Chapter 9 Arthropathies, Osteonecrosis, and Bursitis
Arthropathies
Osteoarthritis
Osteoarthritis (OA) is the most common type of arthritis, affecting an estimated 21 million Americans.55,71 It is suggested that 10% to 13% of Americans over the age of 60 to 65 years have OA of the knee, and the expected prevalence of OA is expected to increase as the population ages and obesity continues to rise.31,34,55 Despite the prevalence and extensive investigation of OA, the exact pathologic processes underlying OA remain somewhat elusive.
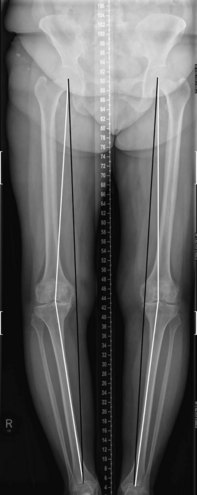
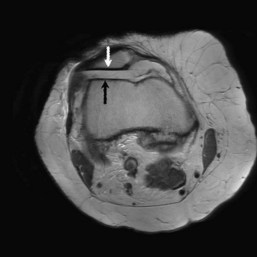
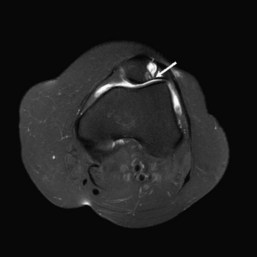
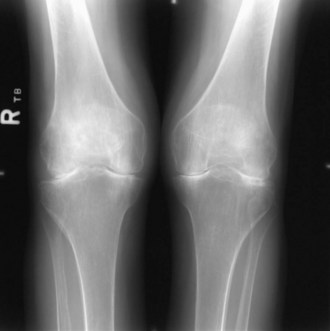
OA is now considered a disease of the entire joint and is no longer believed to be due to a “wear and tear” phenomenon alone.121 It is widely believed that the combination of local mechanical factors, including prior trauma and surgery, and systemic susceptibility is linked to its development.21,55,121 Systemic vulnerability includes such factors as genetics, age, ethnicity, nutritional/metabolic status, and female gender.34 The chief biomechanical factor influencing development of knee joint OA involves the hip-knee-ankle alignment.8,55 The knee is a complex joint that generates forces on the articular surfaces during weight bearing. The three knee joint compartments (medial, lateral tibiofemoral, and patellofemoral) may all be involved in OA. Generally, a varus or valgus angulation ≥10 degrees leads to disproportionate medial or lateral transmission of load to the tibiofemoral joint, respectively.55,57 Mechanical axis deviation is associated with medial unicompartmental arthritis more frequently than lateral compartment OA (75% involves the medial compartment, and the remaining 25% the lateral compartment).55 Predominant medial joint involvement is likely a result of increased load and stress placed upon this compartment.57 Full leg length standing views of the knees can be obtained to evaluate the mechanical and weight-bearing axes of each leg, as well as the degree of varus or valgus angulation (Fig. 9-1). The patellofemoral (PF) joint is commonly affected in knee OA, predominantly at the lateral facet. Lateral facet involvement is likely related to the large articular surface and the generation of lateral forces as a result of valgus stress.104 Anatomic abnormalities, including lateral tilt of the patella, lateral shift, patellar tracking abnormalities, and increased Q angle, can contribute to the development of OA (Fig. 9-2).46,54 Additionally, high forces transmitted through a small contact area during increasing knee flexion contribute to the development of PF OA.55 Patellofemoral OA is often associated with medial tibiofemoral compartment OA. Isolated PF OA should lead to a search for another disease process, such as calcium pyrophosphate deposition disease. Isolated and premature patellofemoral OA can be seen in patients with patellar tracking disorders.
Radiographic evaluation is an essential component in the evaluation of OA. Anteroposterior weight bearing, posteroanterior weight bearing in 40 degrees of flexion, and lateral, tangential, patellofemoral, and tunnel views may be obtained to evaluate the three compartments of the knee.57,58 A degenerative process should be considered when joint space narrowing, sclerosis, osteophyte formation, and subchondral cysts are identified, and joint involvement is not uniform (Fig. 9-3). Osteophyte formation is a common finding in OA of the knee.58,66 OA can lead to a remodeling process that results in formation of central or marginal osteophytes. Marginal osteophytes are seen at the outer borders of the articular cartilage, and central osteophytes are identified at the bone/cartilage interface. Intercondylar osteophytosis is seen in early OA and is best appreciated on the tunnel view.67 Although osteophyte formation is common and often is diagnostic for OA, findings of subchondral sclerosis or cysts (geodes) and the extent of joint space narrowing establish the severity of the disease.58 In addition, osteophyte formation helps differentiate OA from inflammatory arthropathies such as rheumatoid arthritis.7 Patellofemoral views are helpful in the evaluation of PF OA, as this joint is difficult to evaluate on lateral views. Additionally, tilt and position of the patella within the trochlear sulcus may be evaluated. CT can be performed using varying degrees of flexion (from 0 to 60) to evaluate the relative position and tilt of the patella through a full range of motion.
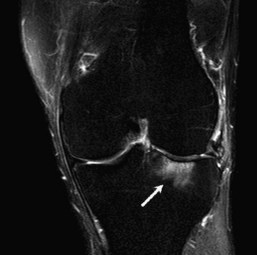
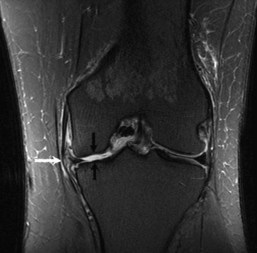
Although typical features of OA include loss of hyaline articular cartilage and osteophyte formation, it is now believed that OA includes important changes in subchondral bone, synovium, menisci, and/or ligaments.21,26 For this reason, MRI excels in the evaluation not only of the osseous changes of OA, but also of associated soft tissue pathology. Subchondral bone abnormalities include bone marrow edema–like lesions (BMLs), subchondral cysts, and attrition. On magnetic resonance imaging (MRI), BMLs are low signal subarticular foci on T1-weighted images with corresponding high signal on fat-suppressed T2-weighted or short tau inversion recovery (STIR) sequences.26 It is important to differentiate degenerative BMLs from other traumatic and nontraumatic marrow signal abnormalities. The key feature in distinguishing degenerative marrow signal abnormality is identifying subjacent articular cartilage damage (Fig. 9-4).10,26 Subchondral cysts, a common feature of OA, are defined on MRI as round, circumscribed areas of fluid intensity signal (Fig. 9-5).26,129 Subchondral attrition is often associated with advanced OA and is a good predictor of cartilage loss (Fig. 9-6).26 Both subchondral cysts and attrition are often seen in regions of BMLs. Furthermore, BMLs and subchondral attrition are associated with knee malalignment. Generally considered a secondary phenomenon, synovitis is another important component of OA.26 On MRI, enhancement and thickening of the synovial membrane on contrast-enhanced T1-weighted sequences are indicative of synovitis.26,74
MRI is regarded as the best noninvasive imaging modality for the detection of cartilage defects, although the gold standard for the diagnosis of articular cartilage lesions remains arthroscopy.29,44 Both proton density (PD) and fat-suppressed (FS) PD fast spin echo (FS PD-FSE) weighted images are commonly employed to evaluate articular cartilage, some investigators use gradient echo MRI. FS PD-FSE sequences provide increased conspicuity of lesions due to the ability to differentiate between fluid and cartilage. Associated subchondral bone abnormalities are less well imaged by non–fat-suppressed PD images when compared with fat-suppressed sequences.113 Some investigators prefer to evaluate articular cartilage with the use of gradient echo imaging or newer techniques such as T2 mapping, T1RHO, and delayed MRI of cartilage following intravenous gadolinium administration. T1 FS imaging after placement of intra-articular gadolinium may be used to provide images similar to nonarthrographic FS PD-FSE images. Many grading systems in the radiology and orthopedic surgery literature have been used to quantify cartilage abnormalities. Because these grading systems vary, it is best to describe the size of the region of abnormal signal intensity, the degree of surface fibrillation or irregularity, and the depth of cartilage involvement (partial- or full-thickness defects).46,60 Although MRI allows for ease of identification and varying extent of cartilage abnormalities, some literature has suggested no significant correlation between clinical symptoms and extent of MRI findings.72
The menisci are intimately related to the hyaline articular cartilage. By acting in shock absorption and load transmission, the menisci distribute stress over a large area of articular cartilage. Meniscal tears often predispose to knee OA because of loss of this protective function. It is interesting to note that knee OA may lead to meniscal tears, which, in turn, result in further cartilage damage (Fig. 9-7).33 Normal appearing menisci are rarely found in knees with OA. Usually, the menisci are torn and macerated when evidence of advanced OA further supports the association between meniscal pathology and OA.15,33,56 During arthroscopic surgery, the goal is to preserve as much of the meniscal tissue as possible because a large body of data supports progression to OA after partial or complete meniscectomy.33,104
Inflammatory Arthropathies of the Knee
Rheumatoid arthritis (RA) is a common and progressive inflammatory arthropathy affecting the synovium of joints in a bilateral, symmetrical distribution. The diagnosis of RA is typically made by a combination of clinical, laboratory, and radiographic findings. RA commonly affects the knee, demonstrating similar radiographic findings as are seen more classically in the hands and wrists. Although radiographic findings can be diagnostic for RA, they are often not clearly seen until later in the disease. For this reason, and for its superior soft tissue depiction, MRI has proved to be of much greater utility in evaluating these patients during the early stages of disease, when radiographic findings are often occult.37–39 Diagnosis at this early stage allows earlier intervention with disease-modifying antirheumatic drugs and subsequently more rapid cessation of symptoms.
The spectrum of radiographic findings of RA in the knee ranges from the nonspecific finding of a joint effusion early in the disease to marginal erosions and eventual uniform joint space narrowing late in the disease (Fig. 9-8). Other findings include periarticular osteopenia and soft tissue swelling. Marginal erosions, unlike central erosions seen along the weight-bearing portion of the knee articulation, occur at the edges of the joint, where synovial reflections are present without underlying cartilage. The lack of cartilage in these regions, along with the presence of inflamed synovium, results in erosive osseous change. With disease progression and continued inflammation, more global cartilage loss occurs throughout the joint space. Erosions from RA can also happen once the hyaline cartilage has been lost and subchondral bone becomes exposed. The radiographic finding of periarticular osteopenia is believed to be secondary to synovitis-induced osseous hyperemia in RA.
MRI is far superior in imaging the osseous, articular, and periarticular changes in RA when compared with radiographs.* A specific advantage is the imaging of synovitis, which is seen as synovial thickening or irregularity, as well as increased synovial signal intensity.22,116 Of particular interest is the appearance of the synovium after intravenous administration of gadolinium–diethylenetriaminepentaacetic acid (DTPA) (Fig. 9-9). Contrast-enhanced imaging allows better differentiation between synovium, effusions, and pannus.2,68 Also, measurement of gadolinium uptake over time has been correlated with the degree of synovitis in patients with RA and therefore can provide additional information as to the severity of synovial inflammation.30,96–98 Other findings seen on MRI include the presence of joint effusions, erosions, hyaline cartilage loss, and a bone marrow edema pattern that may serve as a precursor to further erosive change. Rice bodies, sloughed and hypertrophied fragments of synovium, are imaged to advantage on MRI and appear as small, low signal, loose bodies within the joint (Fig. 9-10).
While radiographs remain the primary modality of differentiating RA from other inflammatory arthropathies, in confounding cases MRI may be of value.83,84 McGonagle and associates83 demonstrated that the MRI finding of entheseal abnormalities is commonly seen in patients with spondyloarthropathy but is not encountered in patients with RA. An additional application of MRI in patients with RA is monitoring response to therapy. This has most commonly been applied to disease at the wrist.95
Juvenile idiopathic arthritis (JIA) is the most common rheumatic disorder of childhood.24 The term juvenile idiopathic arthritis has replaced juvenile rheumatoid arthritis because of the broad spectrum of disease and causality within this diagnosis. JIA includes oligoarticular and polyarticular JIA (rheumatoid factor [RF] negative and RF positive), juvenile psoriatic arthritis, systemic JIA, and enthesitis-related and undifferentiated arthropathies.18,122 It commonly affects the large joints of the body, most frequently the knee,80 and radiographic findings can be similar to those seen in RA, such as periarticular osteopenia and joint effusions. More specific to JIA are the presence of epiphyseal overgrowth and the potential for late-stage ankylosis; the latter is not characteristic of adult RA.
As with RA, MRI has been shown to be useful in the early identification of JIA and in assessing clinical response to treatment.49,86 MRI findings include the presence of joint effusions, synovial hypertrophy and pannus formation, rice bodies, erosions, bone marrow edema pattern, epiphyseal overgrowth, and cartilage degeneration (Figs. 9-11 and 9-12).* Contrast-enhanced imaging is also useful in JIA for evaluating the extent of synovial inflammation.
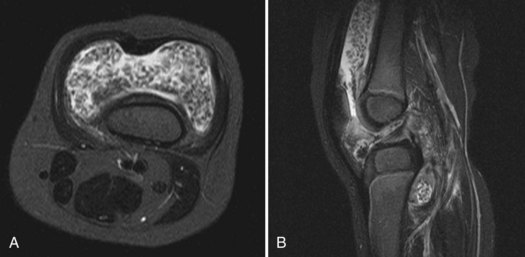
Hemophilic arthropathy, although not technically an inflammatory arthropathy, shares radiographic imaging findings with JIA, particularly at the knee. Hemophilia is an X-linked recessive congenital disorder caused by a deficiency of clotting factors and is therefore clinically seen in males but carried by females. In the knee, radiographic manifestations of hemophilic arthropathy include osteopenia, epiphyseal overgrowth, and widening of the intercondylar notch (Fig. 9-13).65 Because of the presence of repeated hemarthroses, dense effusions are seen in patients with hemophilia. MRI can show similar findings as well, including synovial hypertrophy and cartilage abnormalities.128 However, because of frequent and chronic hemarthrosis within the knee, low signal is seen within the joint space on PD-, T1-, and T2-weighted imaging from synovial hemosiderin deposition (Fig. 9-14). These signal characteristics are not seen in patients with RA and therefore, besides the obvious clinical history, serve as a definitive discriminating factor.
Crystal Deposition Diseases and Arthropathies
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease is the most common crystalline arthropathy and often affects the knee articulation.1 Its prevalence increases with age, and it has been reported that 50% of patients older than 80 years of age have CPPD.82 CPPD typically manifests itself by the presence of calcification in and around the knee joint, most commonly as chondrocalcinosis (calcific deposits within the menisci and hyaline cartilage) (Fig. 9-15). Chondrocalcinosis itself is asymptomatic and is mainly a radiographic finding that can be seen in a variety of diseases. However, some patients manifest an arthropathy with CPPD when crystals are shed into the joint and are phagocytized by leukocytes, thereby releasing chemotactic factors.79 Other clinical and radiographic presentations of CPPD arthropathy include mimics of OA, gout, and neuropathic arthropathy.
CPPD arthropathy can often have similar radiographic findings as OA with cartilage loss, subchondral cyst, and osteophyte formation. Although the menisci and hyaline cartilage most often demonstrate the presence of calcium deposition, the arthropathy, when present, has a preference for the patellofemoral joint with relative preservation of the medial and lateral compartments. Many of these patients are older, and superimposed degenerative joint disease may be present, potentially complicating the diagnosis. Definitive diagnosis can be confirmed by direct synovial fluid crystal analysis. MRI shows the aforementioned findings to greater advantage, with particular strength in imaging the presence of synovitis. Chondrocalcinosis is seen as low signal within the menisci and hyaline cartilage that often is more apparent on gradient echo imaging.13 It should be noted that the presence of calcium within the menisci does lower the sensitivity and specificity for detecting meniscal tears on MRI.63
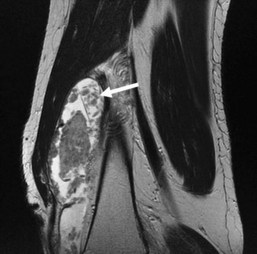
Gout is a systemic metabolic disease characterized by elevated serum urate levels, deposition of urate monohydrate crystals in and around joints, and renal disease.108 Crystal deposition within joints results in acute attacks of gouty arthritis. Chronic gout is manifested by tophi deposition around joints and typically occurs many years after initial acute symptoms. It is rare for chronic tophaceous gout to occur in a patient who has not previously had episodes of acute gouty arthritis.41,107,127 Chronic gout is significantly more common in men (20 : 1), occurs most often during the fifth to seventh decades of life, and has a predilection for the lower extremities. The most common sites include the feet and knees, as well as the hands and elbows.
Imaging is not indicated in cases of acute gout because no specific radiographic findings are known. In cases of chronic tophaceous gout, imaging is useful in that the clinical symptoms and presentation can overlap with other arthropathies, including septic arthritis. Radiographic findings of tophaceous gout involve both the bone and adjacent soft tissues (Fig. 9-16). Tophi appear as soft tissue masses that are eccentric in relation to the bone and joint space. Rarely, they can be intra-articular or intraosseous. Within the knee, tophi can also deposit within the distal quadriceps tendon, which explains the predisposition of patients with gout to tendon rupture (Fig. 9-17). Calcification within tophi is more often present in patients with concomitant renal disease.58 Juxta-articular bone erosions are common and are often seen beneath soft tissue masses or tophi.73 Overhanging edges are seen, representing new bone formation around these erosions. At MRI, tophi can have a variable appearance but are typically isointense to muscle on T1-weighted images, with mixed intermediate and low signal on T2-weighted images (Fig. 9-18).127 Postgadolinium imaging demonstrates irregular enhancement of the tophi.
Synovial Proliferative and Tumor-like Disorders
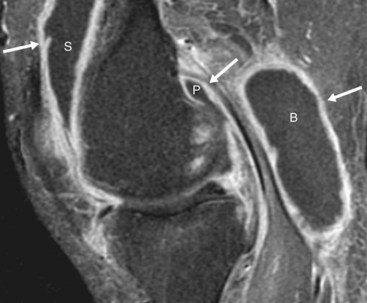
Pigmented villonodular synovitis (PVNS) is a benign synovial proliferative process that is thought to be neoplastic in origin and most commonly affects adults in their third to fifth decades. This process can be localized (75% to 85%) or diffuse (15% to 25%). The localized form can be intra-articular or extra-articular. When it occurs within a bursa, it is called pigmented villonodular bursitis (PVNB), and around the knee it is most common in an infrapatellar location.92 This has been previously termed localized nodular synovitis of the knee.53 The localized extra-articular form is found in tendon sheaths and is called giant cell tumor of the tendon sheath (GCTTS). This is uncommon in the knee and most often occurs in the hands and feet. Diffuse PVNS is a monoarticular process that is most common (66% to 80%) in the knee.92 It is important to differentiate between focal and diffuse forms of the disease, as the clinical presentations and response to treatment differ significantly. The localized form requires only local excision and rarely recurs, whereas the diffuse form requires extensive synovectomy and commonly recurs.53
The most common radiographic feature found in PVNB and the diffuse, intra-articular form of PVNS is a suprapatellar effusion, although with diffuse PVNS, periarticular erosions with preservation of the joint space are commonly found (Fig. 9-19). Erosions from diffuse intra-articular PVNS in the knee are less common than those from the same process in other joints such as the hip, because of the potential for decompression into larger joint recesses and adjacent structures. On CT, diffuse intra-articular PVNS may demonstrate periarticular erosions but usually reveals diffuse synovial thickening.
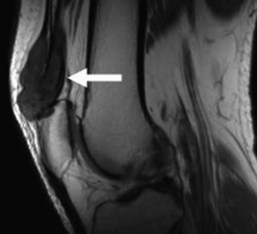
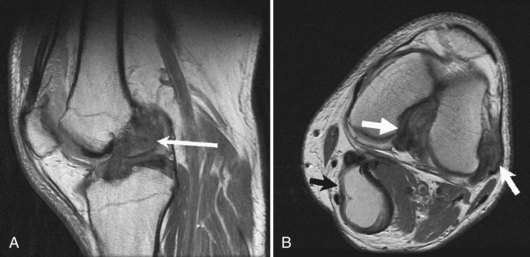
MRI is the best modality for evaluation of PVNS and PVNB. Intra-articular PVNS or PVNB appears as thick, sometimes nodular, and masslike synovial thickening, which is hypointense/isointense on T1, is hypointense on T2, and enhances on postcontrast sequences (Figs. 9-20 and 9-21). This hypointense signal on T2-weighted sequences is attributable to hemosiderin, and on gradient echo sequences, these areas enlarge through a process known as blooming. Although processes such as synovial hemangioma and hemophilic arthropathy can also demonstrate blooming, the former can be identified by the presence of internal flow voids, and the latter by clinical history.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree