Chapter 74 Anesthesia for Knee Surgery
Intraoperative Anesthesia
Choice of Anesthetic Technique
Surgery on the knee is often performed using regional anesthetic techniques. Neural structures may be blocked at the neuraxial (spinal, epidural), plexus (psoas compartment), or peripheral nerve (femoral, lateral femoral cutaneous, sciatic) level. Regional anesthetics offer several advantages over general anesthetics for these patients, including improved postoperative analgesia, decreased incidence of nausea and vomiting, less respiratory and cardiac depression, improved perfusion via sympathetic block, reduced blood loss, and decreased risk of thromboembolism.33 The regional technique and the local anesthetic solution used depend on a variety of factors, including duration of surgery, degree of sensory and motor block desired, and length of postoperative analgesia. Surgical anesthesia for operative procedures on the knee in which a tourniquet will be used requires blockade of all four nerves (femoral, lateral femoral cutaneous, obturator, and sciatic nerves) innervating the leg. Although it is possible to perform major knee surgery under peripheral nerve block, more often a single-injection femoral or lumbar plexus (psoas compartment) block is combined with a spinal or general anesthetic. Spinal anesthesia can be accomplished with hyperbaric or isobaric solutions, although the latter are favored by most orthopedic anesthesiologists. Injection of hyperbaric solutions often results in a higher level of sensory and motor blockade than needed for the surgical procedure, with subsequent earlier offset of anesthesia. Epidural blockade offers the advantage of a continuous catheter technique that can be continued into the postoperative period. Patients with an absolute contraindication to regional anesthesia (patient refusal, infection at the site of needle placement, systemic anticoagulation) are candidates for general anesthesia. Thus, although knee surgery may be performed under general or regional anesthesia, the ability to provide superior postoperative analgesia, rapid postoperative rehabilitation, and reduced cost of medical care may result from thoughtfully implemented regional anesthetic and analgesic techniques.
Monitoring Requirements
Blood Loss and Pneumatic Tourniquet Inflation
Damage to underlying vessels, nerves, and muscles has been reported following tourniquet inflation.20 Injury is a function of both inflation pressure and duration of inflation.27,42 Direct pressure from the cuff is more damaging distally than the ischemia.35,42 Arterial spasm, venous thrombosis, and nerve injury are demonstrable after several hours. Clinical examination, electromyography, and effluent blood analysis all show completely reversible changes for inflation of 1 to 2 hours, which is the basis for the recommendation of this period as the safe duration for tourniquet use; longer inflation times are associated with prolonged or irreversible changes in neurologic and/or muscular function.22,25
Transient systemic metabolic acidosis and increased arterial carbon dioxide levels have been demonstrated after tourniquet deflation and do not cause deleterious effects in healthy patients. Prolonged inflation or the simultaneous release of bilateral tourniquets may produce clinically significant acidosis. Tourniquet release has also been associated with cerebral embolic phenomena.11
Postoperative Analgesia
Patients undergoing total joint arthroplasty experience significant postoperative pain. Failure to provide adequate analgesia impedes aggressive physical therapy and rehabilitation, which are critical to maintaining joint range of motion; this potentially delays hospital dismissal. Traditionally, postoperative analgesia following total joint replacement was provided by intravenous patient-controlled analgesia (PCA) or by epidural analgesia. Each technique has distinct advantages and disadvantages. For example, opioids do not consistently provide adequate pain relief and often cause sedation, constipation, nausea/vomiting, and pruritus. Epidural infusions containing local anesthetics (with or without an opioid) provide superior analgesia but are associated with hypotension, urinary retention, motor block limiting ambulation, and spinal hematoma secondary to anticoagulation. Single-dose and continuous peripheral nerve techniques that block the lumbar plexus (fascia iliaca, femurs, psoas compartment blocks) with/without sciatic nerve blockade have been used in this patient population.1,5,17,47 Several studies have reported that unilateral peripheral block provided a quality of analgesia and surgical outcomes similar to those of continuous epidural analgesia, but with fewer side effects.5,47 This suggests that continuous peripheral techniques may be the optimal analgesic method following total joint arthroplasty.
Multimodal Analgesia
Systemic Analgesics
Opioid Analgesics
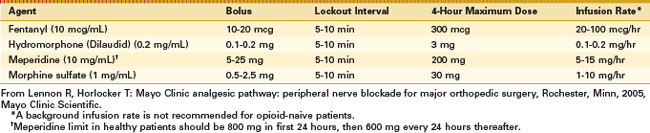
Adequate analgesia achieved with systemic opioids is frequently associated with side effects, including sedation, nausea, and pruritus. However, despite these well-defined side effects, opioid analgesics remain an integral component of postoperative pain relief. Systemic opioids may be administered by intravenous, intramuscular, and oral routes. Current analgesic regimens typically provide intravenous PCA for 24 to 48 hours postoperatively, with subsequent conversion to oral agents. The PCA device may be programmed for several variables, including bolus dose, lockout interval, and background infusion (Table 74-1). The optimal bolus dose is determined by the relative potency of the opioid; insufficient dosing results in inadequate analgesia, whereas excessive dosing increases the potential for side effects, including respiratory depression. Likewise, the lockout interval is based on the onset of analgesic effects; a lockout interval that is too short allows the patient to self-administer additional medication before achieving the full analgesic effect (and may result in accumulation/overdose of the opioid). A prolonged lockout interval will not allow adequate analgesia. The optimal bolus dose and lockout interval are not known, but ranges have been determined. Varying the settings within these ranges appears to have little effect on analgesia or side effects. Although most PCA devices allow the addition of a background infusion, routine use in adult opioid-naive patients is not recommended. However, background opioid infusion may have a role in opioid-tolerant patients. Because of variation in patient pain tolerance, PCA dosing regimens may have to be adjusted to maximize the benefits and to minimize the incidence of side effects.
Adverse effects of opioid administration can cause serious complications in patients undergoing major orthopedic procedures. In a systematic review, Wheeler and associates55 reported gastrointestinal side effects (nausea, vomiting, ileus) in 37%, cognitive effects (somnolence and dizziness) in 34%, pruritus in 15%, urinary retention in 16%, and respiratory depression in 2% of patients receiving PCA opioid analgesia.
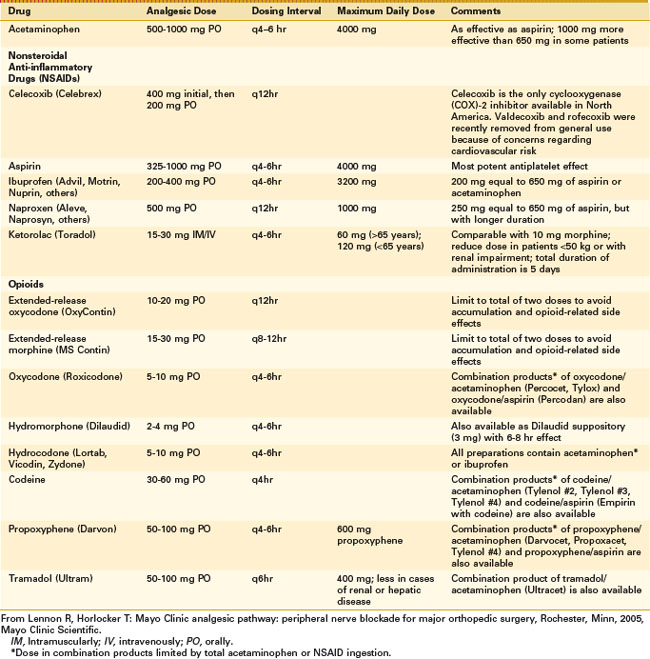
Oral opioids (Table 74-2) are available in immediate-release and controlled-release formulations. Although immediate-release oral opioids are effective in relieving moderate to severe pain, they must be administered as often as every 4 hours. When these medications are prescribed as needed (prn), delayed administration may be followed by increased pain. Furthermore, interruption of the dosing schedule, particularly during the night, may lead to an increase in the patient’s pain. The adverse effects of oral opioid administration are considerably fewer than those associated with intravenous administration, and they are mainly gastrointestinal in nature.55
Nonopioid Analgesics (Acetaminophen and Nonsteroidal Anti-Inflammatory Drugs)
The introduction of specific COX-2 inhibitors represented a breakthrough in the treatment of pain and inflammation. However, despite their efficacy, two (rofecoxib [Vioxx]; valdecoxib [Bextra]) of three COX-2 inhibitors were voluntarily removed from general use because of an increased relative risk for confirmed cardiovascular events, such as heart attack and stroke, after 18 months of treatment. Celecoxib (Celebrex) is currently the only COX-2 inhibitor available in the United States, although the Food and Drug Administration (FDA) has requested that safety information be included regarding potential cardiovascular and gastrointestinal risks for all selective and nonselective NSAIDs except aspirin.14
Although numerous NSAIDs have been used in the perioperative management of pain, ketorolac is the only NSAID that can be given parenterally. An intravenous dose of ketorolac 10 to 30 mg was found to have similar efficacy to 10 to 12 mg of intravenous morphine. In surgical patients, ketorolac reduces opioid consumption by 36%. Because of the potential for serious side effects, ketorolac should be used for 5 days or less in the adult population with moderate to severe acute pain.48
Major side effects limiting NSAID use for postoperative pain control (renal failure, platelet dysfunction, and gastric ulcers or bleeding) are related to nonspecific inhibition of the COX-1 enzyme.48 Advantages of COX-2 inhibitors include lack of platelet inhibition and a decreased incidence of gastrointestinal effects. All NSAIDs have the potential to cause serious renal impairment. Inhibition of the COX enzyme may have only minor effects in the healthy kidney but unfortunately can lead to serious side effects in elderly patients or those with a low-volume condition (blood loss, dehydration, cirrhosis, or heart failure). Therefore, NSAIDs should be used cautiously in patients with underlying renal dysfunction, specifically in the setting of volume depletion due to blood loss.48 Similar to COX-2 inhibitors, NSAIDs interfere with the inhibitory COX-1 effects of aspirin on platelet activity and may counter the cardioprotective effects.7
The effects of NSAIDs on bone formation and healing are of concern to the orthopedic population. Although the data are conflicting, evidence from animal studies indicates that COX-2 inhibitors may inhibit bone healing.15 Thus, adverse effects of COX-2 inhibitors must be weighed against their benefits. Until definitive human trials are performed, it is reasonable to be cautious regarding the use of COX-2 inhibitors, especially when bone healing is critical.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree