Chapter 47 Anterior Cruciate Ligament Reconstruction via the Anteromedial Portal and Single-Tunnel, Double-Bundle Techniques
Anterior Cruciate Ligament Reconstruction via the Anteromedial Portal
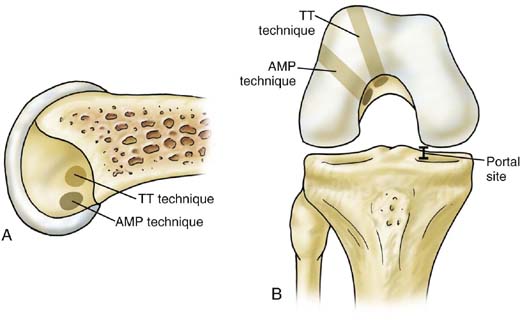
Use of the anteromedial portal (AMP) for establishment of the femoral tunnel in anterior cruciate ligament reconstruction (ACLR) surgery is an area of growing clinical and research interest. Traditionally, femoral tunnel creation has been performed by placing instruments through the previously reamed tibial tunnel. Several studies3–6,8,14,15,26 have suggested that use of the AMP eliminates the constraint in instrumentation positioning imposed by the transtibial technique, which can lead to the creation of a more vertical femoral tunnel or one with a nonanatomic aperture. The AMP is meant to allow for more anatomic, lower placement of the femoral tunnel and better re-creation of the native origins of the anteromedial and posterolateral bundles on the femoral condyle. However, some reports3,19,20 have underscored the technical challenges and steep learning curve associated with application of the AMP technique. Complications that have been described include lateral femoral condyle back wall blowout, iatrogenic damage to the anterolateral cartilage of the medial femoral condyle (MFC), bending or breakage of the guide pin or Beath pin, and difficulty with graft passage.
Additionally, technical considerations related to graft-length mismatch, shortening of femoral tunnel length, and inadequate femoral tunnel fixation can arise with use of the AMP technique. Because the femoral tunnel angle is typically smaller, or less steep, than that used with the transtibial technique, and because the tunnel is directed toward the lateral cortex, rather than the anterior cortex, of the distal femur, the length of the femoral tunnel is generally shorter. With the use of bone-patellar tendon-bone (BPTB) grafts, either autograft or allograft, shorter femoral tunnel length can cause the graft to be longer than the overall distance from the proximal extent of the femoral tunnel to the distal extent of the tibial tunnel on the anterior cortex of the tibia—that is, graft-length mismatch. Although this situation is rarely seen with the technique to be described, detailed preoperative planning can avoid this pitfall13 and several approaches can be used to address it when it occurs. Shortening of the bone plug lengths, seating the distal end of the femoral bone plug several millimeters deep to the aperture of the femoral tunnel, use of a free tibial bone block, and rotation of the tibial bone plug within the tibial tunnel are all acceptable, well-described techniques for addressing length issues and should be familiar to surgeons performing ACLR.34,35
When using soft tissue grafts, there are a number of options for femoral fixation. The growing popularity of the AMP technique and its shorter femoral tunnel has increased the demand for soft tissue fixation constructs with flexibility in length. For example, because the commonly used EndoButton CL (Smith & Nephew, Andover, Mass) uses suspensory cortical fixation and the construct contains a continuous loop of suture, with a minimum length of 15 mm, shorter femoral tunnels may leave a relatively short or unsatisfactory amount of graft contained within the tunnel. The newer EndoButton Direct (Smith & Nephew) device allows direct fixation of the graft onto the button, which maximizes the amount of graft in the femoral tunnel and may therefore be better suited for AMP techniques. The ACL Tightrope (Arthrex, Naples, Fla) is another suspensory fixation option for soft tissue grafts and allows the doubled-over end of the graft to be advanced to the most proximal aspect of the femoral tunnel. The Femoral Intrafix (DePuy Mitek, Raynham, Mass) uses aperture fixation via a sheath and screw construct. Because it allows for separation of different portions of the graft, thereby replicating the two bundles,10 it represents the senior author’s current implant of choice when using the AMP technique with soft tissue grafts. The AperFix femoral implant (Cayenne Medical, Scottsdale, Ariz) can also offer aperture fixation. However, AMP technique with this device requires a slightly larger portal, because both the implant and all graft limbs must be passed through the portal, and the smallest length of the implant is 29 mm, requiring a femoral tunnel length of at least 30 to 35 mm.
Technique
Creation of an appropriately located anteromedial portal is the most essential, primary step in ACLR surgery that uses the AMP technique (Fig. 47-1). Although some favor the use of an accessory AMP, we prefer instead to use a single AMP that is slightly more inferior than the standard portal in ACLR. The only exception to this approach is the need to perform a concomitant procedure that requires standard portal placement, such as meniscal repair, in which case two AMP portal incisions may be made. In this scenario, the first portal is established 1 to 2 mm inferior to the inferomedial pole of the patella and the second, femoral tunnel–creating AMP is 1 to 2 mm superior to the superior rim of the tibial plateau. Arthroscopic visualization of AMP creation from a standard anterolateral portal (ALP) is advised to avoid damage to the anterior horn of the medial meniscus, given the relatively inferior position of the AMP. In addition, some surgeons have recommended a more medial position of the portal compared with the AMP placement typically used in ACLR. However, we have found that damage to the cartilage of the medial femoral condyle can be a significant complication that is best avoided with AMP placement 2 to 3 mm medial to the medial edge of the patellar tendon.
A similar approach as described for the tibial footprint is used to identify and mark the center of the femoral ACL footprint. The soft tissues are then completely débrided from the lateral wall of the intercondylar notch while preserving the mark for the center of the footprint. An arthroscopic probe is used to identify the back wall of the femoral condyle definitively to avoid back wall blowout. The AMP is used to introduce the offset femoral guide and the guide wire as a unit past the medial femoral condyle, just as Cain and colleagues8 initially described introduction of the guide wire and reamer as a unit. The knee must be hyperflexed 110 to 120 degrees to allow the trajectory of the guide wire directly into the center of the femoral footprint. Alternatively, flexible guide pins and reamers have been introduced in an effort to avoid the need for hyperflexion, minimize articular cartilage damage on the medial femoral condyle, and allow the length of the femoral tunnel to be maximized via a more proximally directed orientation. The guide wire is advanced to the level of the anterolateral femoral cortex and the offset guide is removed. A second guide wire is introduced through the AMP to the femoral footprint, just adjacent and parallel to the first, to allow for measurement of the approximate length from footprint to cortex to ensure adequate tunnel length. If insufficient tunnel length is anticipated, the angle of the guide wire can be altered to increase tunnel length or other techniques to address mismatch can be planned, such as slight shortening of one or both bone plugs, depending on the estimated length. The second guide wire is removed and the reamer is then introduced into the notch under arthroscopic visualization, taking care to avoid damage to the MFC cartilage by the edges of the reamer.
Discussion
Despite its advantages in revision or double-bundle procedures, use of the AMP may have its greatest role as a new standard technique in primary ACL reconstruction, given the increasingly recognized importance of femoral tunnel position on restoration of native knee kinematics.10,39,40 Despite the technical challenges associated with its use, complications can be avoided by a thorough understanding of the potential pitfalls and technical principles. Critical to success with AMP techniques are an understanding of native footprint anatomy, appropriate inferior AMP placement, introduction and advancement of instruments into the joint and notch under arthroscopic visualization, meticulous measurements of graft and tunnel length, and experience with appropriate flexion and hyperflexion angles of the knee for the different portions of the procedure. Although more clinical outcomes studies related to use of this technique are warranted, early, lower level evidence, cadaveric studies, and descriptions of its technique have been favorable.4,5,12,14,19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree