Chapter 43 Anterior Cruciate Ligament Reconstruction With Hamstring Tendons
Graft options include hamstring tendon autograft, patellar tendon autograft, and allograft. The ideal graft should be easy to harvest with minimal donor site morbidity, have the strength of the native ACL, incorporate quickly, and allow rigid fixation to enable early mobilization and rehabilitation. Most surgeons prefer autograft because of ready availability, decreased cost, and faster graft incorporation and because of the risk of disease transmission associated with the use of allograft.17,20,36 Historically, patellar tendon autograft is the gold standard; however, because of the associated complications related to donor site morbidity,88,90,95 many surgeons are now using hamstring tendon autografts.
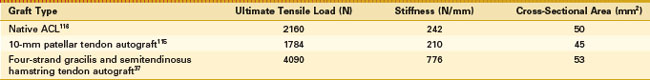
Biomechanical advantages of hamstring tendon grafts include increased strength, stiffness, and larger cross-sectional area for vascular ingrowth and ligamentization (Table 43-1).37,79,80,108
An understanding of the process of graft healing is required to manage the reconstructed ACL safely through the rehabilitation process. Over time, the graft undergoes a process of remodeling and revascularization, referred to as ligamentization.5 Most studies on graft healing have been conducted using various animal models.35,87 Few studies have examined the process of ligamentization in humans and the true process is not completely understood. Several authors have found, using core biopsy of traumatically failed hamstring autografts, that complete graft integration with the surrounding bone occurs, with the presence of Sharpey-like fibers as early as 12 weeks with interference screw fixation.78,82 Other biopsies have shown the graft to be enveloped with a layer of granulation tissue and that macroscopically and histologically, no direct connection between the tendon graft and the bone could be found. There are no neural elements in the reconstructed ACL9 and some have suggested that a normal ligament never forms after ACL reconstruction.32,68
There have been several well-conducted prospective studies and meta-analyses comparing the results of hamstring and patellar tendon autografts. The results of these studies suggest that a functionally stable knee is achieved in more than 95% of patients with hamstring tendon or patellar tendon autograft ACL reconstructions.30 The most consistent difference between the two graft options in these studies is increased kneeling and anterior knee pain* and greater loss of postoperative extension† with patellar tendon reconstructions. Over the short term, the hamstring tendon graft has been associated with tendon discomfort for up to 6 to 8 weeks after surgery, weakness with high knee flexion, and greater laxity.6,22,28 The issue of increased laxity seemed to be related to inadequate fixation, which has subsequently been resolved with alternate fixation devices. Over the long term, the patellar tendon graft may be associated with higher rates of radiographic degenerative change. In studies in which fixation, surgical technique, and rehabilitation are standardized, the incidence of ACL graft rupture is equivalent with hamstring and patellar tendon autograft.92,103 It is generally well accepted that reconstruction of the ACL with hamstring tendon autograft is effective for restoring anteroposterior laxity to the knee, has good subjective outcomes, and allows a high proportion of patients to return to their desired activity level.
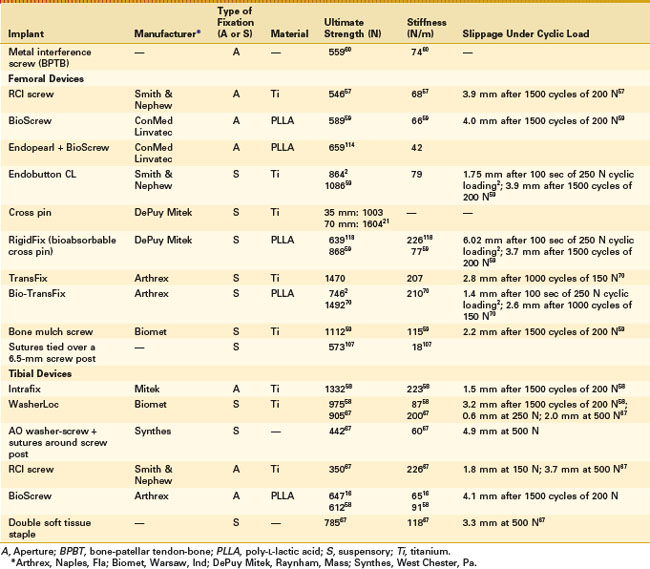
For immediate postoperative mobilization, the ACL graft-fixation construct should be strong enough to withstand the everyday forces required for walking and activities of daily living, which has been estimated to be up to 450 N.40,44,74,79 Currently, there are a multitude of fixation options for hamstring tendon autografts. These are classified into aperture versus suspensory fixation and metal versus bioabsorbable materials. There are several considerations when selecting a fixation device. First, the process of graft healing and maturation is poorly understood, as is the effect of rehabilitation protocols on these processes. Second, most studies on fixation devices and their biomechanical properties have been conducted on animal or cadaver models and in vivo results may differ. Commonly used fixation devices and their biomechanical properties are summarized in Table 43-2.
Table 43-2 Commonly Used Fixation Options in Hamstring Tendon Anterior Cruciate Ligament Reconstruction
Aperture fixation with interference screws is commonly used in ACL surgery. Soft tissue interference screws with blunt threads were designed for hamstring tendon grafts to enable compression of the graft against the tunnel wall without graft damage. Improved initial soft tissue graft fixation strength can be achieved with the use of a longer13 and larger diameter screw.113 Proper graft-tunnel fit with the tunnel sized 0.5 mm larger than the graft diameter also improves fixation strength.104 Nurmi and colleagues81 have found that there is no difference in initial fixation strength between compaction and extraction drilling using a porcine model. However, extraction drilling often leaves sharp bony edges within the tunnel that can damage the graft on insertion, and compaction drilling may still be beneficial to avoid graft damage. Concentric or eccentric screw placement does not influence initial fixation properties.97,99
Suspensory fixation has been reported to result in an increased incidence of tunnel widening compared with aperture fixation.11,43 The exact mechanism of this is unknown, but proposed reasons include a greater distance between the fixation point and tunnel aperture, leading to micromotion between the graft and bone. Clinical studies have shown, however, that there is no difference between aperture and suspensory fixation methods with respect to physical examination, instrumented testing, Lysholm, Tegner, and International Knee Documentation Committee (IKDC) scores.11,65,100
Graft fixation is also affected by bone mineral density.13,18,40 The bone mineral density of the proximal tibia is lower than that of the distal femur. Hill and associates42 have found that females undergoing ACL reconstruction with hamstring tendon autograft and 7- × 25-mm interference screw fixation may develop increased postoperative laxity compared with their male counterparts; they recommended supplemental tibial fixation with a staple, which successfully restored normal laxity at the expense of increased kneeling pain at 2-year follow-up. Older patients are another subgroup of patients with decreased bone mineral density for whom supplemental tibial fixation may need to be considered.
There has been a recent trend toward using bioabsorbable fixation devices. Possible advantages of bioabsorbable devices include easier revision surgery, minimal interference with future imaging such as magnetic resonance imaging (MRI),40,76 and decreased risk of graft laceration during insertion of bioabsorbable interference screws.14,119 Ultimately, the benefit of bioabsorbable screws is resorption of the device, with subsequent bony replacement of the device in the tunnel. Unfortunately, this has not consistently been the case in vivo. Studies have found no evidence of screw resorption up to 4 years postoperatively and no evidence of new bone formation in the tunnels.10,86,111 Other disadvantages of bioabsorbable devices include synovitis12,31 and device breakage, leading to loss of fixation, a potentially catastrophic complication.19 With current software and imaging techniques, the metal artifacts from titanium screws can largely be eliminated. If revision is required, a small, screw-shaped femoral defect is superior to a larger fibrous defect or a partly resorbed bioscrew with remnant material adhering to the tunnel wall. Thus, our preferred technique is to use metallic interference screw fixation of hamstring tendon autografts, which have had excellent clinical success for over 15 years.
When assessing the outcome of ACL reconstruction, it is imperative to acknowledge that variations in the surgical technique and selection of patients have a direct effect on outcomes. The surgical technique described in this chapter, using the anteromedial portal and a four-strand hamstring tendon autograft, has been used in an ongoing prospective study of 200 patients with an isolated ACL injury since 1994. A summary of the 7-year outcome of 200 patients and the 10-year outcome of a subgroup of 90 patients from this group is shown in Table 43-3.83,94 Ongoing longitudinal assessment is continuing, and we are currently collecting the 15-year outcomes.
Table 43-3 7- and 10-year Outcomes of Isolated Anterior Cruciate Ligament Reconstruction*
| Parameter | OUTCOME | |
|---|---|---|
| 7-year | 10-year | |
| No. of patients reviewed | 165/200 | 86/90 |
| ACL graft rupture (%) | 11 | 13 |
| Contralateral ACL rupture (%) | 6 | 10 |
| Mean KT-1000 (mm) | 1.6 | 1.6 |
| Lachman grade 0 (%) | 75 | 79 |
| Grade 0 pivot (%) | 85 | 86 |
| Normal or nearly normal IKDC range of motion grade (%) | 99 | 98 |
| Lysholm median | 95 | 89 |
| Patients able to hop >90% of contralateral limb (%) | 79 | 80 |
| No knee-related decrease in activity (%) | 89 | 89 |
| Overall IKDC grade A or B (%) | 83 | 83 |
| Grade A radiograph (%) | 83 | 81 |
* Using four-strand hamstring tendon graft, interference screw fixation, and anteromedial portal.
Corry and coworkers22 have found a left- to right-sided difference in knee laxity measurement. It was hypothesized that this difference is related to graft rotation during femoral screw insertion. With a standard screw, clockwise graft rotation occurs, leading to a posterior final graft position in left knees but a relatively anterior final graft position in right knees. This was improved with the use of a reverse thread screw for right-sided ACL reconstructions.75
Improper tunnel placement is one of the most common, yet avoidable, reasons for early graft failure.* Single-incision arthroscopic ACL reconstruction was introduced and popularized using transtibial femoral tunnel drilling.73 When constrained by the tibial tunnel, proper placement of the femoral tunnel can be more difficult to achieve reproducibly and often results in vertical graft placement, leading to residual anterolateral rotatory instability.7,41,54 Subsequent research has confirmed that lower, more anatomic, tunnel placement in the lateral femoral condyle results in increased rotational stability of the knee, with elimination of the pivot shift phenomenon.38,50,53,64
The low anteromedial portal technique was first described by the senior author (LP) and has been used since 1989. It has recently gained popularity because of recognition of the importance of femoral tunnel placement and the advent of double-bundle ACL reconstruction techniques.106,120 The principle of the low anteromedial portal technique is drilling of the femoral tunnel independent of, and before, drilling the tibial tunnel, allowing the tunnels to be placed within their respective ACL footprints.54 Another advantage of this technique is improved visualization. In the transtibial technique, once the tibial tunnel is drilled, the irrigation solution escapes through this tunnel, decreasing the intra-articular pressure and obscuring visualization required for femoral tunnel placement.
The key to successful femoral drilling via the anteromedial portal requires that the knee be flexed to 120 degrees at the time of drilling and screw insertion (see Fig. 43-5). This helps prevent posterior wall blowout.39 A low central anteromedial portal, 1 cm proximal to the medial joint line, helps prevent injury to the medial femoral condyle during femoral tunnel drilling and screw insertion105 and allows an anterior orientation to the femoral tunnel direction.
Successful results 7 years after surgery are strongly associated with the radiologic position of the tunnels. The center of the femoral tunnel should be located 86% posteriorly along Blumensaat’s line and, on the AP view, it should be at a distance of 43% lateral to the lateral femoral epicondyle. Anterior placement of the femoral tunnel is associated with adverse clinical outcomes as a result of excessive constraint, leading to loss of movement or elongation of the graft with cyclic loading. The tibial tunnel should be centered 48% posteriorly along the tibial plateau on the lateral radiograph. Placement of the tibial tunnel center 50% or more posteriorly is associated with loss of knee flexion and increased incidence of graft rupture. More anterior placement is associated with graft impingement and decreased range of motion. In the coronal plane, the tibial tunnel should be centered 47% across the width of the tibial plateau from the medial cortex. More lateral placement is associated with impingement of the graft, whereas medial placement will result in loss of flexion. The graft inclination angle should be measured from a 30-degree weight-bearing posteroanterior radiograph. This angle is subtended by a line connecting the medial wall of the femoral tunnel and the medial wall of the tibial tunnel and a line perpendicular to the tibial plateau84 (see Fig. 43-8).
Surgical Technique
Timing of Surgery
It is now well accepted that ACL reconstruction should not be performed until the knee has recovered from the acute injury—after the effusion has resolved and almost full pain-free range of motion has been achieved. Early intervention should only be considered in the acutely locked knee caused by a displaced bucket handle meniscal tear; however, most patients with fixed flexion deformity have a medial ligament strain preventing terminal extension, rather than a bucket handle tear of the meniscus, which is extremely rare in an acute, first-time cruciate ligament injury.51
Preoperative Considerations
The evolution of ACL reconstructive surgery, advent of day surgery, and anesthetic technique have resulted in this operation being an elective outpatient procedure. All patients receive antibiotic prophylaxis. The most common bacteria causing infection are coagulase-negative staphylococci and Staphylococcus aureus.52,110 Coagulase-negative staphylococci are often resistant to first-generation cephalosporins but are susceptible to vancomycin. Accordingly, patients receive 1 g vancomycin and 2 g of a cephalosporin IV 1 hour prior to induction of anesthesia for prophylaxis against these common bacteria. We understand that this antibiotic regimen is controversial; however, using this antibiotic regimen, our infection rate has dropped to less than 0.2%. Vancomycin resistance has never been reported using the antibiotic in this manner.
Positioning and Examination
Following induction of anesthesia, the patient is positioned supine on the operating table lying close to the edge of the table on the operative side. A tourniquet is placed high on the thigh and inflated after the limb is exsanguinated and a straight leg raise is performed to stretch the hamstrings. The knee is positioned at 70 degrees of flexion using a foot rest and a lateral thigh post (Fig. 43-1). The foot rest is placed at the end of the operating table, which allows the surgeon to stand at the foot of the table to harvest the graft, rather than leaning over the limb toward the center of the table.
Hamstring Tendon Harvest and Graft Preparation
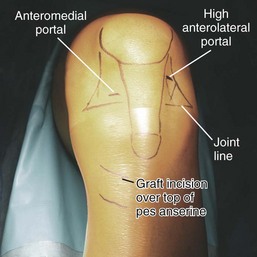
A sound knowledge of the surface anatomy around the knee is imperative for successful graft harvest. The hamstring tendons insert at the pes anserine, 1 cm medial to the tibial tubercle and 1 to 3 cm distal to the tubercle. The gracilis and semitendinosus tendons are harvested through a 2-cm oblique incision centered over the pes anserine to decrease the incidence of injury to the infrapatellar branch of the saphenous nerve (Fig. 43-2). However, until a level of surgical comfort is achieved in harvesting the tendons, a vertical incision, which is extensile, should be used. Although this places the infrapatellar branch of the saphenous nerve at greater risk, it is preferable to an insufficient graft. A vertical skin incision is also recommended for patients in whom palpation of the tendons is difficult or for whom prior trauma or surgery may have created scar tissue about the pes anserine, making a difficult harvest. If palpation of the tendons is difficult, centering the incision three fingerbreadths below the joint line approximates the correct position.
Using a right-angled forceps to hook around the tendon, providing distal traction, an arthroscopy probe is used to palpate its inferior and medial surface for vinculi. There are usually two vinculi along the semitendinosus tendon, one distally near its insertion and one more proximally.109 Because the proximal vincula is not usually found more than 12 cm from the distal insertion into the tibia, it can be hooked and pulled out of the wound or divided close to the tendon, depending on its mobility. Once the vinculi have been divided, the tendon stripper is applied and 22 cm of tendon is harvested, with the instrument aimed at the ischial tuberosity. Prior to amputating the tendons, 50 mL of local anesthetic solution (40 mL of 0.5% bupivacaine with adrenaline diluted in 100 mL of normal saline, corrected for weight) is administered along the track of the tendon stripper through multiple percutaneous punctures using a 19-gauge spinal needle (Fig. 43-3). This provides significant postoperative pain relief from the graft harvesting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree