Fig. 21.1
Volar wrist gangli on cyst

Fig. 21.2
Dorsal wrist gangli on cyst
Patient Evaluation
History and Physical Examination
The majority of patients that present for evaluation of a dorsal wrist ganglion do so secondary to cocerns regarding cosmesis. Ganglions are also associated with pain particularly on wrist extension activities and forceful grip. The volar ganglion may irritate the radial artery and the median nerve along with its palmar cutaneous branch. Occult ganglions are those that present without a palpable mass yet patients report symptoms of wrist pain. These patients present with nontraumatic, nonsystemic inflammatory wrist pain. Often these patients go undiagnosed for a period of time because clinically and radiographically there is no evidence of pathology. Ultrasound or magnetic resonance imaging can aid in the diagnosis. A study that evaluated patients with chronic wrist pain (at least 3 months) using ultrasonographic examination found 58 % of patients had an occult ganglion as the source of their pain [11]. Westbrook looked at the reason patients present to hand clinics with dorsal wrist ganglions and found that 38 % are concerned with the cosmetic appearance, 28 % are concerned that the cyst is cancerous, and 26 % present with pain [12]. A discussion of the etiology, natural history and benign nature of the mass is often enough to alleviate patient fears and the desire for surgical intervention.
When diagnosing a dorsal ganglion cyst, it is imperative to ensure that the mass is truly a ganglion cyst. Many elements of the history and physical examination are not conclusive. Occurrence, progression, size, shape, texture, presence or absence of pain, and association with traumatic or repetitive activities provide little information regarding the true diagnosis. One element of history, however, can be quite helpful in determining whether the lesion is cystic. While ganglion cysts and other tumors get larger, only ganglion cysts decrease in size as well. Exceptions to this include some vascular tumors than involute over a period of months to years; however, ganglion cysts can decrease in size as quickly as overnight. On physical examination, transillumination can be helpful to differentiate a ganglion cyst from an alternative tumor. This is performed by holding a penlight to the lesion and observing the light transmit through its fluid medium, whereas a solid tissue tumor will prevent any propagation of the light.
Occasionally, ganglion cysts may herald underlying pathology, such as a scapholunate ligament injury. The history and physical examination should focus on any recent or remote trauma. Often, patients have incompetent scapholunate ligaments that remain clinically unapparent until the manifestation of an associated dorsal ganglion cyst. One study reported on 19 wrists with painful dorsal ganglia, a positive Watson scaphoid shift test and negative radiographs that underwent ganglion excision. Postoperatively, all patients had decreased pain and 17 of the wrists had a postoperative negative Watson shift test [13]. Tenderness during palpation of the dorsal portion of the scapholunate ligament, a positive radial scaphoid shift test, or a positive straight finger resistance test may suggest scapholunate ligament pathology. Furthermore, ganglion cysts may resemble other pathologies, such as a gouty tophus, tenosynovitis, or rheumatoid pannus. A careful history and physical examination should suffice to differentiate these conditions.
Diagnostic Imaging
Magnetic resonance imaging (MRI) and ultrasonography remain the imaging modalities most commonly utilized to differentiate fluid-filled cysts from solid tumors. A study comparing the diagnostic abilities of ultrasound versus magnetic resonance imaging to detect occult wrist ganglions showed they are equally effective [14]. Nevertheless, there has been a shift toward ultrasonography as the preferred technique, given its readible availability, quickness, and lower cost. Very small ganglion cysts, known as occult ganglion cysts, although clinically significant, can be easily missed by either imaging modality. Surgeons should keep a high index of suspicion for occult ganglion cysts, even in the face of a negative reading by the radiologist. With intraoperative arthroscopic diagnosis of occult ganglia as the standard, the sensitivity of MRI scanning was found to be only 83 % and the specificity only 50 % [15].
Treatment
Nonoperative Management
The initial treatment of choice is a trial of nonoperative management, including splinting for comfort, prior to proceeding to operative intervention. However, the results of conservative treatment are unpredictable with success rates ranging from 30 % to 85 % [7]. Attempted aspiration can safely be performed on the dorsum of the wrist but attempts to aspirate volar ganglion cysts may cause injury to neurovascular structures, such as the radial artery and palmar cutaneous nerve. Adjunctive measures, such as steroid injections, sclerosing injections, and multiple cyst punctures, have been reported but show results no better than expectant management and, furthermore, carry up to a 5 % complication rate [7].
Operative Management
Surgical excision remains the treatment of choice for carpal ganglion cysts refractive to conservative measures. Prior to the recognition of the ganglion stalk, recurrence rates rivaled those of expectant management but now are reported to be as low as 1 % [8]. However, surgical intervention is not without risk and complications, which although rare, include recurrence, infection, neuroma, keloid, scar hypersensitivity, postoperative stiffness, grip weakness, and scapholunate instability.
Indications for surgical intervention include symptomatic ganglia that produce pain, weakness or limitations in wrist function/range of motion. Unacceptable cosmesis is also an indication, but typically additional symptoms are necessary for us to recommend proceeding to operative intervention.
Many patients seek excision of their ganglion for cosmetic reasons or concern that the mass is malignant. Although an open incision across the dorsum of the wrist may not seem excessive to a surgeon, the patient may have another perspective. One study reported a very high postoperative satisfaction rate after arthroscopic excision, despite the fact that 17 % of the patients were asymptomatic preoperatively and opted for surgery for cosmetic reasons [6]. The implication is that offering arthroscopic ganglion resections for patients primarily interested in the cosmetic appearance of their hands is reasonable. However, while surgical excision of the cyst will remove the “bump,” a scar will replace the “bump.” Arthroscopic excision of the cyst has the potential to remove the “bump” with minimal scarring.
Arthroscopic Technique
The patient is placed supine on the operating room table and a non-sterile pneumatic tourniquet is applied to the upper arm (Fig. 21.3) (Video 21.1). Subsequently, the remainder of the upper extremity is prepped and draped in the usual sterile fashion and the patient is placed in the standard wrist arthroscopy tower. Prior to suspension in the traction tower, it is useful to do a wrist exam under anesthesia. While the patient’s arm is suspended in a traction tower, a 6-R portal is created as a visualization portal, by first placing an 18G needle to ensure appropriate placement of the portal. Once the needle confirmed the correct location, a stab incision is made through the skin only. Blunt dissection is carried out with a hemostat and a capsulotomy is made with the blunt trocar. The arthroscope is now inserted into the joint and directed radially to visualize the stalk of the ganglion at the junction of the fibrous and membranous portion of the scapholunate ligament. The typical initial visualization portal, the 3–4 portal, is avoided as the primary portal to prevent inadvertent decompression of the cyst.
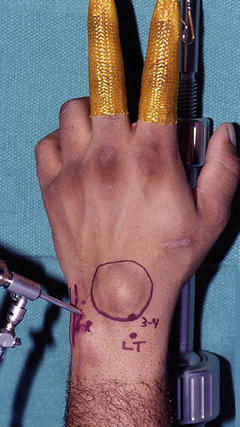
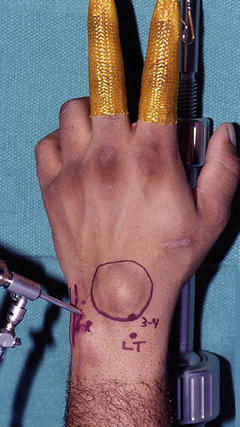
Fig. 21.3
Arthroscopic set up for dorsal ganglion cyst excision
In contrast, with volar ganglion excision the 3–4 portal is established first, as this provides good visualization of the radial wrist ligaments, the common origin of the volar ganglion. The scope is then introduced through the 4–5 or 1–2 portal for visualization during resection of the ganglion through the 3–4 portal. The radial artery and sensory branch of the radial nerve need to be protecting with use of the 1–2 portal [16].
After the 2.7-mm arthroscopic camera is directed toward the dorsal compartment of the wrist, the capsule adjacent to the scapholunate ligament can be visualized. Occasionally, a sessile or pedunculated protrusion into the joint can be seen in the area where the extrinsic capsule joins the distal portion of the dorsal scapholunate ligament. This capsular reflection serves as part of the barrier between the radiocarpal and midcarpal joints, and the protrusion located here has been termed the cystic stalk. More often, the surgeon may be impressed with the amount of synovitis and redundant capsule in this area instead of an actual stalk.
Once the stalk and cyst are visualized, a full radius shaver is placed through the cystic sac using the 3–4 portal. This action decompresses the cyst and may obscure any presence of an intra-articular stalk. If visualization is difficult to establish the 3–4 portal, we recommend finding Lister’s tubercle and moving approximately 1 cm distal to locate the radiocarpal joint. The aforementioned technique of ensuring accurate placement is followed by utilization of an 18G needle followed by making the stab incision, utilization of a hemostat for blunt dissection, and finally inserting the trocar to perform the capsulotomy. A 2.9-mm, full-radius shaver is introduced through this portal, and every effort is made to avoid decompressing the cyst with simple introduction of the shaver.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








