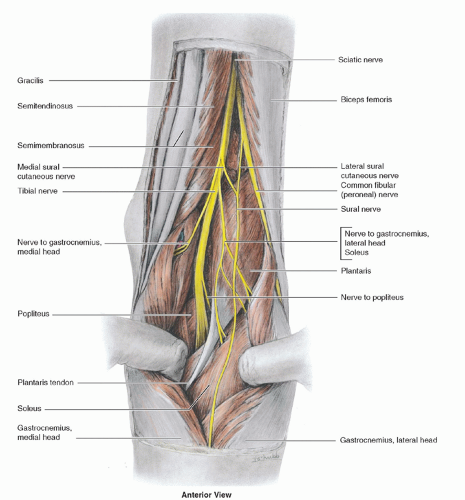
The neurovascular bundle runs along the posterior margin of the knee and can be injured acutely. The blood supply to the knee consists of a network of genicular branches from
the popliteal system. The tibial and peroneal nerves, which innervate the lower extremity and foot, also course posterior to the knee and are at risk at the time of initial injury to the knee (Fig. 18.7).
the popliteal system. The tibial and peroneal nerves, which innervate the lower extremity and foot, also course posterior to the knee and are at risk at the time of initial injury to the knee (Fig. 18.7).
EPIDEMIOLOGY
The potential morbidity of knee injuries has led many physicians, trainers, coaches, and athletes themselves to attempt to identify the factors predisposing to these injuries in the hope of minimizing risk. Injuries are categorized by bony, ligamentous, or meniscal involvement. The type of injury that is encountered depends, to some extent, on the type of athletic pursuit. The majority of studies on preventing injury have centered around football in the United States and soccer internationally.
The most significant trend in acute knee injuries over the past 20 years has been the rise of ACL tears, with a disproportionately higher rate among female athletes. The incidence of ACL injuries is estimated at approximately 200,000 a year
with upward of 100,000 ACL reconstructions a year. Recent studies have shown a difference between the rates of ACL injuries in women compared to men. Speculation as to the reasons for this is unclear. Some authors account for a decreased protective role of dynamic stabilizers (quadriceps and hamstrings) in women, while others note the smaller-diameter ACL and narrower intercondylar notch as reasons for the increased incidence.3 In any event, an ACL injury can be a devastating injury for the competitive and recreational athletes alike.
with upward of 100,000 ACL reconstructions a year. Recent studies have shown a difference between the rates of ACL injuries in women compared to men. Speculation as to the reasons for this is unclear. Some authors account for a decreased protective role of dynamic stabilizers (quadriceps and hamstrings) in women, while others note the smaller-diameter ACL and narrower intercondylar notch as reasons for the increased incidence.3 In any event, an ACL injury can be a devastating injury for the competitive and recreational athletes alike.
PCL injuries have historically been underdiagnosed because these are often asymptomatic. Some studies have shown an incidence of up to 44% of all acute knee injuries.4
The overall incidence of posterolateral injuries of the knee is rare and has been reported to be less than 2% of all acute ligament knee injuries.5 Approximately 40% of all posterolateral knee injuries occur during sports activities.6
The annual incidence of meniscal tears is 60 to 70 per 100,000.7,8 Injuries occur more commonly in men, with the male-to-female ratio of 2.5:1 to 4:1.9 Meniscal injuries are also highly associated with other injuries within the knee. Lateral meniscal tears are more common acutely with an ACL tear,10 whereas chronic ACL tears are associated with medial meniscal tears. Meniscal tears also have been reported frequently in the setting of an acute tibial plateau fracture.
The incidence of osteochondritis dissecans (OCD) of the knee has been estimated at between 0.02% and 0.03% based on knee radiographs and 1.2% based on arthroscopy.11,12 The highest rates are among children aged 10 to 15, and the male-to-female ratio approaches 2:1. Approximately 15% to 30% of cases reported are bilateral.13 A history of trauma is reported in as many as 40% of OCD lesions, although this has recently been challenged.14
NARROWING THE DIFFERENTIAL DIAGNOSIS
History
In the initial approach to the acute knee injury in the athlete, it is imperative to obtain a detailed history. This coupled with a thorough physical exam will significantly narrow the differential and ultimately the diagnosis (Fig. 18.8).
Important questions to ask include a complete description of the mechanism of injury and localizing symptoms. This includes the onset, location, severity, and intensity of the pain as well as the alleviating and modifying factors. Specific questions to ask if not given in the overall description of the mechanism include the following:
Position of the knee at the time of injury (i.e., extension vs. flexion)
Anterior versus posterior symptoms; medial versus lateral symptoms
Twisting/rotational injury versus axial load injury
Varus stress/valgus stress
Catching or locking of the knee
An initial “pop” or later “clicking”
Presence of an effusion
Ability to range
Ability to weight bear
Presence of a deformity
Certainly the position of the knee can play a role in the injury process. An extended knee has more inherent stability than a flexed knee but could be subject to axial loading forces with the end result in fracture. These patients will be very uncomfortable with weight bearing. The location of symptoms often helps narrow the differential by assigning a compartment of injury, be it on the medial or the lateral side, where one can have an injury to the collateral ligament, meniscus, or plateau. The presence of an effusion helps to depict between intra-articular and extra-articular pathology, while catching or locking of the knee is often present in meniscal injuries. If the patient complains of a varus or valgus load, meniscal and collateral ligament pathology is brought to the forefront of the differential. Twisting injuries are suspicious for anterior cruciate tears, and the patient can often account for an audible or sensible “pop.” Some very common injuries in the athlete will be discussed later in this chapter with keys to the history and physical outlined.
Evidence-based Physical Exam
After a through history has been elicited, physical exam of the knee is an important step to narrow the differential diagnosis. The general exam techniques as well as injury-specific exam techniques described later in this chapter can help to differentiate between the most common diagnoses for each particular compartment, or area, of the knee. Location of tenderness, ligament laxity, presence of an effusion, and range of motion (ROM) are keys to the physical exam that will always be helpful to narrow the differential. It is important to remember that possibly the greatest and most morbid knee injury in an athlete is a frank dislocation. This should be clearly evident by gross deformity, severe pain, an inability to range or weight bear, and sometimes neurovascular compromise. Knee dislocation is an emergency, and failure to recognize a knee dislocation may lead to devastating residual injuries and even amputation. These patients should be evaluated at the nearest emergency department for radiographic confirmation, prompt reduction, and further treatment, as necessary.
Once a proper history is taken, attention can then turn toward the physical exam. A systematic approach to the knee should be preformed with particular attention paid to differences between the affected and unaffected sides. This statement, although true in any athletic extremity injury, is particularly important with the knee exam.
Inspection
The overall position of the knee can lend some insight into the injury process. Ecchymosis or edema can lead an examiner toward a particular area of injury. Evidence of an effusion helps to differentiate between intra-articular and extra-articular processes. An effusion often presents as swelling about the knee, with the knee held in mild flexion and pain with full extension or moderate flexion. A gross deformity can also be present, and knee dislocation needs to be ruled out immediately because of the associated devastating consequences.
Palpation
Palpation over the three compartments of the knee can help differentiate injuries in each particular location. Anterior or posterior tenderness to palpation may include injuries to the extensor mechanism and/or hamstrings musculature, respectively. Pain along the medial or lateral portions of the knee is suspicious for collateral ligament injuries. Finally, pain along the joint line, especially the medial joint line, is indicative of meniscal pathology.
Evidence of an Effusion
Presence of an effusion in the setting of an acute knee injury signifies an intra-articular injury and is a key part of the knee exam. The effusion is a red flag for a potential significant knee injury that needs to be identified for proper management. A minimal effusion is best tested by milking down any fluid from the suprapatellar area with the knee held in extension. The fluid can then be concentrated into either the medial or the lateral compartment by gentle pressure over the opposite compartment. Once the fluid is concentrated in one area, gentle pressure over that area will force the fluid to traverse the joint, and it will be felt in the opposite compartment. Presence of an effusion in the setting of an acute knee injury signifies an intra-articular injury and generally indicates a more significant knee injury that needs to be identified for proper management.
Range of Motion
The normal ROM of the knee is from 0 degrees (full extension) to approximately 135 degrees of flexion and 10 degrees of internal and external rotation. Acutely, a decreased ROM is a nonspecific sign of knee injury but may be helpful when associated with other exam findings. A mechanical “block” to ROM may be indicative of a bucket-handle tear of the meniscus and should not be forcefully reduced. It is important to note that with many acute knee injuries, it is common to have a limited ROM. This is usually secondary to pain and/or presence of an effusion.
Strength
Strength should be accessed in the acute injury as well. This will often be difficult secondary to pain associated with the injury. The strength both of the hamstrings and of quadriceps should be accessed and documented. The patient should also be asked to perform a straight leg raise. This maneuver entails keeping the knee extended and lifting the lower extremity off the bed/ground straight in the air. If the patient is able to straight leg raise, or can at least hold elevation of the leg for a short period of time, the extensor mechanism (quadriceps, patella, patella tendon) is intact.
Ligaments
The most important component to the ligament exam of the knee is the comparison to the opposite (unaffected) knee. This is the best way to gauge an abnormal test. The most basic of approaches to the ligament exam will be discussed here. A more detailed exam will also be outlined with the specific injuries to follow.
Collateral Ligaments
To test the MCL, a valgus stress (knee is stabilized, and pressure is applied on the lateral side of the knee and the medial side of the ankle) is applied with the leg in full extension and in 30 degrees of flexion. To test the lateral collateral ligament, a varus stress is applied with the leg again in full extension and 30 degrees of flexion. Any laxity of these motions with respect to the unaffected side is suspicious for an injury.
Cruciate Ligaments
The Lachmann’s examination is the preferred method for assessing the integrity of the ACL. With the femur/thigh stabilized with one hand, take the leg in the opposite hand near the tibial tubercle and attempt to translate the tibia forward with respect to the femur. A positive test will exhibit increased laxity and no firm “end point” in comparison to the unaffected knee.
The posterior cruciate is best tested with the patient lying down with the hip flexed and the knee at 90 degrees. A posterior force is applied to the proximal tibia with respect to the femur. If the subluxation is greater than the other side, and there is no stiff end point, then a PCL injury is suspected. This is called the posterior drawer test.
Diagnostic Testing
In the workup of knee injuries in the athlete, there are many imaging modalities that will aid in the narrowing and, sometimes, confirmation of the diagnosis.
Laboratory
Routine laboratory analysis is generally not required in the setting of an acute knee injury. If infectious or autoimmune etiology is suspected, then appropriate serology and/or cultures should be obtained.
Imaging
Plain radiographs are usually the initial test that can show any associated fractures and dislocations. Any fracture or dislocation should be seen promptly by an orthopedist. X-ray may also show evidence of bony ligament avulsion either on the medial or on the lateral sides. The lateral radiograph lends information about the congruency of the joint as well as evaluation of the patella. A high- or low-riding patella (patella alta or baja) could be an indication of a patellar or quadriceps tendon tear, respectively.
Other Testing
Computerized tomography (CT) is also very useful in the evaluation of the acute knee injury. CT gives very fine definition of the bony structures of the knee and can confirm evidence of an effusion. It is also helpful for the evaluation of an occult fracture.
Magnetic resonance imaging (MRI) has shown to be extremely useful in many acute knee injuries. MRI gives outstanding detail and the precise location of ligament and menisci injuries.
APPROACH TO THE ATHLETE WITH MEDIAL COLLATERAL LIGAMENT INJURIES
HISTORY AND PHYSICAL EXAMINATION
The diagnosis of MCL injuries is related to the mechanism of injury. The typical injury is one of a valgus moment to the knee. Patients typically present with tenderness along the medial portion of the knee from femur to tibia. They sometimes note a sense of instability with weight bearing.
On physical exam the MCL should be tested at both full extension and 30 degrees of flexion. It is imperative for an adequate exam that the patient be completely relaxed. The exam at full extension tests both the MCL as well as the associated capsular and cruciate ligament injuries. Exam at flexion isolates the MCL complex. A difference of only 5 to 8 mm is indicative of significant injury.1 Palpation along the course of the ligament is helpful in determining the location of the injury. A proximal MCL tear is more common than a distal avulsion. After injury to the MCL is determined, a complete exam of the knee is warranted to rule out concomitant injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree