Anterior Thoracoscopic Discectomy
Thomas A. Zdeblick
INDICATIONS/CONTRAINDICATIONS
The primary indication for anterior thoracoscopic discectomy is disc herniation. The ideal indication for discectomy is myelopathy with cord compression caused by a central or lateral soft disc herniation. On occasion, discectomy is indicated for unremitting radicular or intercostal neuritic pain. The outcomes of discectomy, or discectomy plus fusion, for back pain alone are less certain. Hard discs, calcified discs, or lateral spurs may also cause myeloradiculopathy and may be amenable to anterior decompression (1,2,4,9). Other rare indications include débridement for disc space infection, vertebral body biopsy, and, on occasion, interbody fusion performed for pseudoarthrosis or degenerative disc disease (5,6). For conditions that necessitate corpectomy, I now perform a minithoracotomy with thoracoscopic assistance.
An absolute contraindication to thoracoscopic discectomy is the inability to tolerate single-lung ventilation (7). This may be present in older patients with interstitial lung disease or chronic obstructive pulmonary disease. Relative contraindications include previous thoracotomy, pleuritis, or pleurisy. Spinal levels that are amenable to thoracoscopic approach range from T3 to T11. However, this approach is more difficult at lower thoracic levels because retraction of the diaphragm and, on occasion, diaphragmatic division are required. Upper thoracic levels are difficult to reach if more than a simple release is required.
Technique
The side of pathology usually dictates whether the approach is right or left sided. With central herniations, I prefer a right-sided approach. The patient is positioned in the lateral decubitus position on a gel pad and beanbag. The ipsilateral arm is placed on an arm holder and extended superiorly (Fig. 17-1). Intubation with a double-lumen tube is a requirement. Bronchial blockers are usually not sufficient to maintain single-lung ventilation. To improve visualization, I usually roll the patient forward approximately 10 to 15 degrees (Fig. 17-2). This lets the lung fall slightly away from the vertebral column.
Fluoroscopy is utilized for initial portal placement. Three or four portals are typically utilized (Fig. 17-3). My preference is to use a posterior portal that is placed in the midaxillary line directly over the level of pathology and two anterior portals that are placed at the anterior axillary line (3,8). Usually, one of these is placed in line with the pathology, and the other is placed approximately two levels superiorly. This anterosuperior portal is typically placed first to avoid any chance of injuring the diaphragm. A 1-inch oblique skin incision is made just between the ribs, and sharp dissection is carried down to the intercostal muscle layer. Cautery is then utilized to make the initial division of the intercostal muscles. The ipsilateral lung is deflated, and the chest cavity is entered with a blunt clamp. A soft portal is placed in this anterior location. Thoracoscopic portals are typically 10 mm in diameter. Valves are not necessary. Each portal is placed using a blunt introducer. The remaining two or three portals can then be placed under direct vision, using the endoscope placed within the pleural cavity. After the skin incision, the approach to these portals is performed completely with cautery,
and I visualize the cautery coming through the pleura. Care should be taken that there is adequate space between the three portals in order to prevent “fencing.” In general, each portal should be at least 2 to 3 inches from the next nearest portal.
and I visualize the cautery coming through the pleura. Care should be taken that there is adequate space between the three portals in order to prevent “fencing.” In general, each portal should be at least 2 to 3 inches from the next nearest portal.
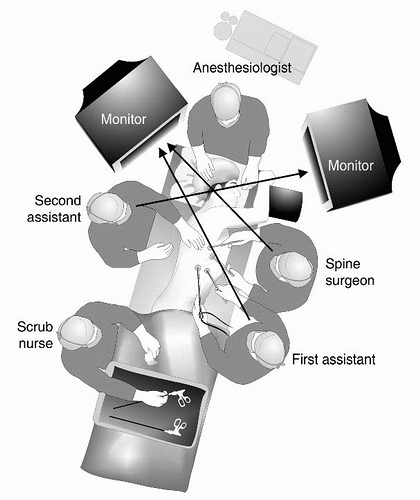
Usually, the lung can be retracted anteriorly using a fan retractor. Often, it stays in this retracted position, and the fan can be removed. However, if the lung does not fully deflate or remains an obstruction, a fourth portal can be placed anteriorly and inferiorly for the use of the fan retractor. Both the surgeon and the assistant typically stand on the ventral aspect of the patient (Fig. 17-1




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree