Anterolateral Approach for Primary Total Hip Replacement
Michael E. Berend
Key Points
Introduction and History
The anterolateral approach to the hip for total hip replacement (THR) was described and popularized by Hardinge in 1970.1 It offers an extensile approach for both primary and revision THR. Traditionally, it involved a split in the anterior portion of the abductor musculature and hip capsule. Modifications have been made in the trajectory and extent of the abductor split over the past three decades.2,3 Exposure of the acetabulum involves retractor insertion to achieve posterior displacement of the femur. In general, advantages have traditionally been ascribed to extensibility and reduction of postoperative dislocation in primary3–6 and revision THR7; proposed disadvantages have included postoperative limp and abductor weakness.
Patient Selection
Most patients who are indicated for a total hip arthroplasty are amenable to an anterolateral surgical approach. Patients who are at higher risk for postoperative dislocation such as femoral neck fracture,8 neuromuscular disorders,9 high range of motion (ROM),10 abductor tendon tears,11 and rotational deformities may benefit from an anterolateral surgical approach.
Positioning
The patient is placed in the lateral decubitus position with the use of a padded pegboard. Attention to ensure that the pelvis is perpendicular to the table is important before skin preparation and draping. Special attention should be focused on posterior stability of the pelvis because femoral retraction to achieve acetabular exposure tends to retrovert the pelvis.
An axillary roll is inserted to help protect the brachial plexus. The leg is positioned anterior to the table during femoral preparation, and leg sterility must be ensured. This may be accomplished with multiple stockinettes or a leg bag, in which the distal extent of the leg may be placed during femoral preparation.
Surgical Anatomy
The incision for an anterolateral approach to the hip is placed over the greater trochanter. With smaller incisions, approximately two thirds of the incision should be proximal to the tip of the trochanter and one third distal. An oblique incision (proximal extent posterior and distal extent anterior) may permit a smaller incision, and skin mobility permits a mobile window during acetabular preparation through the distal extent of the incision. Similarly, the proximal extent may be mobilized during femoral preparation and implant insertion.
The tensor fascia and the gluteus maximus are split in line with their fibers centered over the greater trochanter, exposing the gluteus medius insertion. The tendinous portion of the gluteus medius is covered superiorly by muscular fibers and must be included in the final repair. The proximal portion of the vastus lateralis inserts into the vastus ridge at the inferior portion of the greater trochanter. Approximately 2 cm of the anterior one third of the vastus lateralis is split in line with its fibers and is extended superiorly over the anterior portion of the trochanter and obliquely at a 70- to 90-degree angle, spreading the fibers of the gluteus medius; this exposes the gluteus minimus and hip capsule (Fig. 18-1). Over the anterior-superior femoral neck, the gluteus minimus and capsule are split in one layer; this facilitates subsequent repair in a tenodesis fashion. A retractor can be placed into the hip joint at this point, and the femoral insertion of the anterior hip capsule and the iliofemoral or Y ligament are released off the femur with external rotation of the leg. The release is continued down to the level of the lesser trochanter and the iliopsoas insertion. The superior dissection is carried cephalad to the level of the acetabular rim. Care should be taken to not extend the abductor split more than 4 cm superior to the tip of the greater trochanter because the superior gluteal nerve may be at risk of injury.11
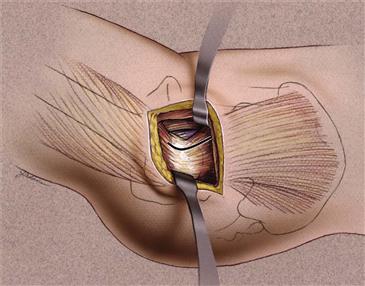
Figure 18-1 Graphical representation of the deep dissection of the abductors for an anterolateral approach to the hip shown in the operative photograph. (Used with permission from JIS, Inc. Joanne Adams.) (Krenzel BA, Berend ME, Malinzak RA, et al: High preoperative range of motion is a significant risk factor for dislocation in primary total hip arthroplasty, J Arthroplasty 25(6 Suppl):31–35, 2010; Epub 2010 Jun 11.)
The opportunity for recognition and repair of attritional abductor tears has been described with this approach.12 Often the superior-most superficial layer of the gluteal medius fibers is intact, and after they are incised, a significant tear of the insertion of the gluteal medius is noted. In these cases, a large osteophyte with a sclerotic cortex is present on the anterior portion of the trochanter. This is similar in appearance to a rotator cuff tear and the changes noted in the humeral head. This osteophyte is removed at the completion of the case to expose cancellous bone and to facilitate healing of the repaired abductor attritional tear.
The hip can be dislocated with external rotation of the leg (Fig. 18-2). A bone hook or hip skid may be a useful adjunct if soft tissue contracture or osteophytes inhibit dislocation. Alternatively, a neck cut can be made in situ, as in cases of acetabular protrusio or significant deformity. Retractors should be placed around the femoral neck and a “napkin ring” of bone removed; this allows femoral head visualization and removal with a corkscrew. Alternatively, after dislocation, retractors are placed around the superior and inferior femoral neck, while the femoral neck osteotomy is completed at the level based on preoperative templating with reference to the lesser trochanter. The femoral head is then removed.
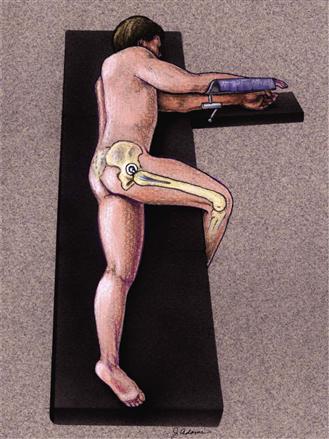
Figure 18-2 Graphic representation of leg position utilized during anterolateral approach to the hip. (Used with permission from JIS, Inc. Joanne Adams.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







