1
Arthroscopic Meniscectomy
Meniscal tears are is a common injury to the knee joint. Poehling et al1 reported two major patterns of meniscal damage (Fig. 1–1):
- Degenerative: horizontal cleavage (12%), flap (21%), complex (30%), generally for older patients
- Traumatic: peripheral tears 3 mm or less from the meniscosynovial junction (26%), radial tears (9%), and tears associated with ligament damage, such as anterior cruciate ligament (ACL) tears. The incidence of meniscal injury following ACL injury ranges from 34 to 92%. Warren and Marshall2 reported that the incidence of meniscal pathology can approach 98% with chronic ACL tears. It is now generally accepted that lateral meniscal tears are more commonly associated with acute injuries and medial meniscal damage with chronic ACL deficiency.
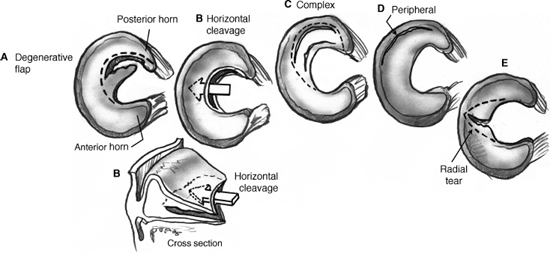
Figure 1–1 Meniscal tear patterns with appropriate level of resection indicated by a dotted line.
Diagnosis
The accurate diagnosis of meniscal pathology requires taking a history and doing a physical examination. Solomon et al3 reported a meta-analysis showing that the accurate diagnosis of a meniscal tear is determined not by a specific maneuver or question but rather by the compilation of the patient’s history and the physical exam findings.
History: The history for meniscal pathology generally involves a twisting injury to the knee, swelling, mechanical symptoms involving clicking, catching, giving way, and pain at the joint line.
Physical exam: Critical elements of the physical exam include the presence of a joint effusion, joint line tenderness, and meniscal compression signs. The McMurray’s test involves having the patient extend a fully flexed knee while internal/external rotation and a valgus force are applied. For the Apley compression and distraction test, the patient is in a prone position, and the knee is flexed to 90 degrees; axial compression is applied through the heel as the lower leg is internally and externally rotated. It is also important to rule out any hip or spine pathology during the physical exam.
Radiograph: Weight bearing, anteroposterior (AP), lateral, and Merchant views are required both to rule out any degenerative joint disease and to assess alignment.
Magnetic resonance imaging (MRI): Although often not necessary to make the diagnosis of a meniscal tear, MRI is useful to assess associated pathology. The MRI accuracy in diagnosing meniscal tears ranges from 91 to 95%.4
Differential Diagnosis
Kitziger and DeLee5 outlined a series of possible differential diagnosis.
Extraarticular
- Spinal hip or neoplastic
- Extremity malalignment
- Reflex sympathetic dystrophy
Intraarticular
- Articular cartilage pathology unrelated to meniscal injury condrofracture or degenerative disease
- Crystalline deposition diseases (gout, calcium pyrophosphate deposition)
- Avascular necrosis of the distal femur of the proximal tibia
- Patellofemoral pathology
Medical Treatment
Nonoperative treatment or initial treatment involves nonsteroidal antiinflammatory drugs (NSAIDs), steroid injection, and physical therapy to concentrate on range of motion and strength of the quadriceps as well as the hamstrings. In cases of degenerative meniscal tears, a steroid injection has excellent success.
Surgical Treatment
Tourniquet
It is generally agreed that a tourniquet should be placed during preparation for surgery. It should be placed as high on the leg as possible, and it should fit snugly but not too tightly. The only time this tourniquet should be inflated is if visualization is a problem; otherwise, it is left deflated. It is important not to cinch the tourniquet, as this could cause a venous tourniquet. Dobner and Nitz6 reported 70% postmeniscectomy electromyogram (EMG) changes in a tourniquet group versus 0% in a non-tourniquet group. The question of clinical significances is always raised; however, it is felt that as long as adequate visualization is achieved, the tourniquet should not be used.
Examination Under Anesthesia
When the patient is under anesthesia, the range of motion, Lachman test, anterior drawer, and pivot shift should be examined to uncover any underlying ligament pathology.
Patient Position
The patient should be placed in the supine position on the operating table with the patient positioned to eliminate excessive lumbar lordosis. A leg holder or lateral thigh post is used to provide better joint access.
Leg Holder
A leg holder is placed on the upper thigh; it produces optimal rotational control of the limb. The contralateral limb is placed in an Allen-type holder, and the bottom of the table is lowered all the way. One of the drawbacks of this approach is that it can be problematic for the superior medial and superior lateral portals.
Lateral Leg Post
The lateral leg post is clamped to the lateral aspect of the table, on the side holding on the involved leg. No contralateral leg positioning is required, and a lateral joint examination maneuver is required, which may reduce blood flow. This maneuver allows easy access to the superior medial and superior lateral portal.
Fluid Management (Inflow and Outflow)
Critical elements in fluid management include:
- Joint distention for visualization
- High-volume flow for shavers and burs
- Intraarticular pressure for hemostasis
Two major types of systems are used today, the gravity system and the pump system. The gravity system is based on Poisson’s law, and the pump system ensures an adequate amount of pressure in the system. The pump system usually provides feedback that does not necessarily require an accessory portal. Generally, this system enters through the arthroscopic sheath, in the outflow portal; if visualization is problematic, the system can be established through a superior medial or superior lateral flow.
Surgical Technique
Instruments (Fig. 1–2)
The basic instruments required for successful arthroscopic partial meniscectomy are:
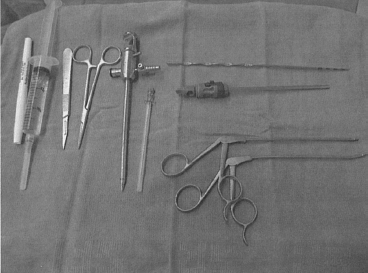
Figure 1–2 Mayo stand with arthroscopic meniscectomy instruments.
- A 30-degree arthroscope with a possible addition of the 70-degree arthroscope if there is difficulty looking into the posterior portion of the knee with the 30-degree arthroscope
- Hand-operating instruments, including a probe that is calibrated or measured by the surgeon, basket forceps of different angles, a grasp for removal of loose bodies, and spinal needles for portal placement and accurate mobilization of the menisci
- Motorized instrumentation including different-size shavers
- Electrocautery
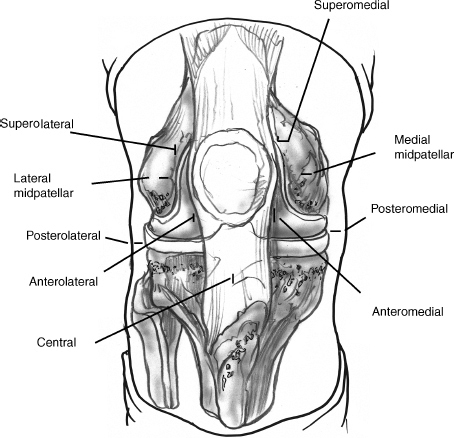
Figure 1–3 Arthroscopic knee portals.
Portals (Fig. 1–3)
Portal positioning is critical for safe and effective arthroscopy. There are advantages and disadvantages to transverse or horizontal portal incisions. Transverse portal incisions, although more cosmetic and less likely to injure sensory nerves, can be more restrictive than longitudinal portals.
The arthroscope is generally placed through an anterior lateral portal, which is just below the inferior pole of the patella and 5 to 10 mm lateral to the patella tendon. The inferior medial portal is created initially or with needle localization. Creating the medial portal in the position of use, usually at 30 degrees of knee flexion for access to the medial side of the knee, prevents the capsule from wandering away from the skin incision, causing difficulty with instrument passing.
Needle localization lowers the risk of condyle or meniscal injury and ensures access to the posterior meniscal segments.
Visualization
Visualization is maximized by keeping the arthroscope as far away from the meniscus as possible. This allows for a more panoramic view. The arthroscope can also be braced gently against the lateral femoral condyle for stability.
Medial Meniscus (Fig. 1–4)
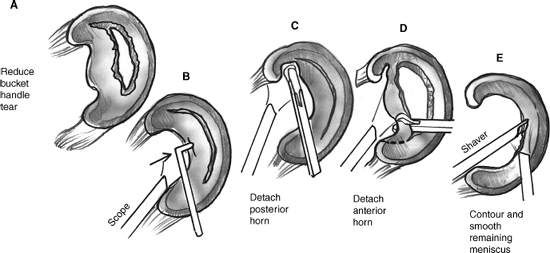
Figure 1–4 Resection of medial meniscus bucket handle tear.
- The meniscus is best viewed in 20 degrees of flexion with valgus force and external rotation stress.
- When approaching the medial compartment from the medial gutter, turn the scope inferiorly to evaluate the meniscosynovial junction.
- The posterior medial joint compartment does not open as readily as the lateral side. It has been reported that only 50% of the posterior horn can be seen. Through this opening, several techniques can be employed:
a. Change the arthroscope to the anterior medial portal.
b. Place the arthroscope on the lateral edge of the medial femoral condyle next to and under the origin of the posterior cruciate ligament (PCL), and push the notch and angle the camera. If you can’t go under the PCL using direct vision, place the blunt trocar and push the posterior knee, and then replace the trocar with the camera.
c. Consider additional portals to enhance visualization.
d. Use a small-diameter arthroscope.
e. Use a 70-degree arthroscope.
The Lateral Meniscus (Fig. 1–5)
If the knee is in the lag holder, a valgus force with the knee in 15 to 20 degrees of flexion and internal rotation should be applied. With this maneuver the entire posterior horn of the lateral meniscus, including the popliteal tendon and sulcus, can be visualized.
- If a lateral post is being used, the leg is brought up and placed into the figure-four position (heel toward opposite knee).
- When visualizing the lateral gutter and popliteal tendon hiatus, it is important to inspect the meniscal synovial junction for peripheral tear.
Indications for Partial Meniscectomy
- A complete longitudinal tear longer than 10 mm7
- Tear with a periphery of 10 to 30% of the meniscus
- Demonstrated instability
- Tear without secondary degeneration
- Tear occurring in a young, active patient
- Tear found during ACL reconstruction
Goals of Partial Meniscectomy
The goals of a partial meniscectomy include:
- Only the torn portion of the meniscus should be removed.
- Trimming and contouring are done to stabilize the remaining rim.
- Preservation of the capsular rim is essential for joint stability; look for a medial meniscectomy in a patient with early onset of degenerative joint disease (DJD).
Technique
Once adequate visualization is achieved, removal of loose, damaged menisci and a balanced resection or contouring of the remaining meniscus are accomplished in a stepwise approach:
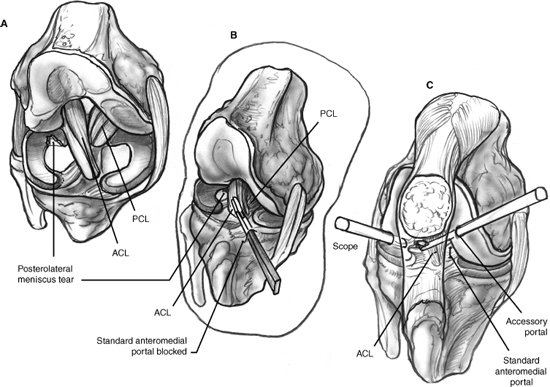
Figure 1–5 Portal placement for resection of a posterior horn tear of the lateral meniscus. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
- There must be a free end of the meniscus fragment for the motorized shaver to be affective.
- Surgeon comfort with portal position and a smooth transfer of instruments to the surgical site are critical in avoiding articular cartilage injury.
- Begin the resection in the hard-to-reach areas.
- If an anterior horn tear is present, create an accessory portal at the medial edge of the patella that points down, and then do the resection.
- If fat pad distress is present, with both the shaver and the arthroscope in the suprapatellar pouch, slowly bring both down the trochlea together until you encounter the fat pad. Start to resect the periphery in a controlled manner until clear visualization is achieved (Fig. 1–6).
- The surgeon should not hesitate to create an accessory portal to allow better angles of access.
- If visualization is difficult, then place a tourniquet and the setup accessory outflow portal. The predictors of successful meniscectomy are a short yet efficient procedure, minimal tourniquet use, and a lack of previous surgery on the operative knee.
Portal Closure
There are many different techniques for portal closure. They include buried absorbable sutures and simple Prolene/nylon sutures, or Steri-Strips. The advantage of using sutures is that the patient is required to return to the office in 7 to 10 days, which gives the physician another chance to go over the operative findings and counsel the patient on physical therapy and the future treatment plan.
Postoperative Care
Pain medication: This includes intraarticular injection of Marcaine as well as consideration of preemptive analgesia, which would include a preoperative NSAID to be taken the night before as well as injection of the portal sites with lidocaine. A narcotic analgesic is prescribed to be taken as needed.
Dressings: A standard absorptive dressing is used with an Ace bandage, which is then removed by the patient at 48 to 72 hours postoperation; the patient is allowed to shower, with no soaking of the wounds. Sutures are removed at 7 to 10 days postoperation, and physical therapy is begun at this time if indicated.
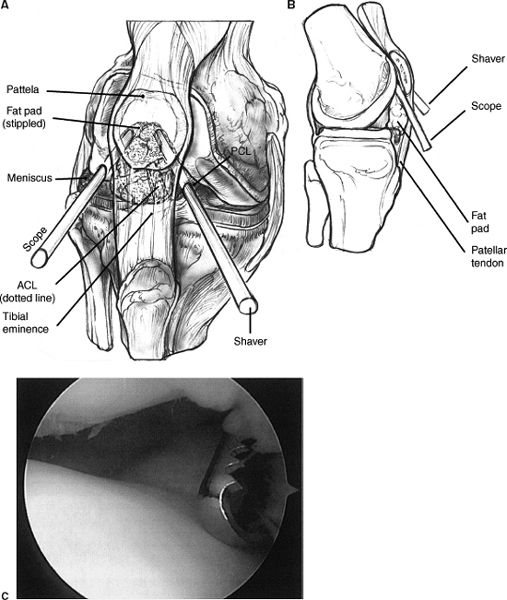
Figure 1–6 Arthroscopic strategy for “fat pad distress.”
Physical therapy: The patient is weight bearing as tolerated with crutches as needed unless some other procedure was performed that requires a modification of this plan. Isometric quad sets, patella mobilization, and active range of motion are begun immediately. Within 48 to 72 hours the dressings are removed by the patient, and the patient is then allowed to shower. If the patient is comfortable, he or she may return to sedentary work within a week. No brace is needed.
References
1 Poehling GG, Ruch DS, Chabon SJ. The landscape of meniscal injuries. Clin Sports Med 1990;9:539–549
2 Warren RF, Marshall J. Injuries of the anterior cruciate and medial collateral ligaments of the knee. A retrospective analysis of clinical records—part I. Clin Orthop Relat Res 1978;136:191–197
3 Solomon DH, Simel DL, Bates DW, Katz JN, Schaffer JL. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA 2001;286:1610–1620
4 Reicher MA, Hartzman S, Duckwiler GR, et al. Meniscal injuries: detection using MR imaging. Radiology 1986;159:753–757
5 Kitziger KJ, DeLee JC. Failed partial menisectomy. Clin Sports Med 1990;9:641–660
6 Dobner JJ, Nitz AJ. Postmenisectomy tourniquet palsy and functional sequelae. Am J Sports Med 1982;10:211–214
7 DeHaven KE, Black KP, Griffiths HJ. Open meniscus repair: Techique and two- to nine-year results. Am J Sports Med 1989;17:788–795.
< div class='tao-gold-member'>









