CHAPTER 3 The cervical spine
Cervical Spondylosis (Cervical Osteoarthrosis: Osteoarthritis of The Cervical Spine)
In cervical spondylosis the cervical canal may be narrowed by osteophytic lipping of the facet or uncovertebral joints, by central disc herniations, by thickening of the ligamentum flava, or even from local cervical vertebral subluxations associated with ligamentous laxity. Developmental narrowing of the canal may be an additional factor. The reduction in the size of the canal may lead to cord compression (cervical spondylotic myelopathy). The disturbance of cord function that results may cause neck pain, difficulty in walking and unsteadiness on the feet, numbness, paraesthesia, weakness, and loss of upper limb dexterity. There is often coexisting compression of cervical nerve roots, leading to radicular symptoms which may complicate the clinical picture. Bladder dysfunction may occur, but is not common, and extensor plantar responses may appear late. Severe progressive myelopathy from spinal stenosis often requires operative treatment by decompression and stabilisation.
Whiplash and Extension Injuries of the Neck
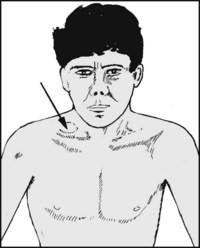
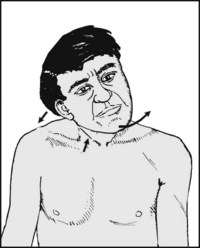
Whiplash injuries are now a common cause of persistent cervical symptoms. A true whiplash injury occurs classically when, as a result of a rear impact, a stationary or slowly moving vehicle strikes another vehicle or object in front. Because of the inertial mass of the head of the car occupant, there is rapid extension of the cervical spine followed by flexion. In the partial whiplash injury the main element is extension of the neck; this also commonly occurs as a result of a rear impact, but in this case the vehicle in which the occupant is travelling comes to rest more gradually, without striking anything ahead. Unfortunately, the attractive nature of the term has led to its misuse, and some recommend that because of its present imprecision it should be avoided altogether. If, however, it is going to be used, then it should be reserved for soft tissue injuries of the neck where extension is the main element. In the majority of cases the radiographs show normal alignment of the cervical vertebrae, but occasionally small avulsion fractures of the anterior margins of the vertebral bodies give evidence of the forcible extension of the spine. In some cases there are minor fractures involving the uncovertebral joints. Where there are spondylotic changes that interfere with the dissipation of the forces involved (because of localised areas of rigidity in the spine), there may be avulsion of anterior osteophytes. The flexion element may sometimes produce wedge compression fractures of the vertebral bodies or avulsion fractures of the spinous processes. Nevertheless, the discovery of unequivocal pathology in the spine is uncommon, and it is now apparent that there is a significant non-organic element in many cases. Although malingering does occasionally occur, this is considered to be rare. It is thought that in many cases a significant component of late disability is psychological, even if this is not at a conscious level, and that psychological elements and sometimes illness-related behaviour are often established within 3 months of injury.
Barré–Lieou Syndrome
This may follow a whiplash incident. There is complaint of headache, vertigo, tinnitus, ocular problems and facial pain. It is thought that it may be due to a sympathetic nerve disturbance at the C3–4 level, and in 75% of the cases there is impairment of sensation in the C4 dermatome, with weakness of shoulder and scapular movements. Myelography may show nerve root sleeve disturbances. Good results have been claimed for anterior discectomy combined with local cervical fusion.