Anterior Cervical Discectomy and Fusion
Christopher K. Kepler
Todd J. Albert
INDICATIONS/CONTRAINDICATIONS
Anterior cervical discectomy and fusion (ACDF) is indicated to relieve anterior-based compression of either the spinal cord or nerve roots causing (a) cervical radiculopathy unresponsive to 8 to 12 weeks of nonoperative treatment; (b) cervical radiculopathy with a progressive neurologic deficit; or (c) cervical myelopathy. Prior to any surgical procedure, appropriate imaging studies must be obtained that demonstrate neural element compression that is consistent with the patient’s clinical presentation. Although expectant management is sometimes employed by spine surgeons in the treatment of cervical myelopathy, it is our practice to operate on patients with myelopathy in a relatively expedient manner given the relative frequency of progression of symptoms and the uncertain recovery of function. Additionally, ACDF may be performed to treat certain traumatic injuries including central cord syndrome and some types of extension-distraction injuries.
Contraindications to ACDF include (a) anterior compression that is not confined to the disc space or the area immediately adjacent to the disc space and (b) anatomic or approach-related concerns that preclude anterior surgery. A relative contraindication is the requirement for decompression at more than three levels because of the increasing risk of nonunion with more operative levels.
PREOPERATIVE PLANNING
Prior to indicating patients for surgery, the surgeon must take a careful history and perform a physical examination with the goal of determining what spinal levels are likely to be causing the patient’s presenting signs and symptoms. Concordance between the patient’s presentation and imaging findings is increasingly important as improvements in magnetic resonance imaging (MRI) allows detailed anatomic visualization and frequently identifies spine pathology in asymptomatic individuals (1).
Disc herniation or spondylosis at the C2-C3 level leads to compression of the C3 nerve root, which does not have a motor component. C3 radiculopathy is most often manifested as pain but is rare, in part due to the relative capaciousness of the spinal canal at this level. C3-C4 disease causing C4 radiculopathy also lacks a motor component but typically results in pain along the top of the shoulder or trapezius region. C4-C5 disc herniation or spondylosis causes C5 radiculopathy which is most often associated with weakness of the deltoid and pain/numbness in the upper arm that may radiate into the radial aspect of the forearm. Disc herniation or spondylosis at C5-C6 leads to a C6 radiculopathy. Patients with C6 radiculopathy present with weakness in the biceps or wrist extensors, decreased or absent biceps tendon reflex, and forearm and hand pain/numbness, classically including the thumb and forefinger. C6-C7 is the most commonly affected cervical level and causes a C7 radiculopathy that most commonly leads to triceps or wrist flexion weakness, diminished triceps reflexes, and forearm or hand pain/numbness affecting the long finger. Finally, C8 radiculopathy is caused by either disc herniation or spondylosis at the C7-T1 level and results in finger flexion weakness and pain/numbness in the forearm extending into the ring and small fingers.
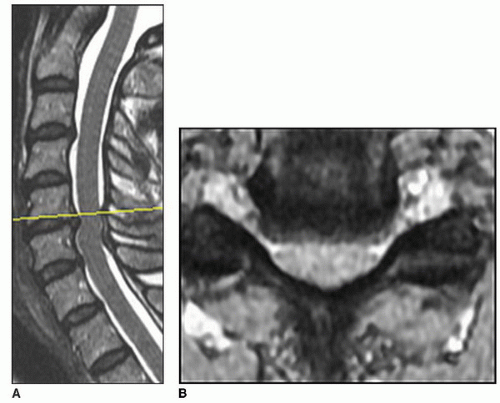 FIGURE 2-1 Sagittal (A) and axial (B) T2-weighted MRI images demonstrating large herniated disc at C5-C6 causing spinal cord compression. |
Patient with cervical myelopathy may or may not also complain of symptoms of cervical radiculopathy in which case localization of levels may be done as described above. Common presenting symptoms of patients with cervical myelopathy include imbalance, difficulty with fine motor tasks, generalized bilateral hand numbness, and difficulty holding objects. More rarely, patients complain of urinary or bowel symptoms. Pertinent exam findings include the presence of pathologic reflexes such as Hoffmann sign or Babinski sign, diminished upper extremity reflexes and enhanced lower extremity reflexes, or ankle clonus.
All patients should initially undergo anteroposterior, neutral lateral, flexion lateral, and extension lateral radiographs. Plain radiographs are essential to evaluate the standing alignment of the cervical spine, identify levels of dynamic instability, and evaluate for the presence of congenital stenosis. Patients who cannot extend to at least neutral cervical alignment must undergo anterior column reconstruction and should not be treated solely via posterior-approach surgery as laminectomy will not decompress the spinal cord in a kyphotic spine. MRI is most commonly used to evaluate the degree and location of neural element compression (Fig. 2-1), but computed tomography scan may be used in those patients with contraindications to MRI, preferably after myelogram to improve identification of sites with compressive lesions.
Surgical levels for patients being treated for radiculopathy should be selected based on concordance between presenting symptoms and imaging findings. When patients are being treated for myelopathy, all levels causing spinal cord compression should be addressed to offer the best chance to arrest symptoms. Finally, it is our practice to carefully consider inclusion of adjacent levels with advanced degeneration that are indeterminate with regard to contribution to radiculopathic symptoms. Hilibrand et al. demonstrated that such levels in the adjacent cervical spine are likely to continue to degenerate, resulting in adjacent-level disease (2).
TECHNIQUE
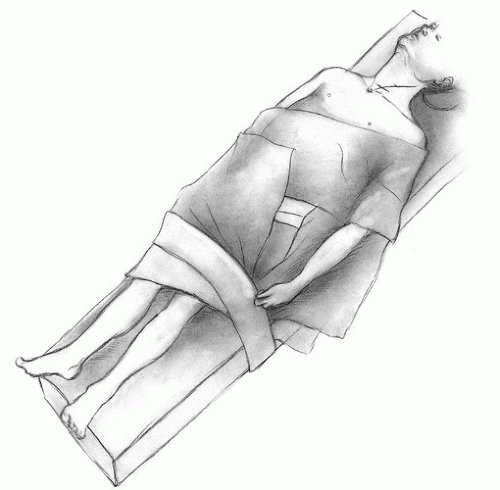
General anesthesia is administered, and the endotracheal tube is taped at the corner of the patient’s mouth and retracted contralaterally and superiorly. The authors’ preference for primary ACDF is to tape the tube in the right corner of the mouth to facilitate a left-sided approach in order to minimize the risk of injury to the recurrent laryngeal nerve as this structure is more reliably protected within the tracheoesophageal interval on the left side. Care should be taken that a line connecting the bottom lip and the inferior aspect of the ear is free of tape as this will define the superior border of the surgical field. Next, bony prominences and any intravenous lines are padded, and
the arms are tucked at the sides. The neuromonitoring personnel should obtain a postintubation, prepositioning set of motor evoked potentials to establish baseline readings. Next the shoulders are retracted inferiorly using tape to optimize visualization on the localization radiograph. The neck is extended to open the disc spaces anteriorly via increased lordosis (Fig. 2-2). This maneuver, however, slightly decreases the cross-sectional area of the central canal, so a set of motor evoked potentials should be obtained after final positioning. If there is any decrease in signal amplitude, the neck position is adjusted into less or no extension and the motor evoked potentials are rechecked. The draping should include both sternocleidomastoid (SCM) muscles and the sternal notch in the surgical field, and the iliac crest should also be prepped and draped if autograft bone is to be used.
the arms are tucked at the sides. The neuromonitoring personnel should obtain a postintubation, prepositioning set of motor evoked potentials to establish baseline readings. Next the shoulders are retracted inferiorly using tape to optimize visualization on the localization radiograph. The neck is extended to open the disc spaces anteriorly via increased lordosis (Fig. 2-2). This maneuver, however, slightly decreases the cross-sectional area of the central canal, so a set of motor evoked potentials should be obtained after final positioning. If there is any decrease in signal amplitude, the neck position is adjusted into less or no extension and the motor evoked potentials are rechecked. The draping should include both sternocleidomastoid (SCM) muscles and the sternal notch in the surgical field, and the iliac crest should also be prepped and draped if autograft bone is to be used.
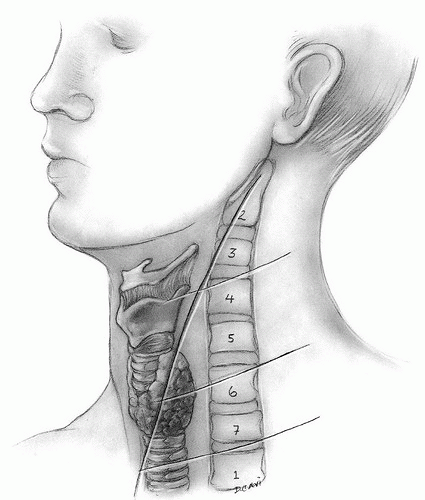
Next, the location of the incision should be planned based on anatomic landmarks. It is our preference to primarily consider the location of the carotid tubercle in planning the incision as it is the only commonly used landmark that is actually part of the spine. The carotid tubercle is the anterior tubercle of the transverse process of the sixth cervical vertebra and lies approximately at the level of the C5-C6 intervertebral disc. While palpating the tubercle, the surgeon should watch the vital signs as inadvertent pressure on the carotid sheath may trigger a vagal response and cause bradycardia. Superficial landmarks are also commonly used to guide the incision and include the hyoid bone around the level of C3, the thyroid cartilage that spans C4 and C5, and the cricoid cartilage at C6 (Fig. 2-3). It is the authors’ observation that these landmarks are variable and should be used in conjunction with other points of reference whenever possible. The skin incision may be made in either a transverse or oblique orientation. The transverse incision is more cosmetic while the oblique incision is more extensile. We prefer the transverse incision and feel that up to fourlevel ACDF can typically be performed through a transverse incision provided that the incision is carried a few millimeters medially past the midline and laterally to the medial border of the SCM. An oblique incision is made along the medial border of the SCM.
After the skin incision is made, the underlying fat is bluntly dissected off of the underlying platysma muscle. We prefer to divide the platysma in line with the skin incision (Fig. 2-4). Small flaps are raised above and below the platysma to assist in identification of this layer during closure. Next the interval between the strap muscles medially and the SCM laterally is identified by dissecting using Metzenbaum scissors (Fig. 2-5). Release of connective tissue that overlies the interval between the strap muscles and the SCM is critical when utilizing a transverse incision for more than two-level ACDF. Surgeons performing procedures in the lower cervical spine may encounter the omohyoid muscle belly passing obliquely from superomedial to inferolateral across the surgical field—this muscle may be transected using electrocautery to provide greater visualization (usually we do not find this necessary) of the spine but should be the only muscle transected beside the platysma. The carotid sheath is identified through gentle palpation of the patient’s pulse along the medial border of the SCM, and the anterior border of the spine can also be palpated medial to the carotid sheath. The interval between the medial border of the carotid sheath and the lateral border of the strap muscles should be freed throughout the entire extent of the incision to facilitate an extensile exposure of the spine (Fig. 2-6).
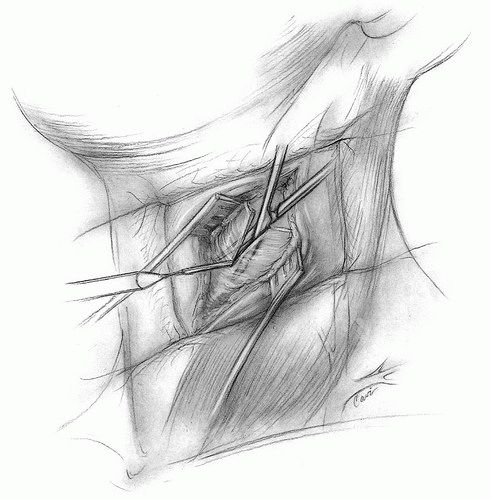 FIGURE 2-4 Transverse skin incision exposing the platysma muscle, which is incised transversely with electrocautery. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree