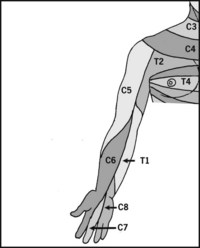
CHAPTER 2 Segmental and peripheral nerves of the limbs
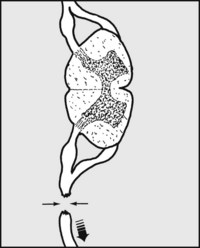
The Brachial Plexus: Cervical Part
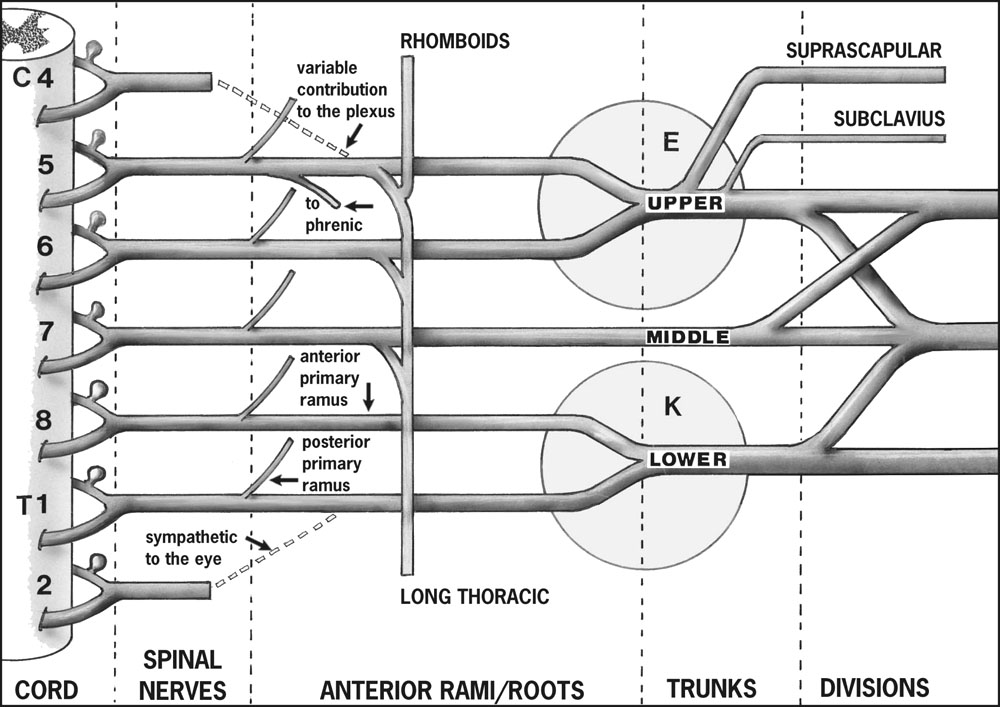
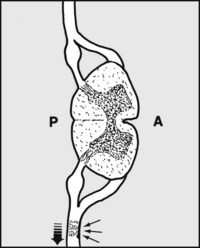
The brachial plexus has a most extensive distribution, and the order in which the nerves come off is of value in determining the site of any lesion. This is of particular importance in traumatic lesions, where the prognosis and treatment are closely related to the level of injury.
Branches from the Nerve Roots
Branches from the Trunks
There are two branches only at this level:
1. In Erb’s (upper obstetrical) palsy (E in Fig. 2.1) the C5–6 roots are affected but the nerve to rhomboids and the long thoracic nerve are spared.
2. In Klumpke’s (lower obstetrical) palsy (K in Fig. 2.1) the C8–T1 roots are involved. The sympathetic nerve supply to the eye (arising from T1) is often also affected, leading to a Horner’s syndrome. It was said that 80% of birth injuries to the plexus make a full recovery by 13 months, and persisting severe sensory or motor deficits in the hand are rare; recent work suggests that this view is somewhat optimistic. Note that a number of obstetrical injuries to the plexus are accompanied by facial nerve palsy and posterior dislocation of the shoulder.
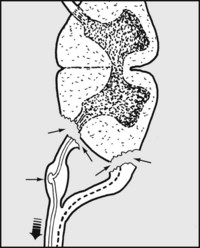
The Brachial Plexus: Axillary Part
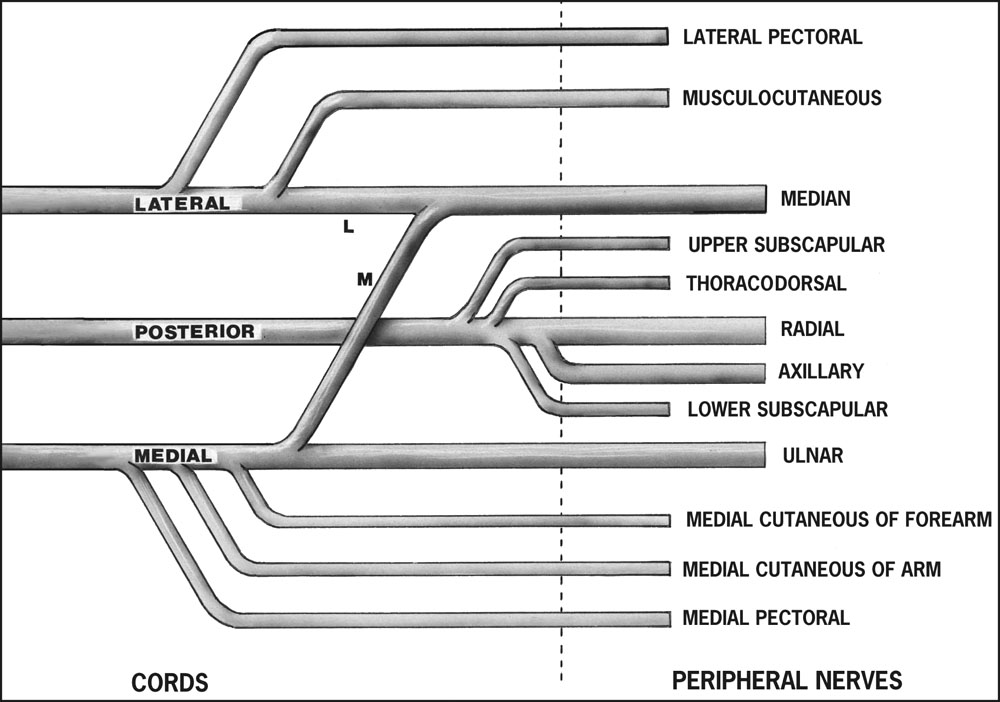
Branches from the Cords
The medial cord (C8, T1)
The posterior cord (C5, 6, 7, 8, T1)
Details of the most important branches (median, ulnar, radial, axillary) are given later.
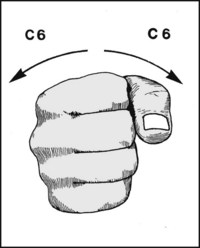
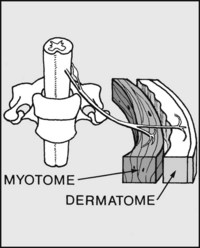
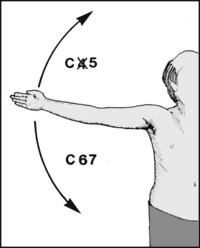
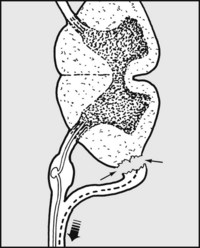
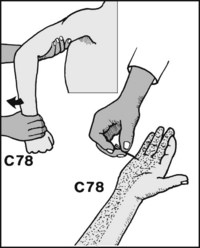
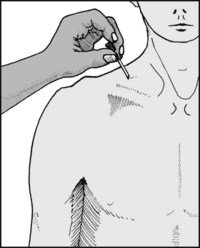
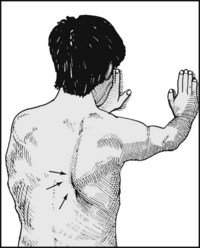
2.7. Myotomes (5):
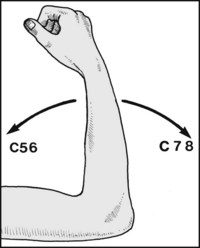
In the case of pronation and supination a single spinal segment is involved, namely C6.

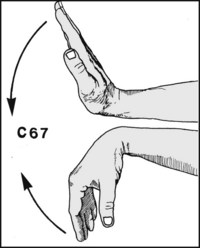
2.8. Myotomes (6):
A single segment again, namely T1, is involved in producing abduction and adduction of the fingers: these movements are carried out by the small muscles (intrinsics) of the hand. Note: In testing for myotomes the ability to perform the above movements should be assessed by MRC grading, and note made of the segments affected. Often the defect can be localised to a single segment.