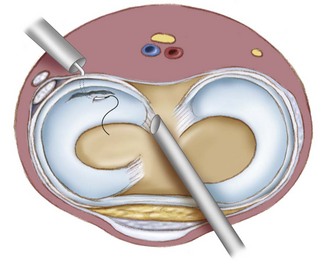
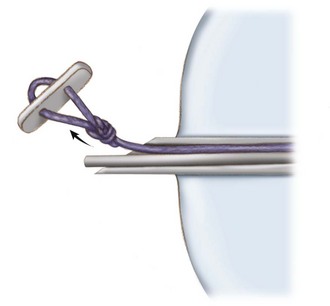
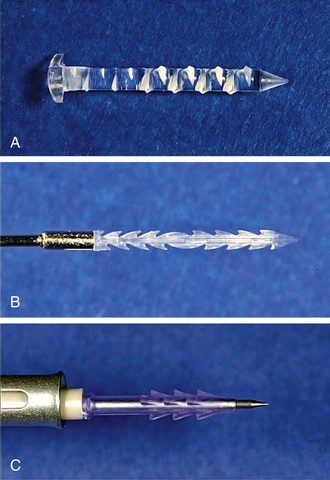
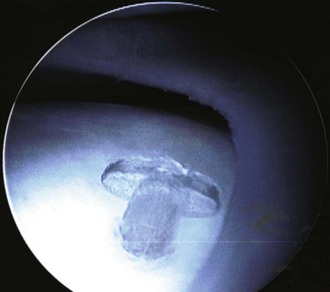
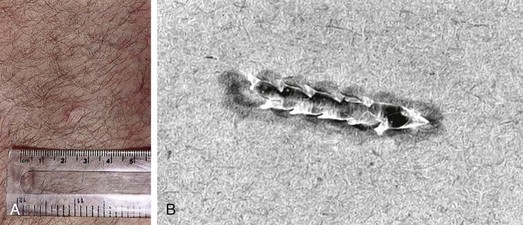
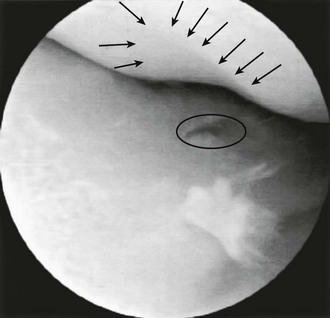
Chapter 55 Morgan first described all-inside meniscal repair in 19911 when he used curved suture hooks and accessory posterior portals. Although these initial results demonstrated that all-inside meniscal repairs could be highly successful, they were technically difficult and required accessory incisions. Since this initial description, there has been a significant evolution with regard to surgical techniques and implant designs. Magnetic resonance imaging can be more than 96% accurate in identifying meniscal lesions and may be used to help confirm their presence.2 However, it has not yet been shown to be helpful in predicting whether a tear is reparable.3 The decision for repair versus partial resection usually requires arthroscopic assessment. Many factors play a role in meniscal treatment decision making: Longitudinal, peripheral (vascular) tears in the red-red or red-white zones are the most amenable to repair. If there is ligamentous instability, it should be addressed at the time of meniscus repair, if possible, or in the near future if the procedure must be staged. As with other forms of repair, the all-inside technique yields better results with acute, traumatic tears and in those knees undergoing concomitant anterior cruciate ligament (ACL) reconstruction.4 Tears that are stable with less than 3 mm of displacement with probing and that are less than 1 cm in length can be left in situ with predictable results. Relative contraindications to an all-inside repair include the following: • The anterior horn may not be accessible through anterior portals with any of the available all-inside devices. • There must be a meniscal rim intact for the anchoring mechanisms of these devices to work appropriately. Hence, meniscocapsular separations are not suited for all-inside repair devices. • Degenerative tears that have poor potential for healing may be unsuitable. • All-inside devices were developed to be used through standard arthroscopic portals. The second-generation devices had good short-term success rates of 80% to 90%5–7 but, more important, taught surgeons it was possible to safely deliver an all-inside device through standard anterior arthroscopic portals. Unfortunately, the procedures were still somewhat challenging to perform, and the inability to adequately tension the sutures was less than ideal. • Bioabsorbable devices introduced • Meniscal arrows, darts, staples, screws (Fig. 55-3) – These devices captured the torn meniscus and anchored it to the peripheral portion of the meniscus or the capsule. – They were mostly made of rigid poly-L-lactide-acid (PLLA). – Meniscal Arrow (ConMed Linvatec) most popular of the group • Prospective randomized study demonstrated 91% healing at 2 years with ACL reconstruction8 • Same group was evaluated at 6 years9 • Other studies showed overall failure rate of 28% and, when an isolated meniscal repair was performed, a 42% failure rate.10,11 • The various suture configurations that each device allows – Some devices allow a variety of suture configurations including horizontal, vertical, or oblique or a continuous running suture. Other devices allow only a specific suture configuration or only a single point of fixation. • The location and composition of backstops, anchors, or “top hats” that the devices uses • The type of suture material of which each device is composed • The deployment mechanism of the device and whether this is active or passive. – Passively deployed devices are manually pushed into the meniscus, and the implant is left behind when the inserter is removed. Unfortunately, this can lead to implants inserted to the inappropriate depth or implants that dislodge or break during implantation. Actively deployed implants are actively inserted to a specific depth when a lever or trigger or wheel is pulled. This leads to a more consistent depth of implantation and fewer misfires.
Arthroscopic Meniscus Repair
All-Inside Technique
Preoperative Considerations
Physical Examination
Imaging
Other Imaging Modalities
Indications
Contraindications
Surgical Technique
First-Generation Repairs
Second-Generation Repairs
Third-Generation Repairs
Fourth-Generation Repairs
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthroscopic Meniscus Repair: All-Inside Technique