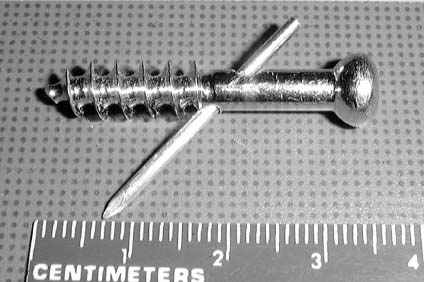
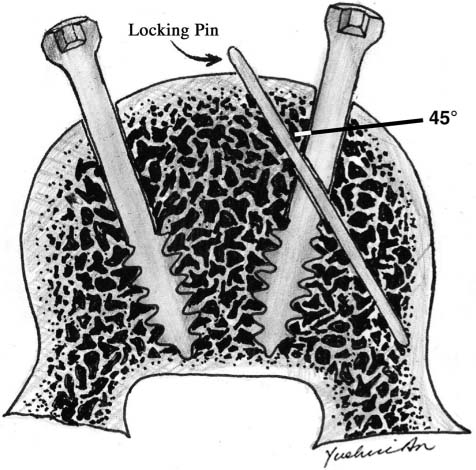
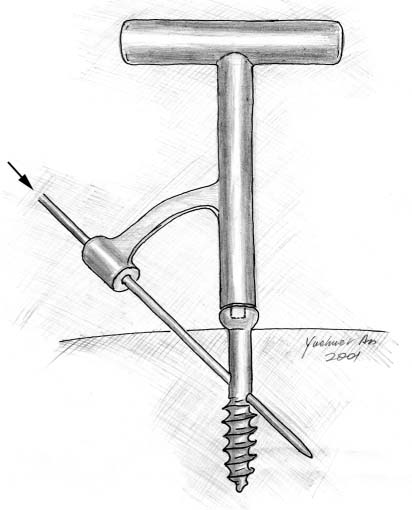
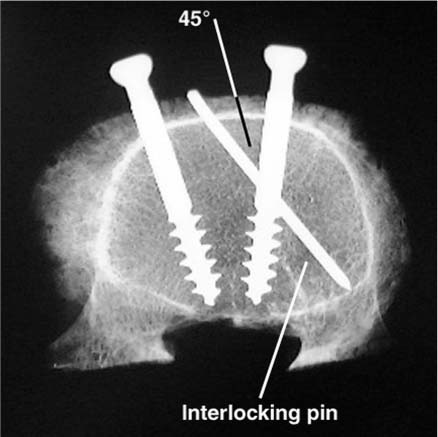
Chapter 20 Osteoporosis constitutes a major health problem through its association with age-related fractures. Patients with fragility fractures create a significant economic burden with more than 400,000 hospital admissions and 2.5 million physician visits per year.1 Adequate screw fixation in osteoporotic bone is a difficult and challenging surgical problem. Screw loosening and subsequent implant failure are major complications.2,3 The quality of bone has been shown to be the most important factor determining the ability of a screw to resist loosening.4 As the bone mineral density decreases, screws are unable to obtain adequate purchase, leading to a decreased holding power.5 In an effort to provide secure screw fixation, the effects of screw design,6,7 orientation,8,9 and cement augmentation10 on pullout strength have been evaluated. Polymethylmethacrylate (PMMA)11 and, recently, biodegradable calcium phosphate cements12 have been shown to increase the holding power of screws in osteoporotic bone. However, the use of cement is not without problems.13–15 PMMA is exothermic upon polymerization16 and toxic monomers can cause bone necrosis,17 proliferation of a fibrous tissue layer,18 and adverse biological responses.19 Cement-induced osteolysis may lead to eventual screw loosening and failure. In addition, another problem with PMMA is its lack of adhesion to bone.20 Although ceramic cements that solidify in situ have excellent biocompatibility, the mechanical properties of these cements are weaker than those of PMMA.21,22 We have developed a new screw locked with a K-wire for fixation in osteoporotic bone that does not require cement augmentation. The purpose of this study is to evaluate the ultimate holding power of the interlocking screw compared to a standard solid screw. Twenty 6.5 mm × 45 mm, partially threaded, solid stainless steel cancellous screws were obtained (Synthes, Paoli, PA). All screws had a pitch of 1.50 mm. Ten screws were used as solid controls. The other 10 screws were modified to produce the new locking screw design (Fig. 20–1). Twenty millimeters from the head of each screw a 1.9 mm hole was drilled through the shaft of the screw at a 45-degree angle. Both embalmed and fresh-frozen vertebral bodies were used in this in vitro study. Four osteoporotic fresh-frozen lumbar vertebral bodies were obtained from a 73-year-old Caucasian female. A dual energy X-ray absorptiometry (DEXA) scan was used to document the bone mineral density and T-score for each of the fresh-frozen specimens. Only specimens with a T-score of less than –2.50, which the World Health Organization defines as osteoporotic, were used in this study. The T-score compares the density of the bone being studied to that of a healthy 30-year-old female. Six embalmed lumbar vertebral bodies (L4 to L5) were also harvested from four cadavers with an average age of 70 years (three females and one male). FIGURE 20–1 Image of an interlocking screw. FIGURE 20–2 Line drawing of the interlocking screw fixed in the vertebral body. All soft tissues and posterior elements were removed from both the embalmed and fresh-frozen specimens. Two 4.73 mm diameter pilot holes were drilled 30 mm into each vertebral body from the anterior side. Although the anteroposterior (AP) diameter of each vertebra differed, no screw obtained bicortical purchase. One hole was drilled on the right side of the vertebral body, and the other hole was drilled on the left side the same distance from the midline. Both holes were drilled at a 30-degree angle toward the center of the vertebral body. Radiographs were taken to ensure neither hole crossed the midline. The solid screw and the new locking screw were inserted into the predrilled holes. The screws were randomized to the right or left side. The same vertebral body was used to test both screws to limit the effects of variability in bone density. The locking pin (1.9 mm smooth K-wire) was inserted through the 45-degree hole in the shaft of the screw, obtaining bone purchase proximally and distally (Fig. 20–2). The embalmed specimens were tested prior to the development of a guiding device. The concept of a right-angle triangle was used to free-hand the pin through the screw. The angle of the screw hole was drilled at 45 degrees, and the proximal portion of the hole was placed 1 cm from the bone surface, so the insertion site and angle for the pin were known. In the same plane as the mark previously made on the screw head, a K-wire was advanced 1 cm from the screw shaft at a 45-degree angle through bone, screw shaft, and bone. The pin was directed from medial to lateral in all cases. Before the fresh-frozen specimens were tested, a prototype guide to assist with pin placement was developed (Fig. 20–3). The guide was placed on the locking screw head after the hardware was inserted into the bone. This guide allowed all pins to be inserted on the first attempt without difficulty. To confirm the positioning of the screw and the interlocking pin, an X-ray was taken before mechanical testing (Fig. 20–4). FIGURE 20–3 The guide for interlocking pin insertion. Axial pullout tests were performed using a servo-controlled hydraulic mechanical testing system (MTS Systems, Minneapolis, MN). A fixture with a hole in the superior aspect for pulling out screws was constructed to hold the specimen during testing. The ultimate load to failure for both screws was determined. The MTS was run in stroke control (actuator displacement). Screws were pulled out at a displacement rate of 5 mm/min. The same procedure was followed for all 10 vertebral bodies. The order of pull-out was randomized between the solid and interlocking screws. The data were evaluated by using a paired Student’s t-test with each of the six vertebrae representing a pair. Statistical significance was set at P<0.05. FIGURE 20–4 Radiograph showing solid and inter-locking screws in a lumbar vertebral body.
AN INTERLOCKING SCREW FOR
FIXATION IN OSTEOPOROTIC BONE
SCREW DESIGN AND TESTING
SCREW PREPARATION
SPECIMEN PREPARATION
MECHANICAL TESTING AND EVALUATION
RESULTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree