Arthroscopic Anatomy of The Knee
Jason Koh
The arthroscopic anatomy of the knee can be best described by consideration of the various parts of the knee joint that can be evaluated during a diagnostic evaluation. Familiarity with the normal anatomy and anatomical variance is important for the understanding of pathology. A complete and systematic evaluation of the knee should be performed prior to the initiation of any planned arthroscopic procedure. The precise sequence of the arthroscopic evaluation should be performed in a consistent fashion to truly assess the knee joint. We will describe the arthroscopic anatomy with regard to a standard arthroscopic evaluation (Table 54.1).
DIAGNOSTIC ARTHROSCOPY
Diagnostic arthroscopy of the knee joint typically begins with the arthroscope placed through an anterolateral portal into the knee joint. Portal creation is noted in the previous chapter; this needs to be precise and accurate both for the viewing portal and for the instrumentation portal. It is strongly recommended that the portals be created after using a spinal needle initially as a guide to the orientation of the proposed portal and instruments. If the tip of the spinal needle is able to touch the specific anatomical area of interest, this increases the likelihood that instruments will also reach those specific areas.
Table 54.1 Arthroscopic regions of the knee | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
The scope is placed through the anterolateral portal, typically entering into the suprapatellar pouch. This should be done with care to avoid iatrogenic damage to the surrounding articular cartilage. Motions inside the joint should be done gently with regard to the tip of the scope and scope sheath.
The arthroscopic evaluation of the knee should be systematic and complete. The sequence described here is not prescriptive; rather it is meant to serve as a guide to the author’s preferred technique. The precise sequence used is up to the individual surgeon; however, we recommend a thorough evaluation of all compartments.
SUPRAPATELLAR POUCH
The suprapatellar pouch is the initial location of the arthroscope. This is a normal anatomical opening above the patella separating the extensor mechanism from the anterior femur. A suprapatellar plica is a normal finding in the majority of knees (Fig. 54.1). In some cases this suprapatellar plica may be extensive enough to nearly wall off the superior portion of the suprapatellar pouch. It is important in these cases to advance the arthroscope sufficiently to view the most proximal portion of the
suprapatellar pouch; otherwise loose bodies in this area may not be identified. The suprapatellar pouch should also be evaluated for the presence of loose bodies, synovitis, or scarring. Postsurgical or posttraumatic adhesions between the extensor mechanism and the anterior femur can decrease quadriceps mobility. The anterior femur is typically covered with a richly vascularized synovial lining and fat. Nodular or villous synovitis may also be present in this area.
suprapatellar pouch; otherwise loose bodies in this area may not be identified. The suprapatellar pouch should also be evaluated for the presence of loose bodies, synovitis, or scarring. Postsurgical or posttraumatic adhesions between the extensor mechanism and the anterior femur can decrease quadriceps mobility. The anterior femur is typically covered with a richly vascularized synovial lining and fat. Nodular or villous synovitis may also be present in this area.
MEDIAL GUTTER
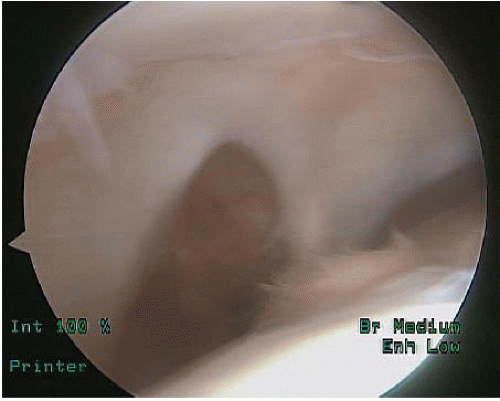
The scope is then gently brought across the knee joint into the medial portion of the knee. As the scope gently sweeps across the anterior portion of the distal femur, depending on the position of the anterolateral portal and other anatomical factors such as osteophytes, it may be difficult to sweep the scope directly anteriorly without engaging the articular cartilage of the trochlea. In this situation it is recommended that the scope be gently drawn back and passed across the more distal anterior portion of the femur anterior to the border of the trochlea. Visualization can be directed anteromedially with a scope and this may demonstrate the presence of anteromedial plica (Fig. 54.2). This plica is a normal anatomical variant in many patients and is often asymptomatic. The plica itself is a normal remnant of embryonic development. About 40% of knees have medial plica originating from the medial retinaculum and inserting onto the fat pad. In some cases an anteromedial plica may become a source of pathology for the knee joint. These pathologic plica typically have significant thickening of the tissue or synovitis and may be associated with articular cartilage damage (1, 2), If a large anteromedial plica is present, it may be difficult to visualize the medial gutter directly. The knee may need to be slightly flexed or the scope placed slightly more proximally to avoid the plica. Visualization of the medial gutter should typically be performed to assess for the presence or absence of loose bodies, marginal osteophytes, and synovitis.
PATELLOFEMORAL ARTICULATION
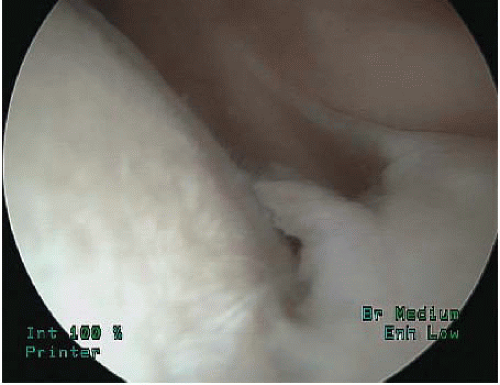
One often takes an initial look at the distal lateral facet of the patella while inspecting the patellofemoral joint. The scope can be placed to look more proximally to inspect the more proximal portion of the patella. The more medial facet of the patella is sometimes obscured by the apex of the patella. This can sometimes be further visualized by placing the scope somewhat more distally and rotating the lens so that it looks more proximally and superiorly to visualize the medial facet (Fig. 54.3). The trochlea should also be inspected. Typically, the most proximal portion of the trochlea is seen with the knee in full extension. Visualization of the trochlea is enhanced by rotating the lens inferiorly and gently flexing the knee to expose the entire trochlea (Fig. 54.4).
Patella tracking and mobility can be assessed while placing the knee through a range of motion and also by shifting the patella medially and laterally. In some cases
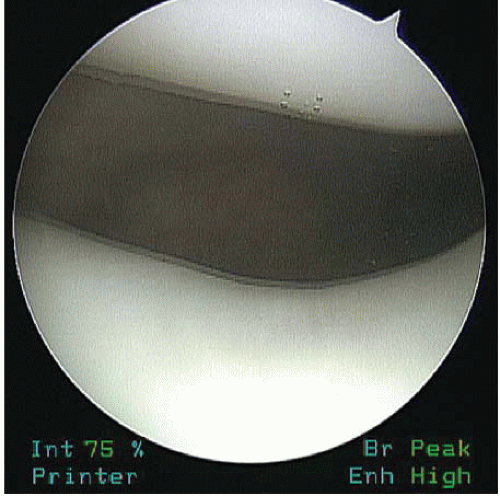
increased patella mobility can be identified with a decrease in the amount of fluid pressure within the knee because the distended knee joint has less patella mobility than the nondistended joint. The patella should be inspected for articular cartilage damage and overhanging osteophytes. In cases of patella instability there is often evidence of trauma to the medial retinaculum. The trochlea should be inspected for evidence of trochlea dysplasia and carefully inspected for the presence or absence of articular cartilage damage. In many cases there may be minimal damage seen more proximally; however, as the knee is flexed, central trochlear damage may become more evident (Fig. 54.5). Articular cartilage lesions should be evaluated for size and depth and should be graded using a standardized grading scale such as the modified Outerbridge classification (3) or International Cartilage Research Society classification (4). It is helpful to use a probe to assess the mechanical properties of the articular cartilage resistance to compression. A calibrated probe can also be used to help provide a ruler for a comparison for measurement of size and also assess the stability of any articular cartilage damage.
increased patella mobility can be identified with a decrease in the amount of fluid pressure within the knee because the distended knee joint has less patella mobility than the nondistended joint. The patella should be inspected for articular cartilage damage and overhanging osteophytes. In cases of patella instability there is often evidence of trauma to the medial retinaculum. The trochlea should be inspected for evidence of trochlea dysplasia and carefully inspected for the presence or absence of articular cartilage damage. In many cases there may be minimal damage seen more proximally; however, as the knee is flexed, central trochlear damage may become more evident (Fig. 54.5). Articular cartilage lesions should be evaluated for size and depth and should be graded using a standardized grading scale such as the modified Outerbridge classification (3) or International Cartilage Research Society classification (4). It is helpful to use a probe to assess the mechanical properties of the articular cartilage resistance to compression. A calibrated probe can also be used to help provide a ruler for a comparison for measurement of size and also assess the stability of any articular cartilage damage.
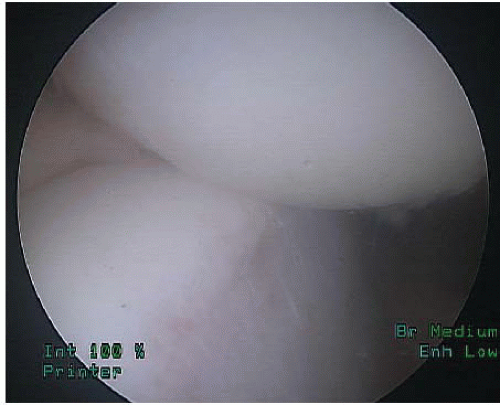 FIGURE 54.6. Identification of patella tracking by scope placed superiorly through a suprapatellar portal entering the trochlea in flexion and exiting going from flexion to extension. |
Table 54.2 Modified outerbridge classification with Insall modification (5) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Evaluation can also be performed by placing the scope superiorly using a suprapatellar portal. The patella tracking through a range of motion can be identified as the scope enters the trochlea in flexion and exits, going from flexion to extension (Fig. 54.6). This may also be enhanced by use of a 70° scope to evaluate the patella tracking (Table 54.2).
LATERAL GUTTER
The lateral gutter should be visualized, and again a similar inspection to the medial gutter should be performed looking for synovitis, loose bodies, and marginal osteophytes. The popliteal hiatus should be identified in this area (Fig. 54.7) and a gentle milking maneuver should be performed to assess for the presence of loose bodies that may move back and forth within the popliteal hiatus. If it is difficult to enter into the lateral gutter, it is recommended that the scope be slightly withdrawn from the joint and passed distal to the distal articular cartilage of the femur. Use of gentle suction applied to the arthroscopic sheath of the scope can help vacuum loose bodies from the popliteal hiatus. A portion of the posterior horn of the lateral meniscus can also be identified in this area.
MEDIAL COMPARTMENT
Inspection of the medial compartment is performed with the knee slightly flexed to allow the scope to enter the compartment over the anterior horn of the medial meniscus. The knee should be placed in flexion of approximately 20° to 30° and the valgus force applied to open up the medial compartment. Typically, this is performed with use of a post or leg holder proximally to stabilize the femur. The anatomic structures evaluated in the medial compartment are the medial tibial plateau, the medial femur, and the medial meniscus. The meniscus can be initially visualized anteriorly with the scope, and then the lens of the arthroscope can be rotated so that the viewing angle is directed more posteriorly and underneath the articular cartilage of the distal femur. The meniscus should demonstrate a smooth and consistent appearance (Fig. 54.8), and it should be possible to visualize the posterior horn of the meniscus. Incomplete visualization suggests abnormal morphology or difficulties with portal placement or positioning. If necessary, the scope should be repositioned to evaluate the entire posterior horn of the medial meniscus. A diminutive posterior horn may actually be the result of a displaced fragment entrapped behind the posterior femoral condyle. The medial joint space typically opens up 3.5 to 4 mm to allow good visualization of the posterior horn of the medial meniscus. Further improvement of visualization of the posterior horn of the medial meniscus can sometimes be enhanced by gentle external rotation of the foot while the knee is flexed in the valgus position.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree