Labral (Including Slap) Lesions: Classification and Repair Techniques
Jay H. Rapley
Alan F. Barber
KEY POINTS
Superior labral injuries can be confused with normal variations or degenerative changes.
Clinically significant superior labrum anterior and posterior (SLAP) lesions are most commonly found in throwing athletes or after shoulder dislocations.
Glenohumeral arthritis and full thickness rotator cuff tears do not accompany true type II SLAP injuries.
Described physical examination maneuvers and provocative tests provide inconsistent results and are not consistently accurate.
An MRI with gadolinium can define labral anatomy and is a commonly chosen diagnostic imaging study.
Posterior type II SLAP injuries commonly demonstrate a “peel back sign” during which the posterior superior labrum “peels back” off the glenoid rim when the arm is abducted to 90° and externally rotated.
Three specific findings associated with significant superior labral pathology include sublabral fraying, superior glenoid chondromalacia, and injury to the superior glenohumeral ligament (SGHL).
Injuries to the biceps tendon attachment to the superior glenoid labrum can be chronic and can often present subtle findings. This type of injury was originally described in throwing athletes by Andrews et al. in 1985 (1). The initial classification system of what has come to be called SLAP lesions was defined in 1990 by Snyder et al. (2) and has been expanded by others over time (3, 4). Although these classifications present an organized approach to the defining SLAP pathology, the challenge is to diagnose these lesions preoperatively and to differentiate significant superior labral pathology from the many normal anatomic variations which exist. Compounding this challenge are the normal changes that occur to the labrum with increasing age. Reflecting this variability, the accepted mechanisms of injury are as varied as the different types of SLAP pathology. This chapter presents the current SLAP tear classifications and an organized approach to their diagnosis and treatment. Clinical pearls are included to enhance an understanding of SLAP pathology and identification.
CLINICAL EVALUATION
Pertinent History
Clinically significant SLAP lesions are most commonly found in throwing athletes or after a specific traumatic event. These athletes often describe a long overhead throwing history starting as a child and may demonstrate significant humeral retroversion. The most prevalent complaints include anterior shoulder pain, clicking and popping in the shoulder, and reduced function (including decreased speed and power). Not uncommonly, patients will present because of pain with attempted overhead activities, decreased velocity in throwers (sometimes referred to as the “dead arm syndrome”), or increasing lap time in swimmers. In overhead throwing athletes, the symptoms may appear suddenly or over time.
SLAP lesions have various mechanisms of injury with no one specific mechanism predominating. These include falling on the outstretched arm creating shearing forces on the superior biceps labral complex, a tight posterior capsule, a sudden forced abduction and external rotation of the shoulder as might happen when a baseball runner slides head first into base, acceleration of the arm during the late cocking phase, a biceps traction overload caused by the long head of the biceps acting as a decelerator of the arm during the follow through phase of throwing, and the forces applied during a motor vehicle accident by a shoulder-lap belt restraining the ipsilateral chest wall causing the shoulder to roll around the seat belt on impact (5, 6).
The main difficulty for the clinician is differentiating a clinically significant superior labral injury (a real SLAP) from degenerative changes or normal variations. The patient’s history is a key element during the decision-making process. In addition, the physical exam and mechanism of injury should be consistent with a SLAP lesion. Preoperative imaging studies are also helpful but can provide false-positive results and should not be the sole basis for the diagnosis.
Patient selection is the most important factor. It is important to understand which patients are likely to develop
a true SLAP injury and those who are not. Age is an important consideration when determining whether a superior labral abnormality is actually symptomatic. Patients older than 40 years often have naturally occurring degenerative changes, which can be confused with pathologic injury (Fig. 14.1). This “senescence pattern” is seen in the superior labrum and can include labral separation as well as fraying. This can be a normal aging pattern and these changes are unlikely to cause symptoms. Pfahler et al. showed that there is a natural evolution of labral degeneration over time (7). A microscopic and macroscopic analysis of normal shoulders stratified by age demonstrated age-dependent changes at the labral attachment. Three stages were described: those younger than 10 years had a circumferential attachment; those between 30 and 50 years of age demonstrated fissuring and the development of sublabral recesses; and those older than 60 years demonstrated circumferential tearing, fissuring, and labral detachment.
a true SLAP injury and those who are not. Age is an important consideration when determining whether a superior labral abnormality is actually symptomatic. Patients older than 40 years often have naturally occurring degenerative changes, which can be confused with pathologic injury (Fig. 14.1). This “senescence pattern” is seen in the superior labrum and can include labral separation as well as fraying. This can be a normal aging pattern and these changes are unlikely to cause symptoms. Pfahler et al. showed that there is a natural evolution of labral degeneration over time (7). A microscopic and macroscopic analysis of normal shoulders stratified by age demonstrated age-dependent changes at the labral attachment. Three stages were described: those younger than 10 years had a circumferential attachment; those between 30 and 50 years of age demonstrated fissuring and the development of sublabral recesses; and those older than 60 years demonstrated circumferential tearing, fissuring, and labral detachment.
The identification of a pathologic SLAP lesion is seldom an unexpected or incidental finding at the time of arthroscopy. Glenohumeral arthritis or full thickness rotator cuff tears do not accompany symptomatic true type II SLAP injuries. If these degenerative conditions are present, then the superior labral variation is most likely also part of the degenerative process and a surgical procedure to attach the labrum to the superior glenoid is unlikely to provide any clinical benefit.
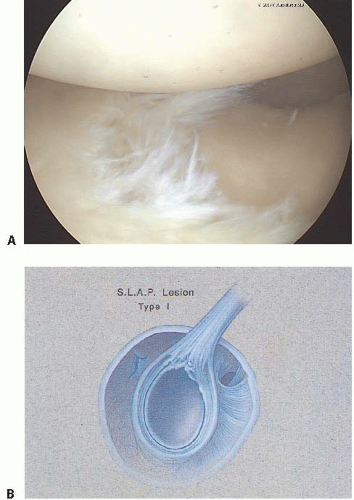 FIGURE 14.1. Patients older than 40 years often have naturally occurring degenerative changes classified as a type I SLAP lesion (photo A), which can be confused with pathologic injury (drawing B). (Photograph Figure 1A © F. Alan Barber MD.) |
SLAP injuries are most commonly found in the dominant arm of male patients younger than 40 years who have participated for many years in high-performance overhead or throwing activities. Another subgroup includes patients with previous shoulder trauma or instability. A history of a shoulder dislocation, a fall on an outstretched hand, or a motor vehicle accident during which the patient was wearing a shoulder lap belt over the involved shoulder are also suggestive of a SLAP injury (8).
Physical Examination
Several physical examination tests have been described to assist in diagnosing significant SLAP lesions. These tests usually apply stress during shoulder manipulation to the biceps anchor using torsion or tensile loads to recreate pain.
The O’Brien’s test (9) positions the arm in 10° to 15° adduction and 90° of forward flexion. With the patient’s thumb pointing toward the floor (full forearm pronation), the patient resists the examiner’s downward pressure on the wrist of the outstretched arm (Fig. 14.2). Following this maneuver, the hand is fully supinated with the palm facing up and the examiner again applies pressure on the wrist while the patient resists. Pain in the shoulder with forearm pronation that is relieved in supination is considered a positive test and suggestive of a SLAP lesion. Tenderness at the acromioclavicular joint combined with local tenderness to palpation indicates AC joint pathology.
In both instances, a positive test consists of less pain with the palm up position than the thumb down position.
In both instances, a positive test consists of less pain with the palm up position than the thumb down position.
 FIGURE 14.2. The O’Brien’s test (9) positions the arm in 10° to 15° adduction and 90° of forward flexion. With the patient’s thumb pointing toward the floor (full forearm pronation), the patient resists the examiner’s downward pressure on the wrist of the outstretched arm. (Photograph © F. Alan Barber MD.) |
When bicipital tendonitis is present, a positive Speed’s test is elicited when pain is produced at the anterior bicipital groove by resisted forward flexion with the shoulder flexed at 90° and the forearm fully supinated.
A reduction in internal rotation when compared with the opposite shoulder is suggestive of a tight posterior capsule (Fig. 14.3). This reduction in internal rotation is suggestive of a SLAP injury especially if it is not resolved by a course of physical therapy. An accurate determination of internal rotation can be made with the patient supine and the examiner stabilizing the scapula by pressure on the anterior shoulder. The arm motion measured with a goniometer should be 180°. Long-term throwing athletes may develop humeral retroversion in which case, the dominant arm will demonstrate increased external rotation with a resultant decrease in internal rotation.
The previously mentioned provocative tests and others often provide inconsistent results and are often not independently diagnostic. The modified O’Brien’s test, crank test, and anterior slide test have not been widely supported as solely diagnostic (10, 11 and 12). The relocation test of Jobe was shown to be accurate in the hands of some individuals but not others. The biceps load test and the pain provocative test can be helpful in addition to other tests, but have not been validated independently. Despite the concerns about reliability of these tests (10, 11 and 12), they do play a role in the physical examination of the shoulder.
Imaging
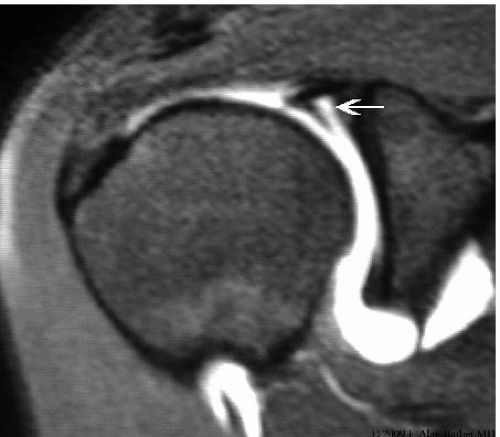
Diagnostic imaging may not be consistent for the identification of SLAP tears. Plain radiographs should be a mainstay to determine if there is any associated bony pathology. MRI with the addition of gadolinium enhances the anatomy of the superior labrum (Fig. 14.4), and interpretation by a musculoskeletal radiologist improves its accuracy. Community read scans were reported to have an accuracy of only 51%, but they were significantly more sensitive if an arthrogram was done in addition with the MRI (13). When reading the same studies, two fellowship-trained musculoskeletal radiologists increased the accuracy by 10% to 20%, but were still limited in their accuracy, sensitivity, and specificity (13).
 FIGURE 14.3. A decrease in internal shoulder rotation when compared with the opposite shoulder is suggestive of a tight posterior capsule. (Photograph © F. Alan Barber MD.) |
Variations within the anatomy of the superior labrum have been identified which confound the diagnostic accuracy of this test. A normal sublabral separation from the glenoid surface is common and this may vary from a slight crease to a sulcus measuring 1 to 2 mm or more. These are not pathologic but may be filled in magnetic resonance arthrography. The presence of such a sulcus does not define a pathologic SLAP lesion. In contrast, the presence of a ganglion or sublabral cyst, often associated suprascapular nerve (SSN) compression, is very suggestive of a SLAP lesion (14, 15). Again, MRI should be used as an adjunct for diagnosis of a SLAP lesion and not relied upon independently.
Even among the “experts,” there is a lack of consensus on making a SLAP diagnosis. The intraobserver and interobserver reliability for the diagnosis and treatment of various SLAP tears was greater than 50% among 70 experienced shoulder arthroscopic surgeons (16). Yet arthroscopy is considered one of the principal diagnostic tools for this condition.
Classification System
With the advancement of arthroscopy equipment and improved techniques, SLAP lesions have been better delineated from normal anatomy. The classification of SLAP
lesions has undergone expansion over the last 20 years by other authors beyond the initial description (2, 3 and 4). A type I SLAP is considered by some to represent normal degenerative changes and the retreat of blood supply from the superior labrum that comes with increasing age and consists of fraying on the inner margin of the superior labrum (Fig. 14.1). Sometimes a larger meniscus-like superior labrum (meniscoid labrum—a normal variant) displays similar degenerative fraying of the inner rim and can also be considered a type I SLAP.
lesions has undergone expansion over the last 20 years by other authors beyond the initial description (2, 3 and 4). A type I SLAP is considered by some to represent normal degenerative changes and the retreat of blood supply from the superior labrum that comes with increasing age and consists of fraying on the inner margin of the superior labrum (Fig. 14.1). Sometimes a larger meniscus-like superior labrum (meniscoid labrum—a normal variant) displays similar degenerative fraying of the inner rim and can also be considered a type I SLAP.
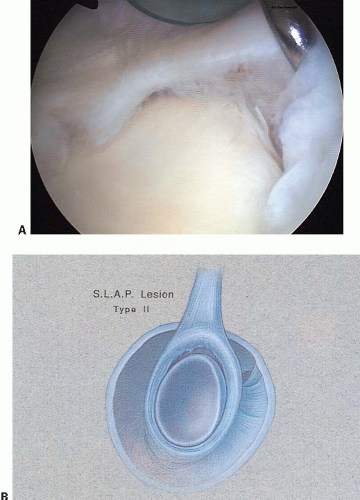 FIGURE 14.5. The type II SLAP (photo A) occurs when the superior labrum at the attachment of the biceps tendon pulls off the superior glenoid tubercle (drawing B). (Photograph A © F. Alan Barber MD.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|