Chapter 3 Anatomy Related to Spinal Subluxation
After reading this chapter you should be able to answer the following questions:
| Question 1 | What structures form the boundaries of the intervertebral foramen (IVF)? |
| Question 2 | What is radicular pain? |
| Question 3 | How might treatment of a subluxation decrease somatic referred pain? |
The relationships between the anatomic components of the spinal motion segment are critical to understanding the spinal subluxation model. This three-joint complex consists of the two zygapophyseal (posterior) joints and the (anterior) intervertebral disc. These structures interact to form the functional unit of the spine. The position of the intervertebral foramen provides a significant boundary between the central nervous system and the peripheral nervous system, and in some cases it may be structurally important to nociception arising from the spinal motion segment (subluxation-generated pain). Pain of spinal origin is transmitted through peripheral and central neural structures and is modulated at various sites.
The Zygapophyseal Joints
General Description
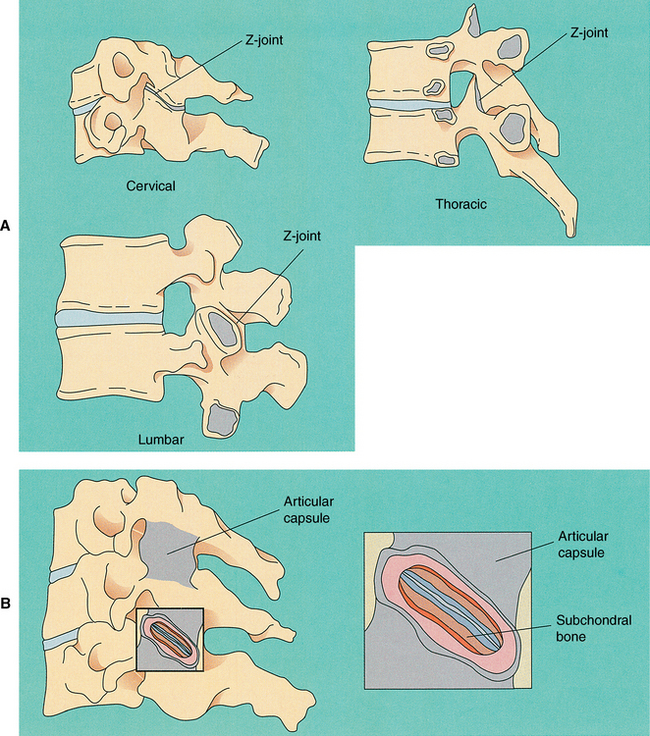
The junctions between the superior and inferior articular facets of the articular processes (zygapophyses) on either side of two adjacent vertebrae are known as zygapophyseal joints (Z-joint). These joints are also referred to as facet joints or interlaminar joints.1 There are left and right Z-joints between each pair of vertebrae and they are classified as synovial (diarthrodial) planar joints. These rather small joints allow motion to occur and, more importantly, determine the direction and limitations of movement that can occur between vertebrae. The Z-joint is of added interest to those who treat spinal conditions because loss of motion or aberrant motion may be a primary source of pain.2
Articular Capsules
Each Z-joint is surrounded by a capsule posterolaterally (Figure 3-1). The capsule consists of an outer layer of dense fibroelastic connective tissue, a vascular central layer made up of areolar tissue and loose connective tissue, and an inner layer consisting of a synovial membrane.3 The anterior and medial aspects of the Z-joint are covered by the ligamentum flavum. The synovial membrane lines the articular capsule, the ligamentum flavum,4 and the synovial joint folds (see following discussion), but not the articular cartilages of the joint surfaces.1
The Z-joint capsules throughout the vertebral column are thin and loose and are attached to the margins of opposing superior and inferior articular facets of adjacent vertebrae.5 Superior and inferior protrusions of the joint capsules known as recesses bulge out from the top and bottom of the joint. These recesses are filled with adipose tissue and the inferior recess is larger than the superior recess.6 The capsules are longer and looser in the cervical region than in the lumbar and thoracic regions to compensate for the greater amount of movement that occurs. As mentioned previously, the anteromedial aspect of the joint is formed by the ligamentum flavum,4 and hyaline cartilage covers the surface of each facet.
The Zygapophyseal Joint Synovial Folds
Zygapophyseal joint synovial folds are synovium-lined extensions of the capsule that protrude into the joint space to cover part of the hyaline cartilage. The synovial folds vary in size and shape in the different regions of the spine. Engle and Bogduk in 19827 reported on a study of 82 lumbar Z-joints. (Cervical folds are discussed later.) They found at least one intraarticular fold (meniscus) within each joint. The intraarticular structures were categorized into three types. The first was described as a connective tissue rim found running along the most peripheral edge of the entire joint. This connective tissue rim was lined by a synovial membrane. The second type of meniscus was described as an adipose tissue pad, and the third type was identified as a distinct, well-defined fibroadipose meniscoid. This latter type was usually found entering the joint from the superior or inferior pole of the joint (or both).
Giles and Taylor3 studied 30 zygapophyseal joints, all of which were found to have “menisci.” The “menisci” were renamed zygapophyseal joint synovial folds because of their histologic makeup. Free nerve endings were found within the folds, and the nerve endings met the criteria for pain receptors (nociceptors). That is, they were distant from blood vessels and were of proper diameter (6 to 12 μm). Therefore the synovial folds or menisci themselves were thought to be pain sensitive. This meant that if the Z-joint synovial fold became compressed by or trapped between the articular facets making up the Z-joint, back pain could result.
Unique Characteristics of the Cervical Zygapophyseal Joints
The cervical Z-joints are oriented approximately 45 degrees to the horizontal plane.8 More specifically, the facet joints of the upper cervical spine lie at approximately a 35-degree angle to the horizontal plane, and the lower cervical Z-joints form a 65-degree angle to the horizontal plane.9
Cervical Zygapophyseal Joint Synovial Folds
Zygapophyseal joint synovial folds (menisci) project into the Z-joints at all levels of the cervical spine. Yu et al.10 found four distinct types of cervical Z-joint menisci ranging from thin rims to thick protruding folds. They demonstrated several types of folds on magnetic resonance imaging scans.
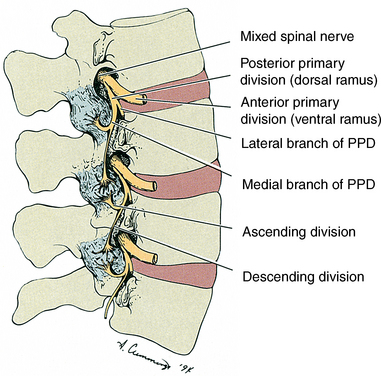
Innervation of the Z-Joints
The Z-joint capsule receives a rich supply of sensory innervation. The sensory supply is derived from the medial branch of the posterior primary division (dorsal ramus) at the level of the joint, and each joint also receives a branch from the posterior primary division of the level above (Figure 3-2). In addition, Wyke11 states that there are three types of sensory receptors in the joint capsule of the Z-joints. These are as follows:
• Type I—very sensitive static and dynamic mechanoreceptors that fire continually to some extent even when the joint is not moving
• Type II—less sensitive and fire only during movement
Type III sensory receptors are nociceptive fibers found in joints of the extremities, and Wyke11 did not find these in the Z-joints.
The Intervertebral Disc
The intervertebral disc (IVD) is composed of water, cells (primarily chondrocyte-like cells and fibroblasts), proteoglycan aggregates, and collagen fibers. The proteoglycan aggregates are composed of many proteoglycan monomers attached to a hyaluronic acid core. However, the proteoglycans of the IVD are of a smaller size and are of a different composition than the proteoglycans of cartilage found in other regions of the body (articular, nasal, and growth plate cartilage).12 The IVD is a dynamic structure that has been shown to repair itself and is capable of “considerable” regeneration.13
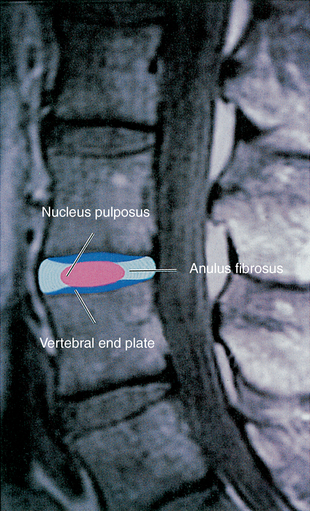
The IVD is composed of three regions known as the anulus fibrosus, the nucleus pulposus, and the vertebral (cartilage) end plate (Figure 3-3). Together they make up the anterior interbody joint or intervertebral symphysis. Each of these regions consists of different proportions of the primary materials that make up the disc. (See previous discussion.)
Anulus Fibrosus
The anulus fibrosus is made up of several fibrocartilaginous lamellae, or rings, which are convex externally. The lamellae are formed by closely arranged collagen fibers and a smaller percentage (10% of the dry weight) of elastic fibers.14 Most of the fibers of each lamella run parallel with one another at approximately a 65-degree angle from the vertical plane. Adjacent lamellae overlie one another, forming approximately a 130-degree angle between their fibers. The most superficial lamellae send thick bundles of collagen into the bone of the vertebral rims in the region of the ring apophysis. These bundles are known as Sharpey’s fibers. They form firm attachments between the intervertebral discs and the vertebral body. The inner lamellae of the anulus fibrosus attach to the cartilaginous vertebral end plate. The direction of the lamellae varies considerably from individual to individual and from one vertebra to the next.15
The lamellae of the anulus fibrosus are subject to tear. These tears occur in two directions, circumferentially and radially. Many investigators believe that circumferential tears are the most common. This type of tear represents a separation of adjacent lamellae of the anulus. The separation may cause the lamellae involved to tear away from their vertebral attachments. The second type of tear is radial in direction. These run from the deep lamellae to the superficial layers. Most authors16 believe that this type of tear develops after circumferential tears. The presence of circumferential tears may make it easier for radial tears to occur because radial tears can then connect several adjacent circumferential tears. When this occurs, the inner nucleus pulposus may bulge or be extruded into the vertebral canal. This is known as intervertebral disc protrusion (bulging) or herniation (extrusion). However, this scenario probably occurs much less frequently than was once believed.
Nucleus Pulposus
The nucleus pulposus is a rounded structure located in the center of the IVD. It develops from the embryologic notochord. The nucleus pulposus is gelatinous and relatively large just after birth, and several multinucleated notochordal cells can still be found within its substance.5
Except for the most peripheral region of the anulus fibrosus, the disc is an avascular structure. The nucleus pulposus is responsible for absorbing most of the fluid received by the disc. The process by which a disc absorbs fluid from the superior and inferior vertebral bodies has been termed imbibition. When a load is applied to the spine, an IVD loses water but retains sodium and potassium. This increase in electrolyte concentration creates an osmotic gradient that results in rapid rehydration when the loading of the disc is stopped.17
The disc apparently benefits from activity during the day and rest during the hours of sleep. As a result, the disc is thicker (from superior to inferior) after rest than after a typical day of sitting, standing, and walking. Too much rest may not be beneficial, however. A decrease in the amount of fluid (hydration) of the intervertebral discs has been noted on magnetic resonance imaging scans after five weeks of bed rest.18 The disc reaches its peak hydration at approximately the age of 30 years, and the process of degeneration begins shortly thereafter.19 As the disc ages, it becomes less gelatinous in consistency and its ability to absorb fluid diminishes. The changes in composition and structure caused by aging, common to all types of cartilage, occur earlier and to a greater extent in the IVD.20 Breakdown of the proteoglycan aggregates and monomers is thought to contribute to the process of degeneration because this process results in a decreased ability of the disc to absorb fluid. In turn, there is a decrease in the ability of the disc to resist loads to which it is subjected. The degeneration associated with decreased ability to absorb fluid (water) has been identified with computed tomography21 and magnetic resonance imaging and has been correlated with histologic structure and fluid content. As the disc degenerates, it becomes thinner (superior to inferior), and the adjacent vertebral bodies may become sclerotic (thickened and opaque on radiographs). Much of the disc thinning seen with age may also be the result of discs “sinking into” the adjacent vertebral bodies over the course of many years.15
Pathology of the intervertebral disc is seen frequently in clinical practice. As mentioned previously, the nucleus pulposus may cause bulging of the outer anular fibers or may protrude through the anulus. This was first described by Mixter and Barr.22 Bulging or herniation of the disc may be a primary source of pain, or pain may result from pressure on the exiting nerve roots in the vertebral or intervertebral foramens. Such bulging is usually associated with trauma, although a history of trauma may be absent in as many as 28% of patients with confirmed disc protrusion.23 Some investigators believe that proteoglycan leaks from tears in the anulus also may cause pain by creating chemical irritation of the exiting nerve roots. Pain caused by pressure on or irritation of a nerve root radiates in a dermatomal pattern. Such pain is termed radicular pain because of its origin from the dorsal root (radix) or dorsal root ganglion. Treatment for herniation of the nucleus ranges from conservative methods24 to excision of the disc (discectomy) to chemical degradation of the disc (chymopapain chemonucleolysis).25,26
Vertebral End Plate
Vertebral end plates are cartilaginous plates that limit the disc (with the exception of the most peripheral rim) superiorly and inferiorly and are attached to the nucleus pulposus, anulus fibrosus, and the adjacent vertebral body. Although a few authors consider the vertebral end plate to be a part of the vertebral body, most authorities consider it to be an integral portion of the disc.18,26 The end plates are approximately 1 mm thick peripherally and thicker centrally. They are composed of both hyaline cartilage and fibrocartilage. The hyaline cartilage is located against the vertebral body and the fibrocartilage is found adjacent to the remainder of the intervertebral disc. The end plates help to prevent the vertebral bodies from undergoing pressure atrophy and, at the same time, contain the anulus fibrosus and nucleus pulposus within their normal anatomic borders.27
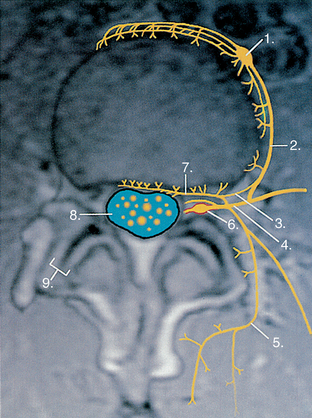
Innervation of Intervertebral Discs
The outer third of the anulus fibrosus receives both sensory and vasomotor innervation.28 The sensory fibers are probably both nociceptive (pain sensitive) and proprioceptive in nature, and the vasomotor fibers are associated with the small vessels located along the superficial aspect of the anulus fibrosus. The posterior aspect of the disc receives its innervation from the recurrent meningeal nerve (sinuvertebral nerve). The posterolateral aspect of the anulus receives both direct branches from the anterior primary division and also branches from the gray communicating rami of the sympathetic chain. The lateral and anterior aspects of the disc primarily receive innervation from branches of the gray communicating rami and also from branches of the sympathetic chain (Figure 3-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree