5
Arthroscopic Debridement of the Knee
Arthroscopic debridement is a surgical option in the man agement of degenerative arthritis (Fig. 5–1). It is a minimally invasive procedure suited for an individual with mechanical knee symptoms and a preponderance of synovitis. The goal is to provide symptomatic relief of knee pain rather than alter the course of osteoarthritis. Arthroscopic lavage and debridement can provide improvement in pain for 50 to 70% of patients with appropriate indications. This relief can last from a few months to several years.1–3
The rationale behind the procedure is to debride mechanical irritants inhibiting knee function and to reduce the concentration of potentially harmful cytokines. In osteoarthritis, degenerating cartilage releases cytokines that lead to the secretion of lytic enzymes by chondrocytes. These enzymes can potentially destroy type II collagen and proteoglycans. Lavage of these irritants by arthroscopy may potentially break the destructive cycle and provide symptomatic relief.4, 5 Cartilage disruption can also compromise joint mechanics and may lead to progressive cartilage deterioration. Arthroscopic shaving of damaged cartilage is performed with the intent to decrease joint symptoms. Debridement can remove frayed and fibrillated cartilage, leaving a smoother articular surface.6, 7
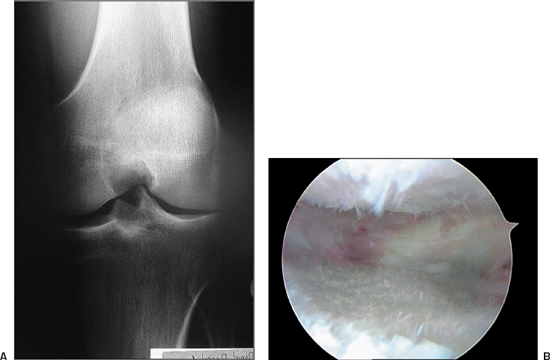
Figure 5-1 (A) Flexion weight-bearing radiograph of a 36-year-old man who is 10 years status post-lateral meniscectomy demonstrating joint space narrowing. (B) Arthroscopic debridement is well suited for arthritic knees with mechanical symptoms, degenerative meniscal tears, and chondral flaps, which can be removed, potentially providing pain relief.
Surgical Indications and Other Options
Surgical Indications
- Onset of symptoms less than 6 to 12 months ago
- Unicompartmental arthritis or normal knee alignment without radiographic evidence of advanced degenerative arthritis
- Overt meniscal symptoms
- Ligamentous stability
- Loose bodies or mechanically significant osteophytes
- Diagnostic tool to determine if patient is a candidate for high tibial osteotomy or unicompartmental joint replacement8
Relative Contraindications
- Onset of symptoms more than 6 to 12 months ago
- Previous arthroscopic debridements within the prior 5 years
- Pain at rest
- Ligamentous instability
- Bi- or tricompartmental degenerative changes
- Lower extremity deformities, either extreme valgus or varus8
Other Options
- Oral medications: Traditional methods for treatment of degenerative arthritis include the judicious use of nonsteroidal antiinflammatory drugs combined with activity modification. Oral agents such as glucosamine and chondroitin sulfate potentially offer some relief in subjective symptoms. Studies indicate that pain, joint tenderness, range of motion, and walking speed may be improved with these medications.9, 10 As of yet, there are no clinical data showing that these oral agents affect the formation of cartilage.11
- Viscosupplementation: Viscosupplementation involves the injection of high molecular weight hyaluronans into the osteoarthritic joint. Despite a paucity of well-controlled studies demonstrating efficacy, viscosupplementation remains an option for nonoperative treatment of degenerative arthritis.11
- Radiofrequency energy: Radiofrequency energy (RFE) has been utilized for the treatment of partial-thickness cartilage defects. These devices grossly appear to contour the area of cartilage loss, providing a smooth transition from abnormal to normal cartilage. An evaluation of chondrocyte viability after bipolar RFE (bRFE) with confocal laser microscopy and standard light microscopy was performed by Lu et al.12 This work indicated that bRFE led to significant chondrocyte death and that these changes were not apparent using light microscopy. The depth of chondrocyte loss was significantly deeper than the chondrocyte loss expected with mechanical shaving. The authors concluded that the in vivo use of bRFE could result in full-thickness cartilage death as well as death to subchondral bone.12 Although reports of adverse events remain anecdotal, the authors believe that the use of RFE for the treatment of chondral disease should be considered investigational at this time.
- Cartilage restoration procedures: There are techniques available for cartilage restoration of localized areas of cartilage loss. In general, these procedures are reserved for focal areas of cartilage loss in otherwise normal knees. They are not indicated for pan-arthritic joints. Examples of these procedures include autologous chondrocyte implantation, osteochondral auto- and allografts, abrasion arthroplasty, and microfracture. Each necessitates a specific postoperative rehabilitation protocol to optimize results. The decision to use these modalities depends on the activity level and age of the patient, as well as the depth, size, and location of the lesion.13
Surgical Technique
- The patient is placed in the supine position.
- Examine the knee under anesthesia. Evaluate range of motion and ligamentous stability. Document the presence of an effusion and patellar mobility.
- Place a nonsterile tourniquet on the patient’s upper thigh.
- If the procedure is performed with a lateral post, place the post midway on the patient’s thigh. If the procedure is performed with a leg holder, put the tourniquet in the device. The patient will have to be moved distally so that the knees are near the break in the table. Drop the leg so that both extremities are hanging over the edge of the table. Place the contralateral leg in a well-padded leg holder or put pillows beneath the thigh to prevent hip hyperextension. Reflex the table to help take tension off the femoral nerve and to reduce lumbar lordosis.
- Prepare and drape the extremity in the usual sterile fashion.
- Create an inferolateral and inferomedial portal. Begin the procedure with the arthroscope in the inferolateral portal.
- Perform a diagnostic arthroscopy, evaluating all knee compartments. This includes the suprapatellar pouch, the medial and lateral gutters, the medial and lateral joints, the patellofemoral articulation, the femoral notch, and the posteromedial and posterolateral compartments. Document all pertinent findings.
- Use a probe to evaluate meniscal and articular cartilage stability.
- Debride when necessary utilizing a 4.5 mm shaver. Meniscal tears may be trimmed with arthroscopic scissors and biters. A bur may be necessary to take down osteophytes that interfere with knee motion.
- Keep operative time to a minimum. Spend the majority of the procedure addressing the symptomatic compartment.
- Suture the portals with 3–0 nylon. Dress the incisions with sterile 4 4s, soft cast padding, and an elastic wrap.
Tips and Tricks
- Make an effort to regulate inflow and outflow through the two inferior portals. A superomedial or superolateral portal may be created for inflow or outflow purposes. However, the risk with this portal may be quadriceps shutdown due to quadriceps trauma. This may delay the postoperative recovery time.
- Concerning the articular surfaces, unstable flaps can be debrided with the mechanical shaver. A smooth transition from abnormal to normal cartilage is the goal (Fig. 5–2).
- Meniscal tears are also addressed with instrumentation, leaving as much stable tissue as possible (Fig. 5–3). Only the periphery of degenerative meniscal tears must be debrided. Make sure there are no unstable flaps displaced beneath the meniscus or adjacent to the joint line.
- Avoid use of the tourniquet during the procedure. This device may be a potential source of postoperative pain. Visualization is maximized by avoiding fat-pat debridement, keeping the systolic blood pressure low, and placing epinephrine in the arthroscopic fluid.
- Postsurgical pain is minimized through preemptive anesthesia by injecting the joint with Marcaine (Abbott Pharmaceuticals, Chicago, IL) 20 minutes before the surgery and injecting the joint and portals with Marcaine at the conclusion of the case.
- Anvil osteophytes are those that arise from the central tibial surface. They may serve as a mechanical block inhibiting full knee extension. Judicious use of a bur on these structures will allow more complete knee extension (Fig. 5–4).
- Alternate use of both inferior portals with the arthroscope and shaving devices as needed. This will allow better visualization and access.
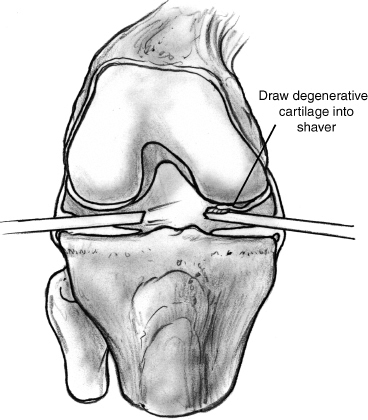
Figure 5-2 Unstable flaps can be debrided with the mechanical shaver. Using intermittent suction, draw the degenerative cartilage into the shaver. A smooth transition from abnormal to normal cartilage is the goal.
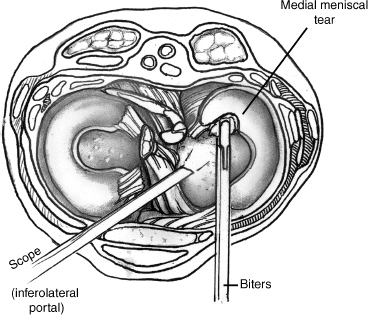
Figure 5-3 Meniscal tears are addressed with arthroscopic biters, removing only the peripheral rim of the degenerative meniscus. The majority of the meniscal body is left intact.
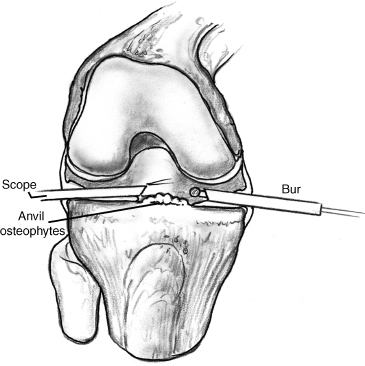
Figure 5-4 Anvil osteophytes are those that arise from the central tibial surface. They may serve as a mechanical block inhibiting full knee extension. Judicious use of a bur on these structures will allow more complete knee extension.
Pitfalls and How to Avoid Them
- Avoid the routine use of curettes and microfracture awls on arthritic chondral and subchondral surfaces. These devices are better suited for marrow-stimulating procedures, which require a postoperative course of non-weight bearing and passive range of motion. Remember, the goal of arthroscopic debridement is to remove mechanical irritants.
- Beware of the temptation to remove a relatively well-fixed chondral flap. Aggressive debridement may uncover otherwise protected subchondral bone and damage normal cartilage (Fig. 5–5).
- Limit the debridement to the symptomatic compartment. Overzealous work performed on the unaffected joint space may lead to new postoperative complaints.

Figure 5-5 Avoid undermining a relatively well—fixed chondral flap with instrumentation. Aggressive debridement may uncover otherwise protected subchondral bone and damage normal cartilage.
Conclusion
The use of arthroscopic debridement in degenerative knee arthritis may potentially decrease mechanical symptoms experienced by the patient. The procedure is palliative rather than curative, and this must be communicated to the patient before the surgery. Technically, this operation is relatively straightforward and may be performed by the experienced arthroscopist. Restraint must be employed by the surgeon to avoid aggressive debridement of chondral lesions and degenerative meniscal tears, which may lead to additional postoperative discomfort.
References
1 Merchan EC, Galindo E. Arthroscope-guided surgery versus nonoperative treatment for limited degenerative osteoarthritis of the femorotibial joint in patients over 50 years of age: a prospective comparative study. Arthroscopy 1993;9:663–667
2 Wouters E, Bassett FH, III, Hardaker WT, Jr, Garrett WE, Jr . An algorithm for arthroscopy in the over 50 age group. Am J Sports Med 1992;20:141–145
3 Yang SS, Nisonson B. Arthroscopic surgery of the knee in the geriatric patient. Clin Orthop Relat Res 1995;316:50–58
4 Baumgaertner MR, Cannon WD, Jr, Vittori JM, Schmidt ES, Maurer RC. Arthroscopic debridement of the arthritic knee. Clin Orthop Relat Res 1990;253:197–202
5 Sprague NF, 3rd. Arthroscopic debridement for degenerative knee joint disease. Clin Orthop Relat Res 1981;160:118–123
6 Buckwalter JA. Arthroscopic treatment of osteoarthritic knee joints. In: Brandt KD ed. Cartilage Changes in Osteoarthritis. Indianapolis, IN: University of Indiana Press; 1990:137–141
7 Buckwalter JA, Mow VC. Cartilage repair in osteoarthritis. In: Moskowitz RW, Howell DS, Goldberg VM, Mankin HJ, eds. Osteoarthritis: Diagnosis and Management, 2nd ed. Philadelphia: WB Saunders; 1992:71–107
8 Cole BJ, Harner CD. Degenerative arthritis of the knee in active patients: evaluation and management. J Am Acad Orthop Surg 1999;7:389–402
9 De Camara CC, Dowless GV. Glucosamine sulfate for osteoarthritis. Ann Pharmacother 1998;32:580–587
10 Barclay TS, Tsourounis C, McGart GM. Glucosamine. Ann Pharmacother 1998;32:574–579
11 Tomford WW. Chondroprotective agents in the treatment of articular cartilage degeneration. Oper Tech Sports Med 2000;8:120–121
12 Lu Y, Edwards RB, Kalscheur VL, et al. Effect of bipolar radiofrequency energy on human articular cartilage: comparison of confocal laser microscopy and light microscopy. Arthroscopy 2001;17:117–123
13 Cole BJ, Cohen B. Chondral injuries of the knee: a contemporary view of cartilage restoration. Orthopedics (Special Edition) 2000;6:71–76
< div class='tao-gold-member'>









