Arthroscopic Cuff Repair: Single-Row Options
Matthew R. Lavery
Joseph P. Burns
Stephen J. Snyder
The origins of rotator cuff surgery date back to Codman’s 1911 description of the first supraspinatus repair to its insertion on the greater tuberosity and the subsequent publication of his treatise on the shoulder in 1934. The succeeding decades produced refinement in the description of anatomy, terminology, and surgical treatment of rotator cuff tears. Neer provided us with a definition of “impingement” in 1972 and elucidated many of the important concepts in the etiology and treatment of rotator cuff disease followed today. The development of arthroscopy in the 1970s may have paved the way for modern shoulder surgery, but the past decade has provided even more rapid advancement in the techniques and implants available to surgeons treating rotator cuff disease.
Arthroscopic rotator cuff repair techniques offer significant advantages to both the surgeon and the patient. Some of these advantages include better visualization of the pathoanatomy, deltoid preservation, greater versatility in treatment, and less postoperative pain and scarring. As an increasing number of surgeons develop the skills necessary to perform these operations, we have amassed sufficient experience to document the success of arthroscopic rotator cuff repair.
In recent years, the sports medicine and arthroscopy literature has demonstrated the short- and long-term success of these techniques. Morse et al. published a metaanalysis in 2008 in the American Journal of Sports Medicine comparing outcomes between all-arthroscopic and miniopen repairs. The study found no difference in outcomes between the two techniques (1). Successful outcomes and a satisfied patient population validate the incorporation of arthroscopic rotator cuff repair into the armamentarium of any surgeon with the appropriate skill set.
Today, there is little debate over the safety and efficacy of arthroscopic cuff repair techniques although controversy remains regarding the appropriate method of fixation. Both single-row and double-row options are being extensively studied. We advocate a single-row, minimally tensioned repair that emphasizes the need for biologic healing in conjunction with an adherence to the biomechanical principles of adequate tendon to bone fixation.
CLINICAL EVALUATION
Pertinent History
The clinical history of patients with rotator cuff disease can be stratified based upon patient age. Young patients with rotator cuff problems are usually involved in aggressive overhead athletics, sustain a high-impact injury, or engage in heavy overhead manual labor. Pain typically occurs during the overhead phase of the activity and seems to diminish with rest. When pain persists after the offending activity ceases or intensifies at night, a partial thickness cuff tear should be suspected.
As patients progress toward middle age, their history often reveals a pattern of chronic overuse, especially when they routinely perform overhead work. Full-thickness cuff tears may be present, particularly in cases with shoulder trauma. Patients will report a chronically aching shoulder with radiating pain into the lateral deltoid area. This pain may be associated with weakness or catching. Often the patient has recently increased upper extremity activity secondary to a new exercise routine or job. Other patients may report more chronic impingement syndrome-type symptoms in which the rotator cuff and biceps tendon are insidiously eroded by a subacromial spur. Symptoms are often more pronounced at night and may result in the patient sleeping in a semi-sitting position or using sleeping medications to achieve some degree of rest. In severe cases, active shoulder elevation and external rotation may be weak or nearly impossible to perform.
As patients age beyond 65 years, rotator cuff pathology is extremely common, possibly affecting more than 40% of the population (2). Symptoms may be less pronounced in this age group as activity levels decline, and the chronic nature of the disease results in more compensatory movements. Weakness and chronic aching are the most pronounced complaints in this age group.
Physical Examination
Patients undergoing surgery should undergo a comprehensive physical examination. However, the evaluation of rotator cuff pathology should involve a specific and standardized
subset of tests. It is useful to inspect both shoulders for symmetry of the bony and muscular anatomy. Scars, incisions from previous surgery, and visible irregularities may give clues regarding previous trauma or treatments.
subset of tests. It is useful to inspect both shoulders for symmetry of the bony and muscular anatomy. Scars, incisions from previous surgery, and visible irregularities may give clues regarding previous trauma or treatments.
Palpation and Range of Motion
After a general inspection, assess the patient’s active and passive range of motion. Observe the patient for signs of pain during this portion of the exam. A painful arc in which the patient displays pain between 60° and 140° of flexion is a classic finding. This often indicates that the rotator cuff has been disrupted and is being pinched between the anterior edge of the greater tuberosity and the acromion. Palpate the entire shoulder including the sternoclavicular joint. Assess ligamentous integrity when there is any suspicion of instability (e.g., younger patient).
Neuromuscular Testing
Strength and function of the intrinsic and extrinsic shoulder muscles should be assessed and graded from zero to five. Resisted internal and external rotation with the arm adducted to the side allows for grading of subscapularis and infraspinatus strength, respectively. To test supraspinatus strength, the arm should be positioned in 60° of abduction and 45° of forward flexion with the shoulder in internal rotation and the thumb pointing toward the ground as resistance is applied. This maneuver is often quite painful in patients with rotator cuff pathology and should be performed with care.
Because there are several neurologically mediated conditions that can mimic the pain of rotator cuff disease, careful neurologic testing should be performed. Two of the more common conditions affecting shoulder pain and function are cervical radiculitis and suprascapular nerve dysfunction. These conditions may result in profound atrophy of the rotator cuff musculature. Patients with suprascapular nerve dysfunction often report pain that is deep in the joint and has a more constant presence as opposed to the activity-related pain of cuff pathology. Cervical nerve root pathology may produce pain that radiates down the arm and is associated with burning or numbness; deep tendon reflexes may be altered. The performance of a Spurling’s maneuver (extension, rotation, and axial compression of the neck) may reproduce these symptoms in patients with cervical nerve root irritation. An electromyogram may help more clearly define the location of a neurologic lesion.
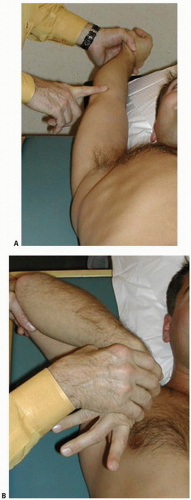
Impingement Tests
Impingement signs are often positive in patients with rotator cuff pathology. While no impingement test is completely reliable, they are a valuable component of the routine shoulder examination. We utilize the Neer test (impingement test 1) and the Hawkins test (impingement test 2) (Fig. 9.1A, B). These maneuvers are performed with the patient in the supine position to stabilize the scapula against the exam table. To perform the Neer test (impingement test 1), position the internally rotated arm into a forward-flexed overhead position. This causes the greater tuberosity to compress under the anterior acromion and
against any spur that may be present. The Hawkins test (impingement test 2) requires that the elbow be position in flexion and the shoulder in 90° of abduction. The arm is then maneuvered into an arc of adduction, elevation, and internal rotation. This maneuver results in a similar compression of the rotator cuff structures beneath the lateral and anterior acromial arch, resulting in pain when pathology is present. In addition to rotator cuff injury, biceps disease, labral pathology, and bursal inflammation may also result in positive impingement signs (3).
against any spur that may be present. The Hawkins test (impingement test 2) requires that the elbow be position in flexion and the shoulder in 90° of abduction. The arm is then maneuvered into an arc of adduction, elevation, and internal rotation. This maneuver results in a similar compression of the rotator cuff structures beneath the lateral and anterior acromial arch, resulting in pain when pathology is present. In addition to rotator cuff injury, biceps disease, labral pathology, and bursal inflammation may also result in positive impingement signs (3).
Imaging
Radiography
Four radiographic shoulder views: a true anterior-posterior (AP perpendicular to the plane of the scapula), an axillary lateral, a lateral supraspinatus outlet view, and a Zanca (acromioclavicular joint) view are obtained on patients presenting with shoulder complaints. Taken together, these four radiographs generally provide adequate information for preoperative planning in conjunction with a good quality MRI scan.
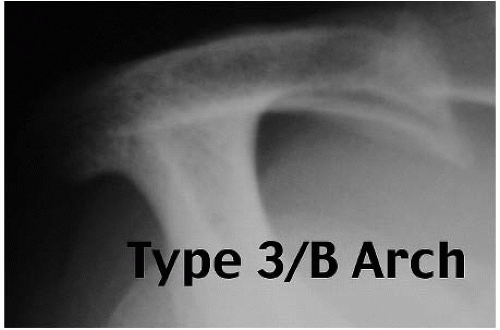
Part of that preoperative plan involves assessing the need for subacromial decompression. The supraspinatus outlet view aids in this determination as do the intraoperative findings. Based upon the supraspinatus outlet view, we apply the Bigliani and Morrison classification to the acromion: type I, flat acromion; type II, gently curved acromion; type III, acromion with a sharp inferior “beak” (4). Because acromial thickness can vary significantly, we also classify the thickness of the acromion: type A, less than 8 mm; type B, 8 to 12 mm; type C, greater than 12 mm (5). This measurement is made on the supraspinatus outlet view in an area that corresponds to the posterior aspect of the AC joint for consistency (Fig. 9.2). This information is extremely useful in the preoperative planning of a subacromial decompression.
Magnetic Resonance Imaging
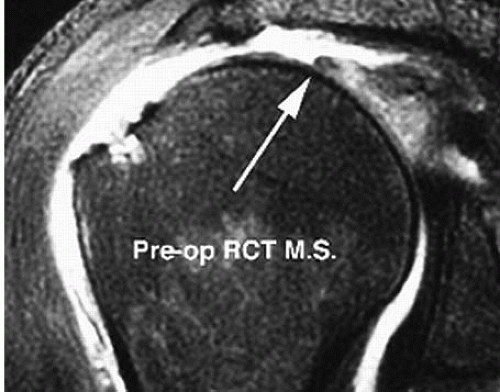
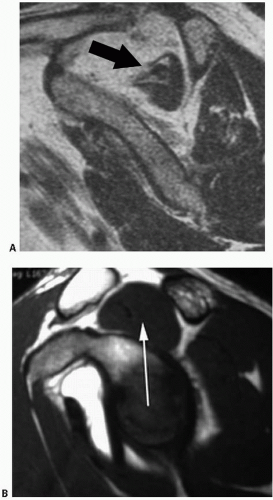
Most of our patients have obtained an MRI scan prior to rotator cuff repair. A high-quality, noncontrast MRI scan provides a multitude of information regarding the status of the rotator cuff tendons and their muscle bellies, the subscapularis, the biceps, as well as the AC and glenohumeral joints. Our protocol is to obtain sagittal oblique (perpendicular to the scapula), coronal oblique (parallel to the scapula) (Fig. 9.3), and axial sequences. The coronal images provide the most immediate assessment of the supraspinatus tendon. The most lateral cuts in the sagittal sequence can provide information regarding the amount of footprint involved in a tear, whereas the medial cuts help to assess fatty infiltration in the muscle bellies of the rotator cuff. Significant fatty infiltration of the muscle may portend a poorer prognosis following repair, and patients should be counseled accordingly preoperatively (Fig. 9.4A, B). Axial images provide a clear look at the subscapularis and posterior rotator cuff tendons. In cases where a recurrent tear or a PASTA (partial articular supraspinatus tendon avulsion) lesion is suspected, we utilize a gadolinium arthrogram in conjunction with the MRI to more clearly define the pathoanatomy.
Decision Making
Indications for arthroscopic rotator cuff repair hinge on both the patient and the surgeon. The nature of the tear (i.e., chronicity, size, and quality of the cuff musculature) has an impact on its suitability for repair. Other patient factors include age and the physical demands placed on the shoulder. Full-thickness tears do not heal or reattach to the bone without intervention and are likely to progress in size (6). Essentially all young, active patients should be considered for early repair of a torn rotator cuff tendon. In middle-aged and older patients, pain, loss of strength, and range of motion are also generally indications for operative repair, assuming a repairable tendon and adequate bone stock for secure anchor purchase.
Contraindications to rotator cuff repair are relatively few. Inadequate bone stock or large subchondral cysts may prevent adequate bone purchase and holding strength of the suture anchor. Other contraindications include advanced degenerative joint disease, overriding medical comorbidities, or activity demands low enough to tolerate
cuff deficiency. Patients with large, retracted, chronic, or recurrent tears and significant fatty infiltration should be counseled that outcomes are less predictable than with more standard tears. A capsular release and manipulation are performed at the time of repair for patients with concomitant adhesive capsulitis. We counsel the patient that they are likely to have a protracted postoperative course requiring more physical therapy to restore motion and possibly another manipulation or release to regain motion. Delaying the operation risks more atrophy and a more difficult repair.
cuff deficiency. Patients with large, retracted, chronic, or recurrent tears and significant fatty infiltration should be counseled that outcomes are less predictable than with more standard tears. A capsular release and manipulation are performed at the time of repair for patients with concomitant adhesive capsulitis. We counsel the patient that they are likely to have a protracted postoperative course requiring more physical therapy to restore motion and possibly another manipulation or release to regain motion. Delaying the operation risks more atrophy and a more difficult repair.
Classification
The ability to precisely evaluate and classify rotator cuff pathology facilitates recording, studying, and communicating treatment strategies with others. This should be done routinely as a component of the permanent operative record. The Southern California Orthopedic Institute (SCOI) rotator cuff classification system is a simple descriptive scheme that uses letters and numbers to designate the pathologic conditions of the tendon. The capital letter indicates the side of the cuff where the tear is located: “A” for articular side partial tears, “B” for bursal side partial tears, and “C” for complete thickness or transtendon damage. The degree of tendon damage is classified using a numeric designation of 0 to 5 (Table 9.1).
When recording the information, all three areas are represented even if they are normal. As an example, a tear designated A2/B4/C0 would indicate a small area of fraying on the articular surface with minimal cuff fiber damage. The bursal surface would have a significant injury with tendon fragmentation and a flap formation. Despite the severe nature of the damage, there is still no full-thickness component, hence C0. Larger, full-thickness tears can be further described by their morphology, such as crescent, U-shaped, L-shaped, reverse L-shaped, and massive degenerative tear patterns.
TREATMENT
Nonoperative Versus Operative Treatment
As previously alluded to, we recommend repairing rotator cuff tears in the majority of patients. Individuals with significant medical comorbidities, those with massive tears that may require grafting, or those who are reluctant or unwilling to undergo an operation should be counseled regarding nonoperative options for treatment of their pain. In addition, scapular strengthening exercises and biofeedback training can be employed to allow compensatory shoulder musculature to function more effectively. Patients should be appropriately counseled that although this will not cause a torn tendon to heal back to bone, it may reduce their painful symptoms.
Timing
The quality of the rotator cuff tendon tissue and amount of retraction are important factors in the decision- making process and in appropriately timing surgery. Because chronic tears have the propensity to increase in size and degree of fatty muscle infiltration, we generally recommend earlier repair in suitable candidates. When neglected for an extended period, reparable rotator cuff tears having a good prognosis can become irreparable with a poor prognosis. Our experience has shown that a fullthickness tear that includes two or three cuff tendons and is retracted medial to the level of the glenoid, especially when coupled with significant muscle atrophy, is often untreatable by direct surgical repair. However, a partial rotator cuff repair may be helpful in some of these patients if they qualify for surgery. Additionally, several methods of biologic augmentation have shown promise in bridging previously irreparable gaps (7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree