Arthroscopic Treatment of Anterior Glenoid Bone Loss: Latarjet Techniques
Ettore Taverna
The etiology of anterior-inferior glenohumeral instability is multifactorial. Successful treatment of this condition requires any surgical approach to be sufficiently flexible to allow the surgeon to identify and repair all clinically significant lesions, which may be causing shoulder instability.
At present, anterior-inferior shoulder instability associated with soft tissue lesions can be successfully treated arthroscopically and clinical outcomes are generally equivalent to those after open procedures.
A relationship has been shown between the extent of the glenoid bone loss and the results of the treatment of recurrent anterior shoulder instability. The osseous lesions may influence the results of arthroscopic soft tissue techniques for treating glenohumeral instability.
Glenoid erosion is quite common with chronic anterior shoulder instability and often coexists with a Hill-Sachs lesion. The reported prevalence of anteroinferior glenoid rim fracture or bone erosion ranges from 8% to 90% in shoulders with recurrent anterior dislocation. The lesions are caused by impaction of the posterior-superior humeral head on the anterior-inferior glenoid rim during a dislocation. Severe bony lesions (i.e., large Hill-Sachs lesions and/or glenoid bone loss) are associated with the failure of arthroscopic treatment and constitute the real limit for the arthroscopic approach.
Imaging has shown that 90% of recurrently unstable shoulders have a glenoid defect. Chronic glenoid fractures lead to glenoid bone loss, and the bony fragment tends to disappear with time.
Biomechanical studies have found an inverse relationship between the size of the glenoid defect and the stability of the shoulder: the larger the defect, the less stable the shoulder. The stability of the shoulder decreases as the osseous defect increases.
A large glenoid defect must be treated with glenoid bone grafting when a Bankart procedure is performed. Many authors recommend coracoid transfer if the glenoid rim deficiency involves 25% of the anteroposterior diameter of the glenoid. Others suggest that measures to restore the arc of the glenoid concavity may be beneficial in terms of both stability and motion for patients who have a glenoid defect whose width is at least 21% of the glenoid length. The exact size of the glenoid bone loss that contraindicates an open or an arthroscopic soft tissue repair is still unknown.
Dislocation of the shoulder can produce a wide variety of pathologic lesions. Patients with chronic anterior shoulder instability can be classified as having recurrent dislocations, recurrent subluxations, or a chronically painful shoulder. The reported incidence of bony lesions is variable throughout the existing literature and has been reported to occur in 11% to 90% of cases of recurrent anterior shoulder instability. In addition to an avulsion fracture of the inferior glenohumeral ligament, bony abnormalities of the glenoid associated with anterior instability include a loss of anterior-inferior glenoid bone (Fig. 22.1), probably related to resorption of an avulsion fracture fragment (Fig. 22.2) or a rounding off of the anterior-inferior glenoid bone caused by microimpaction fractures related to multiple dislocations or subluxations.
Arthroscopic techniques have advanced sufficiently so that the shoulder surgeon can successfully repair anterior-inferior glenohumeral instability. Optimally, however, the arthroscopic surgeon should be able to address all clinically relevant lesions, including bony defects, in all cases by incorporating techniques that allow restoration of both the anatomy and the biomechanical function of damaged structures.
The advantages of arthroscopic surgical stabilization include smaller incisions, less soft tissue dissection, the ability to completely inspect the glenohumeral joint, access to all areas of the joint for repair, and potentially, maximum preservation of external rotation. The greatest disadvantage of the arthroscopic procedures until very recently was the inability to successfully treat significant structural bony defects. These techniques continue to evolve, but despite progressive improvement, the results of the arthroscopic treatment of instability have not equaled those obtained with open techniques. The failure
rate of an arthroscopic soft tissue repair has been reported to be between 5% and 30%, especially when performed in a nonselected patient population.
rate of an arthroscopic soft tissue repair has been reported to be between 5% and 30%, especially when performed in a nonselected patient population.
Most authors agree that severe bony lesions in unstable glenohumeral joints are associated with the failure of an arthroscopic Bankart repair. If not properly addressed, plastic deformation of the capsule and ligaments and hyperlaxity could constitute another cause of failure of arthroscopic treatment.
HISTORICAL PERSPECTIVE
In 1923, Bankart proposed retensioning the anterior capsule and reinserting the labrum on the glenoid rim in order to restore the concavity of the glenoid surface. In 1932, Eden and Hybinette proposed the use of a bone block harvested from the iliac crest to increase the glenoid width. Later, the Bristow procedure was first done by Sir Rawley Bristow, who transferred a part of the coracoid process beneath the subscapularis muscle without any rigid attachment. The Bristow procedure transferred only the tip of the coracoid along with the attached conjoined tendon, but these were only sutured to the capsulo-periosteal elements through a short vertical incision made in the subscapularis.
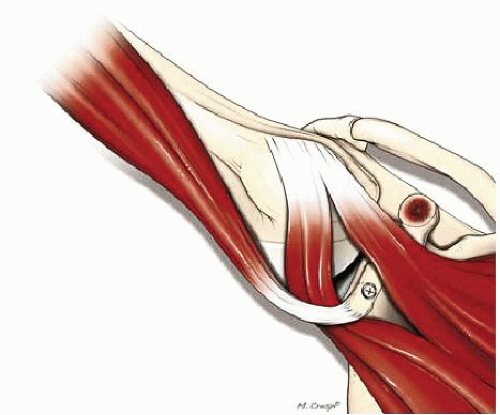
In 1954, Michel Latarjet and Albert Trillat described two different procedures to stabilize the shoulder with the coracoid process and conjoint tendon. Trillat recommended a partial osteotomy of the coracoid process, which was then lowered and medialized before being secured on the anterior glenoid neck with a screw passing through the subscapularis. The main effect of this procedure was the sling created by routing the subscapularis by the conjoint tendon to act as a dynamic checkrein. Notably, the coracoid was not used as a bone block. The Latarjet procedure transfers most of the coracoid as a bone graft that usually measures 2 to 3 cm in length. The efficacy of the procedure is due to a double mechanism: a bone block effect provided by the coracoid, which increases the size of the concavity, and a sling effect provided by the lowering and crossing the subscapularis and conjoint tendon (Fig. 22.3). The success of the combined Trillat-Bristow-Latarjet procedure is from this double effect: a bone block (Latarjet) and a sling effect (Latarjet-Bristow-Trillat). The sling effect allows these procedures to be dynamic operations. The more the patient puts the arm in the throwing position, the more the conjoint tendon acts as a dynamic checkrein, pushing the humeral head backward and lowering the subscapularis. The Eden-Hybinette procedure provided only a bone block effect.
CLINICAL EVALUATION
Pertinent History
Patients presenting with glenohumeral anterior instability with bony lesions report various mechanisms of injury. These mechanisms often include individuals whose arm is taken into forcible external rotation when abducted 90°. A similar pattern can result from a fall on an outstretched, abducted arm. Direct distraction forces on the capsule and ligaments can be the mechanism of the injury. The amount of force required to create the instability is important. Atraumatic or minimally traumatic events lead generally to subluxation. In patients who sustain a dislocation, the force provoking the injury is generally greater and more likely results in capsule and ligament tearing and associated bony lesions.
Individuals who require reduction by a physician at the first dislocation episode are more likely to have a ligament insertion injury while with recurrent episodes bony defects are increasingly common. Patients who spontaneously reduce their shoulder at the first episode are more likely to have capsular elongation, interval enlargement, hyperlaxity, and no bony lesions.
Physical Examination
The diagnosis of shoulder instability is rarely made without a history given by the patient. Symptomatic instability is most often diagnosed by this history and then confirmed by the physical examination. Shoulder apprehension tests in all directions should be performed to confirm the clinical diagnosis. Hyperlaxity of the shoulder should be assessed. Anterior hyperlaxity is defined as external rotation greater than 85° with the arm at the side. Inferior hyperlaxity is defined when the result of the Gagey test test is positive. A positive test occurs when abduction of the affected arm with the scapula blocked by the physician is 20° greater than the other side.
Laxity must be differentiated from instability. Instability is defined as the symptomatic expression of excessive translation. The operative approach is aimed at the direction of the instability rather than all the directions of laxity. The presence of generalized ligamentous laxity is most likely in an individual with multidirectional instability. These patients rarely have any bony lesion associated with the instability. Hyperlaxity is one of the few contraindications for an open or arthroscopic Latarjet procedure.
