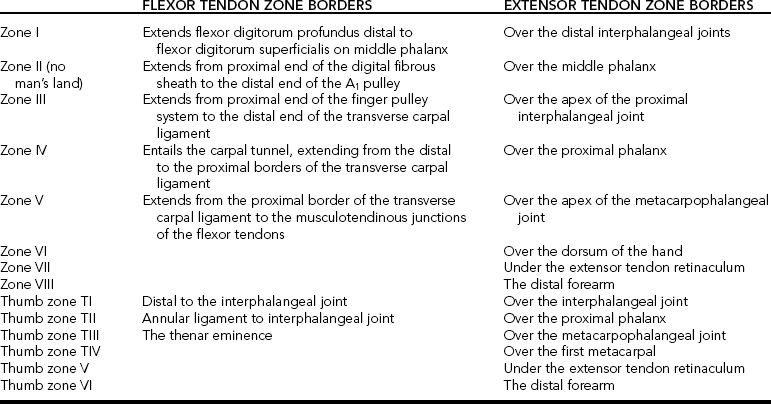
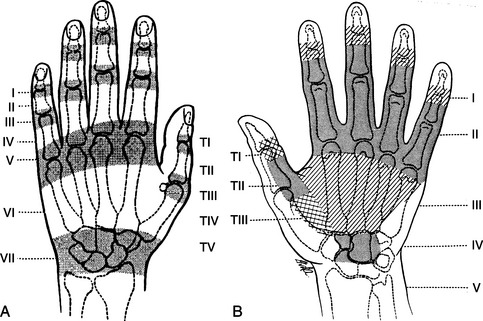
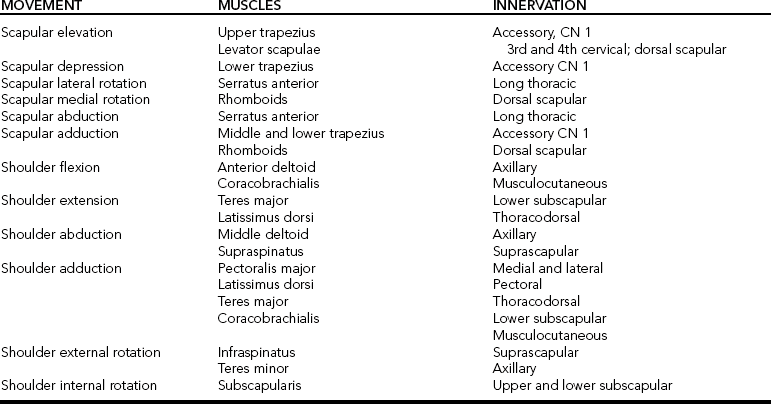
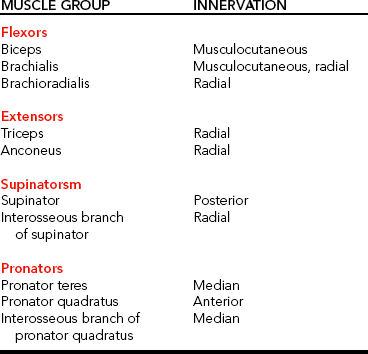
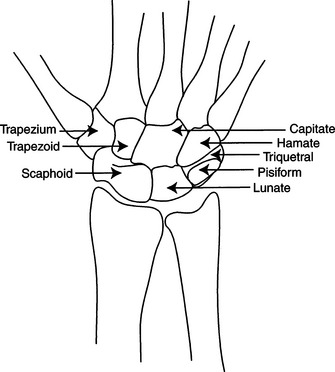
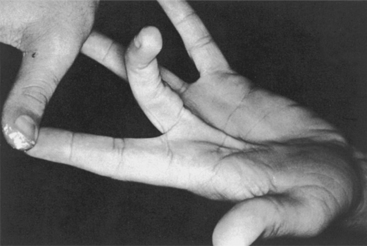
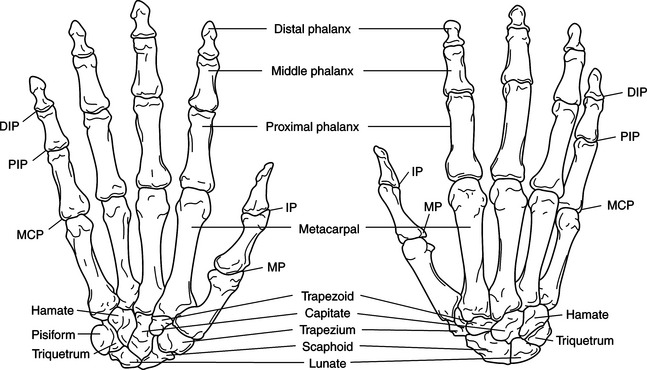
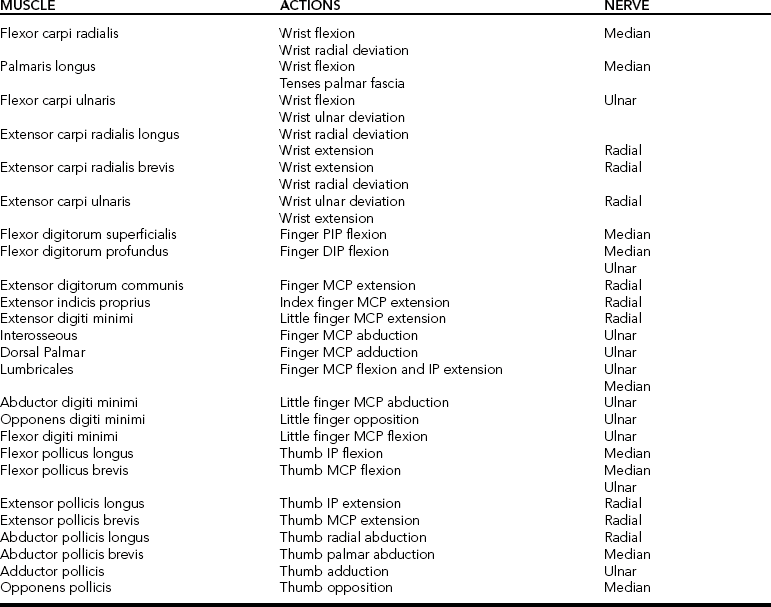
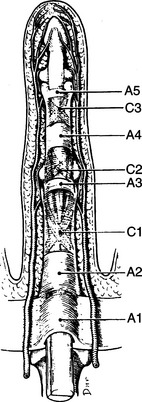
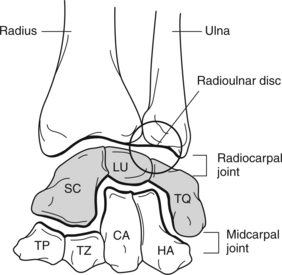
CHAPTER 4 1 Define the anatomical terminology used in splint prescriptions. 2 Relate anatomy of the upper extremity to splint design. 3 Identify arches of the hand. 4 Identify creases of the hand. 5 Articulate the importance of the hand’s arches and creases to splinting. 6 Recall actions and nerve innervations of upper extremity musculature. 7 Differentiate prehensile and grasp patterns of the hand. 8 Apply basic biomechanical principles to splint design. 9 Describe the correct width and length for a forearm splint. 10 Describe uses of padding in a splint. 11 Explain the reason splint edges should be rolled or flared. 12 Relate contour to splint fabrication. 13 Describe the change in skin and soft tissue mechanics with scar tissue, material application, edema, contractures, wounds, and infection. Splinting requires sound knowledge of anatomic terminology and structures, biomechanics, and the way in which pathologic conditions impair function. Knowledge of anatomic structures is necessary in the choice and fabrication of a splint. This knowledge also influences the therapeutic regimen and home program. The following is a brief overview of anatomic terminology, proximal-to-distal structures, and landmarks of the upper extremity pertinent to the splinting process. It is neither comprehensive nor all-inclusive. For more depth and breadth in anatomic review, access an anatomy text, anatomic atlas, or compact disk [Colditz and McGrouther 1998] showing anatomic structures. Knowing anatomic location terms is extremely important when a therapist receives a splint prescription or is reading professional literature. In rehabilitation settings, the word arm usually refers to the area from the shoulder to the elbow (humerus). The term antecubital fossa refers to the depression at the bend of the elbow. Forearm is used to describe the area from the elbow to the wrist, which includes the radius and ulna. Carpal or carpus refers to the wrist or the carpal bones. Different terminology can be used to refer to the thumb and fingers. Narrative names include thumb, index, middle or long, ring, and little fingers. A numbering system is used to refer to the digits (Figure 4-1). The thumb is digit 1, the index finger is digit II, the middle (or long) finger is digit III, the ring finger is digit IV, and the little finger is digit V. Literature addressing hand injuries and rehabilitation protocols often refers to zones of the hand.Figure 4-2 diagrams the zones of the hand [Kleinert et al. 1981].Table 4-1 presents the zones’ borders. Therapists should be familiar with these zones for understanding literature, conversing with other health providers, and documenting pertinent information. The shoulder complex comprises seven joints, including the glenohumeral, suprahumeral, acromioclavicular, scapulocostal, sternoclavicular, costosternal, and costovertebral joints [Cailliet 1981]. The suprahumeral and scapulocostal joints are pseudojoints, but they contribute to the shoulder’s function. Mobility of the shoulder is a compilation of all seven joints. Because the shoulder is extremely mobile, stability is sacrificed. This is evident when one considers that the head of the humerus articulates with approximately a third of the glenoid fossa. The shoulder complex allows motion in three planes, including flexion, extension, abduction, adduction, and internal and external rotation. A complex of ligaments and tendons provides stability to the shoulder. Shoulder ligaments are named according to the bones they connect. The ligaments of the shoulder complex include the coracohumeral ligament and the superior, middle, and inferior glenohumeral ligaments [Kapandji 1970]. The rotator cuff muscles contribute to the dynamic stability of the shoulder by compressing the humeral head into the glenoid fossa [Wu 1996]. The rotator cuff muscles include the supraspinatus, infraspinatus, teres minor, and subscapularis.Table 4-2 lists the muscles involved with scapular and shoulder movements. Muscles acting on the elbow can be categorized as functional groups: flexors, extensors, flexor-pronators, and extensor-supinators.Table 4-3 lists the muscles in these groups and their innervation. The carpal bones are arranged in two rows (Figure 4-3). The proximal row of carpal bones includes the scaphoid (navicular), lunate, and triquetrum. The pisiform bone is considered a sesamoid bone [Wu 1996]. The distal row of carpal bones comprises the trapezium, trapezoid, capitate, and hamate. The distal row of carpal bones articulates with the metacarpals. The radius articulates with the lunate and scaphoid in the proximal row of carpal bones. This articulation is the radiocarpal joint, which is mobile. The radiocarpal joint (Figure 4-4) is formed by the articulation of the distal head of the radius and the scaphoid and lunate bones. The ulnar styloid is attached to the triquetrum by a complex of ligaments and fibrocartilage. The ligaments bridge the ulna and radius and separate the distal radioulnar joint and the ulna from the radiocarpal joint. Motions of the radiocarpal joint include flexion, extension, and radial and ulnar deviation. The majority of wrist extension occurs at the midcarpal joint, with less movement occurring at the radiocarpal joint [Kapandji 1970]. The midcarpal joint (Figure 4-4) is the articulation between the distal and proximal carpal rows. The joint exists, although there are no interosseous ligaments between the proximal and distal rows of carpals [Buck 1995]. The joint capsules remain separate. However, the radiocarpal joint capsule attaches to the edge of the articular disk, which is distal to the ulna [Pratt 1991]. The wrist motions of flexion, extension, and radial and ulnar deviation also take place at this joint. The majority of wrist flexion occurs at the radiocarpal joint. The midcarpal joint contributes less movement for wrist flexion [Kapandji 1970]. Wrist stability is provided by the close-packed positions of the carpal bones and the interosseous ligaments [Wu 1996]. The intrinsic intercarpal ligaments connect carpal bone to carpal bone. The extrinsic ligaments of the carpal bones connect with the radius, ulna, and metacarpals. The ligaments on the volar aspect of the wrist are thick and strong, providing stability. The dorsal ligaments are thin and less developed [Wu 1996]. In addition, the intercarpal ligaments of the distal row form a stable fixed transverse arch [Chase 1990]. Ligaments of the wrist cover the volar, dorsal, radial, and ulnar areas. The ligaments in the wrist serve to stabilize joints, guide motion, limit motion, and transmit forces to the hand and forearm. These ligaments also assist in prevention of dislocations. The wrist contributes to the hand’s mobility and stability. Having two degrees of freedom (movements occur in two planes), the wrist is capable of flexing, extending, and deviating radially and ulnarly. Cutaneous and Connective Coverings of the Hand The skin is the protective covering of the body. There are unique characteristics of volar and dorsal skin, which are functionally relevant. The skin on the palmar surface of the hand is thick, immobile, and hairless. It contains sensory receptors and sweat glands. The palmar skin attaches to the underlying palmar aponeurosis, which facilitates grasp [Bowers and Tribuzi 1992]. Palmar skin is different from the skin on the dorsal surface of the hand. The dorsal skin is thin, supple, and quite mobile. Thus, it is often the site for edema accumulation. The skin on the dorsum of the hand accommodates to the extremes of the fingers’ flexion and extension movements. The hair follicles on the dorsum of the hand assist in protecting as well as activating touch receptors when the hair is moved slightly [Bowers and Tribuzi 1992]. The superficial layer of palmar fascia in the hand is thin. Its composition is highly fibrous and is tightly bound to the deep fascia. The deep fascia thickens at the wrist and forms the palmar carpal ligament and the flexor retinaculum. The fascia thins over the thenar and hypothenar eminences but thickens over the midpalmar area and on the volar surfaces of the fingers. The fascia forms the palmar aponeurosis and the fibrous digital sheaths [Buck 1995]. The superficial palmar aponeurosis consists of longitudinal fibers that are continuous with the flexor retinaculum and palmaris longus tendon. The flexor tendons course under the flexor retinaculum. With absence of the flexor retinaculum, as in carpal tunnel release, bowstringing (Figure 4-5) of the tendons may occur at the wrist level. The distal borders of the superficial palmar aponeurosis fuse with the fibrous digital sheaths. The deep layer of the aponeurosis consists of transverse fibers, which are continuous with the thenar and hypothenar fascias. Distally, the deep layer forms the superficial transverse metacarpal ligament [Buck 1995]. The extensor retinaculum is a fibrous band that bridges over the extensor tendons. The deep and superficial layers of the aponeurosis form this retinaculum. Functionally, the fascial structure of the hand protects, cushions, restrains, conforms, and maintains the hand’s arches [Bowers and Tribuzi 1992]. Therapists may splint persons with Dupuytren’s disease, in which the palmar fascia thickens and shortens. Splints often immobilize or mobilize joints of the fingers and thumb. Therefore, a therapist must have knowledge of these joints. The hand skeleton comprises five polyarticulated rays (Figure 4-6). The radial ray or first ray (thumb) is the shortest and includes three bones: a metacarpal and two phalanges. Joints of the thumb include the carpometacarpal (CMC) joint, the metacarpophalangeal (MCP) joint, and the interphalangeal (IP) joint (Figure 4-6). Functionally, the thumb is the most mobile of the digits. The thumb significantly enhances functional ability by its ability to oppose the pads of the fingers, which is needed for prehension and grasp. The thumb has three degrees of freedom, allowing for flexion, extension, abduction, adduction, and opposition. The second through fifth rays comprise four bones: a metacarpal and three phalanges. Joints of the fingers include the MCP joint, proximal interphalangeal (PIP) joint, and the distal interphalangeal (DIP) joint. The digits are unequal in length. However, their respective lengths contribute to the hand’s functional capabilities. During extension, the MCP joint is able to move medially and laterally. During MCP extension, collateral ligaments are slack. When digits II through V are extended at the MCP joints, finger abduction movement is free. Conversely, when the MCP joints of digits II through V are flexed abduction is extremely limited. The medial and lateral collateral ligaments of the metacarpal heads become taut and limit the distance by which the heads can be separated for abduction to occur. Mechanically, this provides stability during grasp. Table 4-4 provides a review of muscle actions and nerve supply of the wrist and hand [Clarkson and Gilewich 1989]. Muscles originating in the forearm are referred to as extrinsic muscles. Intrinsic muscles originate within the hand. Each group contributes to upper extremity function. Extrinsic muscles acting on the wrist and hand can be further categorized as extensor and flexor groups. Extrinsic muscles of the wrist and hand are listed inBox 4-1. Extrinsic flexor muscles are most prominent on the medial side of the upper forearm. The function of extrinsic flexor muscles includes flexion of joints between the muscles’ respective origin and insertion. Extrinsic muscles of the hand and forearm accomplish flexion and extension of the wrist and the phalanges (fingers). For example, the flexor digitorum superficialis flexes the PIP joints of digits II through V, whereas the flexor digitorum profundus primarily flexes the DIP joints of digits II through V. Because these tendons pass on the palmar side of the MCP joints, they tend to produce flexion of these joints. During grasp, flexion of the MCPs is necessary to obtain the proper shape of the hand. However, flexion of the wrist is undesirable because it decreases the grip force. The synergic contraction of the wrist extensors during finger flexion prevents wrist flexion during grasp. The force of the extensor contraction is proportionate to the strength of the grip. The stronger the grip the stronger the contraction of the wrist extensors [Smith et al. 1996]. Digit extension and flexion are a combined effort from extrinsic and intrinsic muscles. At the level of the wrist, the extensor tendons organize into six compartments [Fess et al. 2005]. The first compartment consists of tendons from the abductor pollicis longus (APL) and extensor pollicis brevis (EPB). When the radial side of the wrist is palpated, it is possible to feel the taut tendons of the APL and EPB. Unlike the other fingers, the index and little fingers have dual extensor systems comprising the EIP and the EDM in conjunction with the extensor digitorum communis. The EIP and EDM tendons lie on the ulnar side of the extensor digitorum communis tendons. Each finger has a flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) tendon. Five annular (or A) pulleys and four cruciate (or C) pulleys prevent the flexor tendons from bowstringing (Figure 4-7). The intrinsic muscles of the thumb and fingers are listed inBox 4-2. The intrinsic muscles are the muscles of the thenar and hypothenar eminences, the lumbricals, and the interossei. Intrinsic muscles can be grouped according to those of the thenar eminence, the hypothenar eminence, and the central muscles between the thenar and hypothenar eminences. The function of these intrinsic hand muscles produces flexion of the proximal phalanx and extension of the middle and distal phalanges, which contribute to the precise finger movements required for coordination.
Anatomic and Biomechanical Principles Related to Splinting
Basic Anatomical Review for Splinting
Terminology
Shoulder Joint
Elbow Joint
Wrist Joint
F. A. Davis.
Finger and Thumb Joints
Palmar Fascia
Joint Structure
Extrinsic Muscles of the Hand
Intrinsic Muscles of the Hand and Wrist
Anatomic and Biomechanical Principles Related to Splinting