Arthroscopic Setup: Approaches and Tips for Success
Richard L. Angelo
PATIENT POSITIONING
The safety and ease with which an arthroscopic shoulder procedure is accomplished frequently relates to how the patient is positioned and how accurate and utilitarian are the portals that have been established. Although minor variations exist, most surgeons employ either the lateral decubitus or the beach chair positions, and each has its proponents. The choice is largely influenced by the familiarity gained while the surgeon was learning shoulder arthroscopy, the ease and anticipated likelihood of converting to a mini-open procedure, and the availability of surgical assistants and supportive devices for arm positioning. Equipment is readily available to facilitate the use of either position.
Lateral Decubitus Orientation
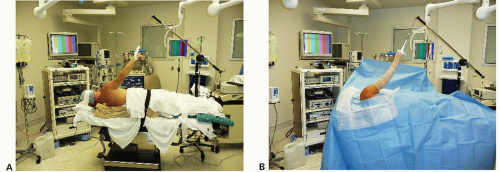
The supine position is used during the induction of general anesthesia. The patient is then repositioned in the lateral decubitus orientation on a vacuum bag (Fig. 1.1A, B). A gel pad can be layered on top of the bean bag, particularly if there is the anticipation that the procedure may be prolonged. A soft axillary roll is placed beneath the upper thorax to minimize direct pressure on the axilla, and the head is supported in a neutral orientation. The patient is allowed to roll back approximately 15° orienting the glenoid parallel with the floor. The vacuum bag is then evacuated to maintain support. All bony prominences must be appropriately padded, in particular the fibular head to protect the peroneal nerve. The operating table is then rotated to position the anesthesiologist and necessary equipment in an area near the middle of the operating table near the patient’s abdomen. The surgeon is thus provided with unrestricted access to the involved shoulder. Monitors are located for easy viewing.
If the primary procedures are to be performed in the subacromial region, that is, rotator cuff repair, the primary monitor is positioned superior and anterior to the patient’s head. A secondary monitor for use by the surgical assistant may be located in front of and above the patient’s abdomen. When the work to be completed is primarily in the glenohumeral joint, that is, a Bankart or SLAP repair, the monitor is set across from the surgeon near the patient’s abdomen as the general viewing direction for glenohumeral procedures is anterior. The arm is supported in 30° to 40° of abduction and 15° of forward flexion using 10 lb (4.5 kg) to suspend rather than place significant traction on the arm. This shoulder position is varied during the case depending on the access necessary to specific locations. Numerous sterile sleeves and gauntlet devices are commercially available to support the arm.
Arthroscopic Bankart repairs may be facilitated by directing 10 lb (4.5 kg) of accessory traction laterally (perpendicular to the humerus) to distract the shoulder and improve access to the anterior aspect of the glenohumeral joint. Alternatively, a similar manual maneuver can be accomplished by an assistant. A routine sterile prep and drape are then performed. The lateral decubitus method eliminates the need for an assistant or mechanical device to support the arm. Internal and external rotation of the suspended arm affords acceptable access to the entire rotator cuff. If range of motion is to be assessed, that is, at the completion of a Bankart repair, the arm is removed from suspension for the motion exam while maintaining sterility of the sleeve suspension loop.
While working in the glenohumeral joint, the monitor view of the glenoid is typically oriented parallel with the floor. When working in the subacromial space, however, the surgeon may elect to either maintain this orientation (the acromion is vertical) or rotate the camera head to view the acromion in a position parallel with the floor (as it would appear with the patient standing).
If converting to an open procedure through a standard deltopectoral approach for the glenohumeral joint, subscapularis, or biceps tendon, the unsterile portion of the suspension apparatus is removed and the patient’s arm is allowed to rest on the ipsilateral hip. The vacuum bag is at least partially inflated (softened) and the patient allowed to roll back into a more supine position. A draw sheet is used to center the patient on the operating table. The table is then configured to a gentle beach chair orientation with acceptable position and support for the head and neck
verified. Although it is unnecessary to completely reprep and redrape, it is prudent to replace the clean, sterile barrier sheet anterior to the shoulder to shield the anesthesiologist and related equipment.
verified. Although it is unnecessary to completely reprep and redrape, it is prudent to replace the clean, sterile barrier sheet anterior to the shoulder to shield the anesthesiologist and related equipment.
If the surgeon elects to convert to a mini-open approach to the subacromial region, repositioning is unnecessary although some prefer to tilt the table posteriorly toward the surgeon to improve access to the anterior shoulder. An approach to the supraspinatus and infraspinatus is readily obtained by extending the lateral subacromial (LSA) portal proximally. An absorbable suture is introduced transversely through the deltoid at the inferior extent of the portal defect to prevent inadvertent distal extension and iatrogenic injury to the axillary nerve. The deltoid is then divided proximally along its fibers to the level of the acromion.
Beach Chair Orientation
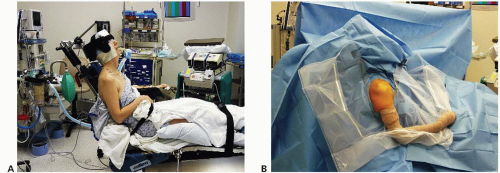
Some surgeons prefer the beach chair position due to its more anatomic orientation, which conforms to the familiar open approach (1). The patient’s thorax is positioned to permit the involved shoulder to overhang the side of the table. Once the hips are flexed 70° to 80° and the legs 30°, the back is then elevated approximately 70°. After padding bony prominences, a vacuum pack supports the hips and thorax, but is displaced from the ipsilateral periscapular region.
Alternatively, a specially designed table with a removable wing for exposure of the operative shoulder may be employed (Fig. 1.2A, B). A relatively more vertical orientation for the back will minimize the dependent position of the camera when the scope is in the posterior portal and also minimize lens fogging. However, a more upright position for the thorax increases the hydrostatic pressure gradient between the head and the brachium. The anesthesiologist sets up near the patient’s uninvolved shoulder, and the viewing monitor is placed opposite the surgeon near the foot of the table. A surgical assistant or a sterile, maneuverable mechanical arm holder adjusts the position of the shoulder during the procedure, depending on the access necessary. Somewhat greater mobility of the arm exists when compared with the lateral decubitus position.
The upright (anatomic) orientation for the arthroscope and monitor view is maintained while working in both the glenohumeral and the subacromial regions. Conversion to an open procedure for all regions of the shoulder is relatively simple and only requires reducing the degree of thorax elevation. The vacuum pack must be at least partially inflated in order to safely change the patient’s position without creating pressure points. Alternatively, a relatively more supine position for the thorax can often be accomplished by tilting the entire table into greater Trendelenberg.
A recent case report identified four patients who underwent shoulder surgery in the sitting position, which resulted in one death and three patients with severe brain damage (2). Cerebral hypoperfusion, rather than cardiovascular risk factors, was believed to be the cause and may be attributable to differences in blood pressure reference points. A blood pressure difference as great as 90 mm Hg between the head and the calf may exist in the sitting position based on hydrostatic factors alone. Potentially catastrophic cerebral hypoperfusion may be avoided by precautions including placing the blood pressure cuff on the brachium rather than the calf (3), maintaining perioperative blood pressure values at a minimum of 80% of preoperative resting values, and ensuring that the intraoperative blood pressure is at a minimum of 100 mm Hg at the level of the head. Loss of vision and ophthalmoplegia have also been reported following general anesthesia with the patient in the beach chair position, but the exact mechanisms for this pathology are unclear (3). Thromboembolic events are also possible with the patient in the sitting position and make the use of cyclical pneumatic compression cuffs around the calves prudent.
ANESTHESIA CHOICES
General Anesthesia
Both endotracheal intubation and a laryngeal mask airway (LMA) provide safe, reliable options for maintaining the airway during general anesthesia. No durable analgesia is afforded once the patient awakens, and nausea/vomiting can sometimes be difficult to manage in the perioperative period.
Interscalene Regional Block
Interscalene blocks (ISBs) provide anesthesia, muscle relaxation, and postoperative analgesia although supportive parenteral pain medication may be necessary during the immediate postoperative period (4). An ISB can be used as the primary means of anesthesia or as an adjunct to general anesthesia. As with any invasive procedure, the risk/benefit ratio determines its use. Proponents note its effectiveness despite the frequent need for some additional narcotic support during the immediate postoperative period and its relatively low risk of serious complications. Dedicated anesthesia teams committed to regional anesthesia and that perform a large number of blocks will be helpful to minimize untoward events (5). Potential serious complications have been reported including cardiac arrest, grand mal seizures, hematoma, and pneumothorax. Possible neurologic injuries include damage to the recurrent laryngeal, vagal, and axillary nerves. Phrenic nerve dysfunction is common and can give rise to significant respiratory distress. Brachial plexus pathology may include transient paresthesias (which have been reported to be as high as 9% at 24 hours and 3% at 2 weeks post-op) (6), or a brachial plexus palsy, which may be transient, require prolonged recovery or be permanent in a very small number of cases.
It is essential that the block be performed in the awake patient who is able to provide critical feedback during administration of the block. More recently, the use of ultrasound to guide placement of the needles has added a measure of safety. Even with a successful block, the duration of pain relief averages only 9 to 10 hours following surgery, which may make pain management challenging in an outpatient setting (4). A thorough disclosure of the potential risks should be discussed with the patient, preferably beforehand in an office setting during the preoperative visit.
Adjunctive Pain Management
The suprascapular nerve supplies 70% of the sensation to the shoulder joint. Instillation of 20 cc of 0.25% bupivacaine adjacent to the suprascapular nerve may result in up to a 30% reduction in postoperative narcotic usage and a five-fold reduction of nausea (7, 8). This block carries a low risk when performed with a blunt-tipped needle, and may be repeated as necessary, even in an office setting on the first postoperative day (9). In addition, local infiltration of the portal sites with 0.5% bupivacaine leads to further reduction in pain. Pain pumps remain controversial, but have been consistently used in the subacromial space with safety provided that the glenohumeral joint is not exposed to the catheter and infiltrate. Cooling jackets using circulating ice water may also substantially improve patient comfort.
PORTALS
When arthroscopic portals are properly placed, they will provide the necessary field of view and instrument access to desired locations within the glenohumeral joint, acromioclavicular joint, and subacromial space (10, 11, 12, 13 and 14). A thorough knowledge of the regional anatomy, particularly the palpable bony landmarks, will improve safety and ensure accuracy in establishing the desired portals. There is a greater margin of safety in creating access to the subacromial space where the use of various accessory portals is routine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree