CHAPTER EIGHT LUMBAR SPINE
AXIOMS IN ASSESSING THE LUMBAR SPINE
INTRODUCTION
As many as 90% of patients with back pain have a mechanical reason for their pain. Mechanical low back pain may be defined as pain secondary to overuse of a normal anatomic structure or pain secondary to trauma or deformity of an anatomic structure. The age of a patient is helpful in determining the potential cause of back pain. In considering spondyloarthropathies, clinical characteristics help in differentiating the diseases belonging in this group (Table 8-3 and Table 8-4). The sex of the patient may also help select potential causes of low back pain. Certain disorders occur more often in men, whereas others are associated more commonly with women. Others occur equally in both sexes (Table 8-5).
TABLE 8-3 CLINICAL CHARACTERISTICS OF SPONDYLOARTHROPATHIES
HLA, Human leukocyte antigen.
Adapted From Kelley WN et al: Textbook of rheumatology, ed 5, Philadelphia, 1997, WB Saunders.
TABLE 8-4 DISEASES BELONGING TO THE SPONDYLOARTHROPATHIES
Adapted From Kelley WN et al: Textbook of rheumatology, ed 5, Philadelphia, 1997, WB Saunders.
TABLE 8-5 GENDER PREVALENCE IN LOW BACK PAIN
| Male predominance | |
| Female predominance |
Data from Klippel JH, Dieppe PA: Rheumatology, vol 1-2, ed 2, London, 1998, Mosby.
Even if treatment involves only a localized part of the lumbar spine, in each case, the lumbar spine has to be considered as a functional unit consisting of bones, ligaments, intervertebral discs, muscles, and all other soft tissues. Because of their central location, spinal elements represent the focal point for the equilibrium of the body. Because of the many connections and relations, spinal changes influence some organs directly, and the functional equilibrium of the spine depends on the efficient performance of other organs.
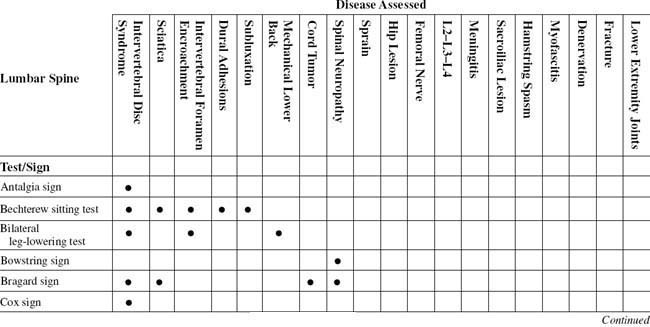
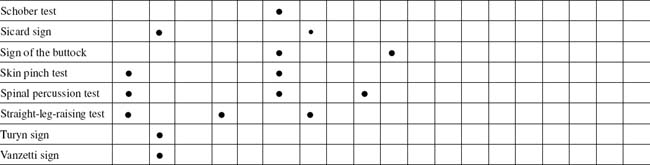
TABLE 8-2 LUMBAR SPINE CROSS-REFERENCE TABLE BY SYNDROME OR TISSUE
| Cord tumor | |
| Denervation | |
| Dural adhesions | |
| Femoral nerve | |
| Fracture | |
| Hamstring spasm | Lewin standing test |
| Hip lesion | |
| Intervertebral disc syndrome | |
| Intervertebral foramen encroachment | |
| L2–L3–L4 | |
| Lower extremity joints | Quick test |
| Mechanical lower back | |
| Meningitis | Kernig/Brudzinski sign |
| Myofascitis | |
| Sacroiliac lesion | |
| Sciatica | |
| Spinal neuropathy | |
| Sprain | |
| Subluxation |
During fetal development, the spine may be exposed to many influences, such as drug-induced malformations, lack of oxygen, or radiation.
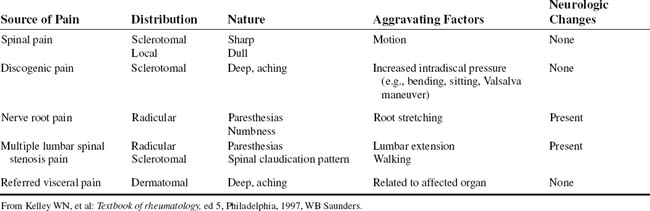
The anatomic structures of the lumbosacral spine receive specific types of sensory innervation that are associated with distinct qualities of pain (Table 8-6).
ESSENTIAL MOTION ASSESSMENT
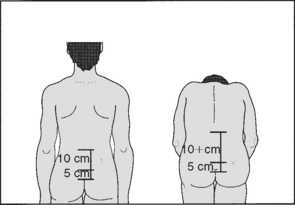
To assess the contribution made to flexion by the lumbar spine, the examiner should mark the spine at the lumbosacral junction and then 10 cm above and 5 cm below this point. On forward flexion, the distance between the two upper marks should increase by approximately 4 cm, the distance between the lower two remaining unaltered (Figs. 8-1 to 8-4).
ESSENTIAL MUSCLE FUNCTION ASSESSMENT
Useful in screening is muscle testing of the legs, which measures strength on a 5-point scale for extension and flexion (knee), abduction and adduction (hip), and eversion and inversion, as well as dorsiflexion and plantar flexion (foot) (Table 8-7).
ORTHOPEDIC GAMUT 8-1 LOWER EXTREMITY MUSCULATURE
Sequential innervation lower extremity musculature:
For patients in whom the objective findings do not match the subjective complaints, close observation helps identify the inconsistencies (Table 8-8). A finding of three or more of the five signs of the Waddell index is clinically significant. Isolated positive signs are ignored.
TABLE 8-8 NONORGANIC PHYSICAL SIGNS INDICATING ILLNESS BEHAVIOR
| Physical Disease/Normal Illness Behavior | Abnormal Illness Behavior | |
|---|---|---|
| Symptoms | ||
| Pain | Anatomic distribution | Whole leg pain |
| Tailbone pain | ||
| Numbness | Dermatomal | Whole leg numbness |
| Weakness | Myotomal | Whole leg giving way |
| Time pattern | Varies with time and activity | Never free of pain |
| Response to treatment | Variable benefit | Intolerance of treatments |
| Emergency admissions to hospital | ||
| Signs | ||
| Tenderness | Anatomic distribution | Superficial |
| Widespread nonanatomic | ||
| Axial loading | No lumbar pain | Lumbar pain |
| Simulated rotation | No lumbar pain | Lumbar pain |
| Straight leg raising | Limited on distraction | Improves with distraction |
| Sensory | Dermatomal | Regional |
| Motor | Myotomal | Regional, jerky, giving way |
From Demeter SL, Andersson GBJ, Smith GM: Disability evaluation, St Louis, 1996, Mosby.
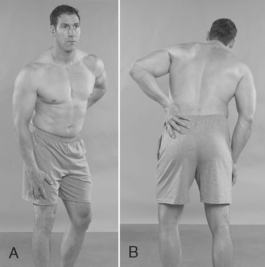
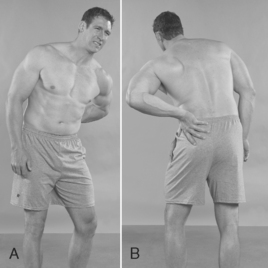
The iliacus arises from the iliac fossa and joins the psoas under the inguinal ligament. The iliacus then crosses the hip joint capsule and inserts into the lesser trochanter of the femur. These muscles flex the lumbar spine and bend it toward the same side. The quadratus lumborum, which lies lateral to the vertebral column, arises from the posterior part of the iliac crest and iliolumbar ligament and inserts into the twelfth rib and the tips of the transverse processes of the upper four lumbar vertebrae. This muscle fixes the diaphragm during inspiration and bends the trunk toward the same side when it acts alone (Figs. 8-5 to 8-7).
ANTALGIA SIGN
Assessment for Posterolateral, Posteromedial, and Posterocentral Intervertebral Disc Protrusion
Comment
Two major types of low back abnormalities center on the intervertebral disc: acute impairment from herniated discs and chronic impairment from degenerative disc disease (Table 8-9).
TABLE 8-9 LUMBAR DISC SYNDROMES
| Lumbar Herniated Nucleus Pulposus | Degenerative Disc Disease | |
|---|---|---|
| Physical examination findings | ||
| X-ray findings |
CT, Computed tomography; MRI, magnetic resonance imaging.
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
ORTHOPEDIC GAMUT 8-2 DISC INJURIES
Definitions of disc injuries are as follows:
PROCEDURE
PROCEDURE
BOWSTRING SIGN
Assessment for Lumbar Nerve Root Compression
ORTHOPEDIC GAMUT 8-3 LUMBOSACRAL NERVE ROOTS
ORTHOPEDIC GAMUT 8-4 WALLERIAN DEGENERATION SEQUENCE
PROCEDURE
PROCEDURE
COX SIGN
Assessment for Prolapse of Intervertebral Disc Nucleus
Comment
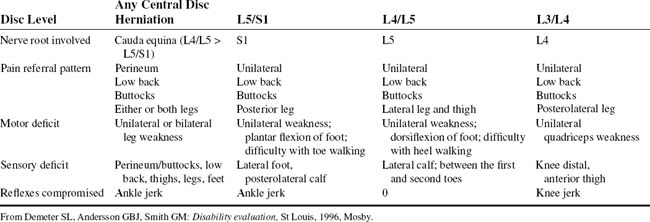
Several maneuvers tighten the sciatic nerve and compress an inflamed nerve root against a herniated lumbar disc. With the straight-leg-raising tests, the L5 and S1 nerve roots move several millimeters at the level of the foramen. The L4 nerve root moves a smaller distance, and the proximal roots show little motion. The straight-leg-raising tests are most important and valuable for detecting lesions of the L5 and S1 nerve roots. Young patients with herniated discs have marked propensities for positive straight-leg-raising tests. Although the test itself is not pathognomonic, a negative test rules out the possibility of a herniated disc. After age 30, a negative straight-leg-raising test no longer precludes this diagnosis. Lumbosacral transitional vertebrae complicate this further (Table 8-10).
TABLE 8-10 CASTELLVI CLASSIFICATION OF LUMBOSACRAL TRANSITIONAL VERTEBRA
• Type III: complete lumbarization/sacralization • Type IIIa enlarged transverse process that has unilateral complete fusion with the adjacent sacral ala |
PROCEDURE
DEMIANOFF SIGN
PROCEDURE
DEYERLE SIGN
Assessment for Sciatic Nerve Irritation
Comment
Occasionally, L4 lesions may also cause similar symptoms and signs. The phase of degeneration or spondylosis often determines the level of intervention (Table 8-11).
TABLE 8-11 OVERVIEW OF SCHEME OF TREATMENT RELATIVE TO THE PHASE OF SPONDYLOSIS
| Phase | Lesion | Treatment |
|---|---|---|
| Dysfunction | ||
| Unstable | ||
| Stabilization |
From Kirkaldy WH: Managing low back pain, ed 4, Philadelphia 1999, Churchill Livingstone.
PROCEDURE
PROCEDURE
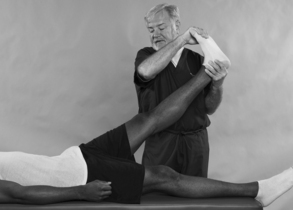
ELY SIGN
ELY HEEL-TO-BUTTOCK TEST
Assessment for Lumbar Radicular or Femoral Nerve Inflammation
Comment
The size of the lumbar vertebral canal ranges from 12 to 20 mm in its AP dimension at the mid sagittal plane and 18 to 27 mm in its transverse diameter. Stenosis has been defined as a narrowing below the lowest value of the range of normal (Table 8-12).
TABLE 8-12 DIMENSIONS OF THE LUMBAR VERTEBRAL FORAMINA (VERTEBRAL CANAL)*
| Dimension | Size (Range)† |
|---|---|
| Anteroposterior (in midsagittal plane) | 12–20 mm |
| Transverse (interpedicular distance) | 18–27 mm |
‡ A typical vertebral foramen is rather triangular (trefoil) in shape. However, the upper lumbar vertebral foramina are more rounded than the lower lumbar foramina. L1 is the most rounded, and each succeeding lumbar vertebra becomes increasingly triangular, with L5 the most dramatically trefoil of all. From Dommisse GF, Louw JA: Anatomy of the lumbar spine. In Floman Y, editor: Disorders of the lumbar spine, Rockville, Md, and Tel Aviv, Israel, 1990, Aspen and Freund Publishing House.
* Dimensions below the lowest value indicate spinal (vertebral) canal stenosis.
† Dimensions of lumbar vertebral foramina are usually smaller than those of the cervical region but larger than those of the thoracic region. From Cramer GD, Darby SA: Basic and clinical anatomy of the spine, spinal cord, and ANS, St Louis, 1995, Mosby.
ORTHOPEDIC GAMUT 8-7 MODIFIED ARNOLD INTERNATIONAL CLASSIFICATION OF LUMBAR SPINAL STENOSIS AND NERVE ROOT ENTRAPMENT SYNDROMES
ORTHOPEDIC GAMUT 8-8 COMPLEX REGIONAL PAIN SYNDROME DIAGNOSTIC CRITERIA (INTERNATIONAL ASSOCIATION FOR THE STUDY OF PAIN)
PROCEDURE
FAJERSZTAJN TEST
PROCEDURE