CHAPTER ONE ASSESSING MUSCULOSKELETAL DISORDERS
AXIOMS IN ASSESSING MUSCULOSKELETAL DISORDERS
INTRODUCTION
The history provides much information about the pathologic process involved and the impact of the condition on the patient, whereas the orthopedic physical examination is essential to define the anatomic structures involved; together these processes allow differentiation of orthopedic disorders into various categories.
ORTHOPEDIC GAMUT 1-1 ORTHOPEDIC EVALUATION PROCESS
The orthopedic evaluation process has three phases:
ORTHOPEDIC GAMUT 1-2 CLINICAL ASSESSMENTS
In clinical practice, assessments occur all day every day, including:
The accuracy of a test for detecting a disease or a condition is determined by sensitivity and specificity. A high sensitivity (or a high specificity) does not suffice to make a test useful in clinical practice; a test should be as sensitive as possible. The sensitivity and specificity of examination procedures and tests can often be found in the literature. Sensitivity and specificity are important characteristics of evidence-based physical assessment procedures but only in the context of a specific disease or condition.
ORTHOPEDIC GAMUT 1-3 BAYES THEOREM
Rules of Thumb Rationale for use in clinical situations:
The decision of whether to perform a new test depends on the result of the previous test. Procedures with the lowest burden, risk, and costs for the patient are performed first, and those with the highest burden, risk, or costs are reserved for certain patients in which the prior probability is highest. Examination procedures in the context of a low prior probability of disease are rarely, if ever, informative, with the yield of diagnostic testing that will increase the prior probability approximating 50%. Very experienced clinicians intuitively apply these rules and arrange their diagnostic process in such a way that the highest possible yield (a highly probable diagnosis) will be obtained at the lowest possible burden, risk, and cost for the patient. Less-experienced clinicians may learn from experienced colleagues by recalling Bayes theorem and implementing its principles in everyday clinical practice.
ORTHOPEDIC GAMUT 1-4 PRÉCIS OF PHYSICAL EXAMINATION
The history provides much information about what difficulties the patient is experiencing and the impact of these on the patient. Orthopedic examination is essential to define the structures involved; together, these processes allow differentiation of orthopedic disorders into various diagnostic categories (Box 1-1).
HISTORY
ORTHOPEDIC GAMUT 1-5 ELECTRONIC PATIENT RECORD KEEPING
OBSERVATION AND INSPECTION
ORTHOPEDIC GAMUT 1-7 OBSERVATION AND INSPECTION
ORTHOPEDIC GAMUT 1-8 PAIN-BASED CLINICAL REASONING
Five main categories of pain-based clinical reasoning are:
A useful approach in clinical examination of the neuromusculoskeletal system is to seek answers to the Critical 5 questions for an orthopedic specialist. Once all five questions are answered, a differential diagnosis can usually be established (Box 1-2).
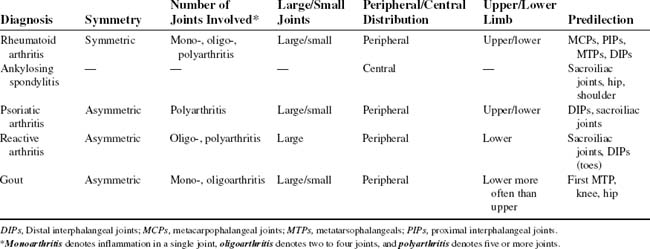
The physician needs to learn what exacerbates or relieves the symptom pattern. Equally important is how long the complaints have existed (Table 1-1).
PALPATION
NEUROLOGIC EVALUATION
ORTHOPEDIC GAMUT 1-16 COMMON AREAS OF MENSURATION
RANGE OF MOTION
ORTHOPEDIC GAMUT 1-19 JOINT END-FEEL CATEGORIES
In passive joint motion assessment, the end-feel is important. The accepted end-feel categories are:
STABILITY TESTING
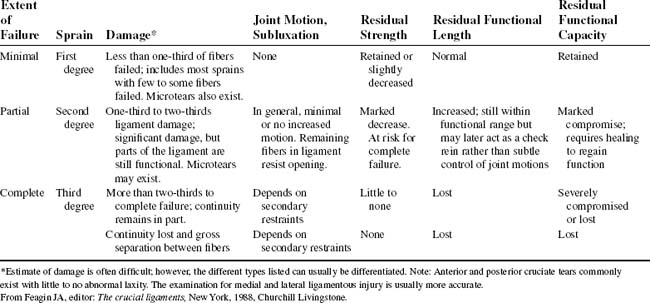
Because clinical examination reveals the degree of ligamentous or joint sprain (Table 1-2), the examiner must be able to test accurately for joint instability. Stability testing moves joint and periarticular structures through their respective arcs and end-range motions. Stability testing involves stressing ligamentous tissues and joint capsules.