Numerous instability tests have been described. In addition to the above-mentioned laxity tests, the drawer test should always be performed. The examiner stabilizes the scapula with one hand and grasps the humeral head with the other hand. Anterior and posterior stresses are applied. The amount of translation and pain must be recorded. In the presence of significant glenoid bone loss, anterior translation can cause a dislocation of the shoulder. The apprehension and relocation tests are also often positive in patients with glenoid bone deficits. With the patient supine, the arm is taken into abduction and external rotation, and an anterior stress is applied until the patient’s apprehension is reproduced. Posterior stress is then applied by pressing against the humeral head with reduction of the anterior subluxation and an immediate decrease in the patient’s apprehension.
Imaging
A standard radiographic series for instability should include anteroposterior views done in three rotations (internal, neutral, and external). The presence of a Hill-Sachs lesion should be noted for each rotation (present or absent). If present on the external rotation view, the lesion’s location is more superior on the humeral head. Glenoid lesions are noted and a distinction should be made between an avulsion fracture and the loss of the anteroinferior sclerotic contour using an AP view (Fig. 22.4) or a glenoid profile view with a contralateral comparison view as described by Bernageau (Fig. 22.5).
Fractures are defined as an abnormality of the anterior glenoid rim characterized by a visible osseous fragment. The “cliff” sign is defined as a loss of the normal anterior triangle without a visible osseous fracture fragment. The “blunted angle” sign is defined as a rounding off of the normally sharp anterior angle of the triangle.
If a bone defect in the glenoid is shown with X-ray projections, it is important to determine the area and the percentage of the bone loss. In the past, the shape of the inferior glenoid has been described as a circle. Using this circle method with a 3D CT, spiral CT (Fig. 22.6), or MRI, it is possible to measure the bone defect of the glenoid. For detecting the lesions and the quality of the articular soft tissue, arthro-MRI and arthro-CT are needed.
Classification
Patients with anterior shoulder instability can be classified as having recurrent dislocations, recurrent
subluxations, or an unstable painful shoulder. The incidence of bony lesions of the glenoid is higher in shoulders with a prior dislocation than in shoulders with a prior subluxation, and more common in shoulders with a prior subluxation than painful unstable shoulders. Using the classification of Rockwood and Matsen, the TUBS instability types are more likely to have glenoid bone defects than AIOS or AMBRI instability types. No clear classification system or guidelines exist to preoperatively select patients for arthroscopic or open shoulder stabilization.
subluxations, or an unstable painful shoulder. The incidence of bony lesions of the glenoid is higher in shoulders with a prior dislocation than in shoulders with a prior subluxation, and more common in shoulders with a prior subluxation than painful unstable shoulders. Using the classification of Rockwood and Matsen, the TUBS instability types are more likely to have glenoid bone defects than AIOS or AMBRI instability types. No clear classification system or guidelines exist to preoperatively select patients for arthroscopic or open shoulder stabilization.
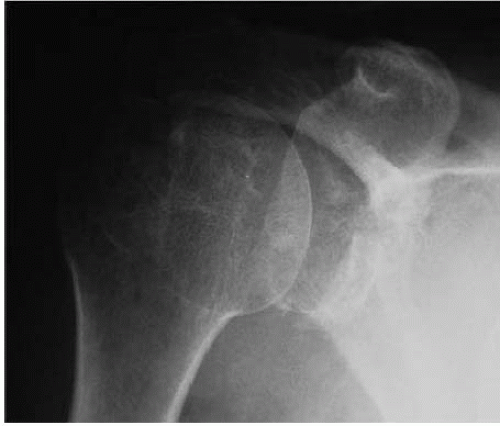 FIGURE 22.4. X-ray AP view: fracture with the loss of the anteroinferior sclerotic contour of the glenoid. |
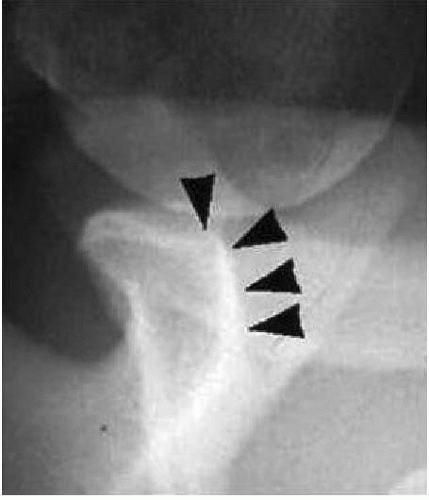 FIGURE 22.5. X-ray Bernageau view: loss of the anteroinferior sclerotic contour of the glenoid. Cliff sign positive (loss of the normal anterior triangle without a visible osseous fracture fragment). |
Decision-Making Algorithms
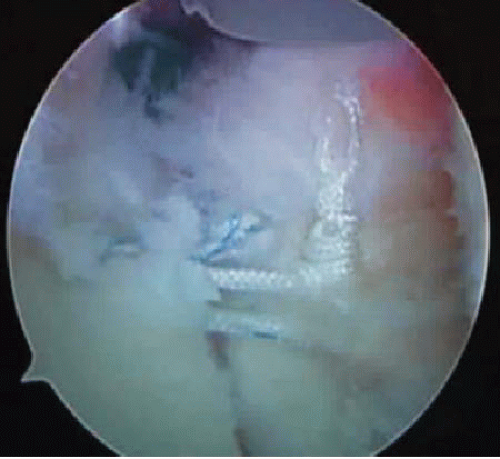
Treatment algorithms depend on many factors, but the size and type (fragment or erosion) of the glenoid bone defect are paramount. If a mobile bone fragment is associated with the labral lesion, then despite the fragment size, the possibility for an arthroscopic reattachment exists (Fig. 22.7). If bone loss is present, no precise guidelines exist. If the percentage of bone loss is greater than 20% of the area of the intact contralateral glenoid, a bone grafting procedure (either open or arthroscopic) to fill the defect and restore the glenoid arc is recommended by most authors. If the missing glenoid area is less than 10% and there is no patulous soft tissue, an arthroscopic soft tissue reconstruction to restore joint stability is certainly an option. If the bone loss is between 10% and 20%, other factors should be considered. Certainly, a coexisting Hill-Sachs lesion could constitute an indication for a bony procedure. Table 22.1 outlines the treatment options based upon these factors.
In addition to an accurate preoperative assessment of a possible bone defect, other risk factors that could preclude arthroscopic soft tissue stabilization must be evaluated. If the instability severity index score (ISIS) (Table 22.2) is more than six points, an isolated soft tissue reconstruction could be insufficient to stabilize the shoulder.
In summary, the careful preoperative assessment of bony lesions, the ISIS scoring system, physical examination, and history may help the surgeon select patients who will benefit from arthroscopic anterior soft tissue stabilization and those who will not.
TREATMENT
Nonoperative
A great deal has been written on the management of anteroinferior shoulder dislocation. The shoulder should be protected against distraction for 6 weeks. One recent approach
calls for constant immobilization of the shoulder in a sling in external rotation for a period of 6 weeks. As soon as the pain has subsided, the patient is started on a shoulder girdle rehabilitation program that includes strengthening of the deltoid, the scapular muscles, and the rotator cuff.
calls for constant immobilization of the shoulder in a sling in external rotation for a period of 6 weeks. As soon as the pain has subsided, the patient is started on a shoulder girdle rehabilitation program that includes strengthening of the deltoid, the scapular muscles, and the rotator cuff.
Table 22.1 Decision-Making Algorithms for Operative Indications in Shoulder Instability | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Nonoperative treatment for an athlete often is chosen based upon the specific sport’s season. Operating on an athlete in the middle of the season can be a difficult choice, and surgery could be delayed until the end of the season. This may be less than ideal particularly if significant bony lesions are present. However, the decision should be made only after a comprehensive discussion of the injury, its prognosis, and the potential consequences of the various treatment options by the physician with the athlete, the coach, and the family.
Operative Indications
Individuals who sustain a dislocation as the result of significant trauma and who do not have generalized ligamentous laxity are more likely to benefit from surgical treatment. Recurrence of instability represents the leading complication of anterior shoulder stabilization. Currently, most surgeons use suture anchor techniques for arthroscopic soft tissue stabilization because of the more reproducible results. However, even with recent technical advances, a recurrence rate between 5% and 20% still persists. The best way would be to preoperatively identify patients whose risk factors preclude arthroscopic stabilization. Numerous prognostic factors have been reported in the literature. Younger patients are at risk, but no clear age limit is identified. Athletes who participate in contact or collision sports have higher recurrence rates after standard arthroscopic stabilization. Finally, patients with significant glenoid bone loss, which result in unacceptably high rates of recurrent dislocation and subluxation after arthroscopic soft tissue repair, are candidates for arthroscopic “bony procedures.”
Table 22.2 Instability Severity Index Score (ISIS) | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree