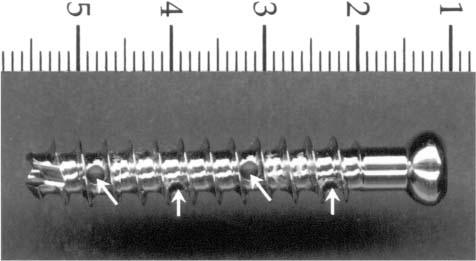
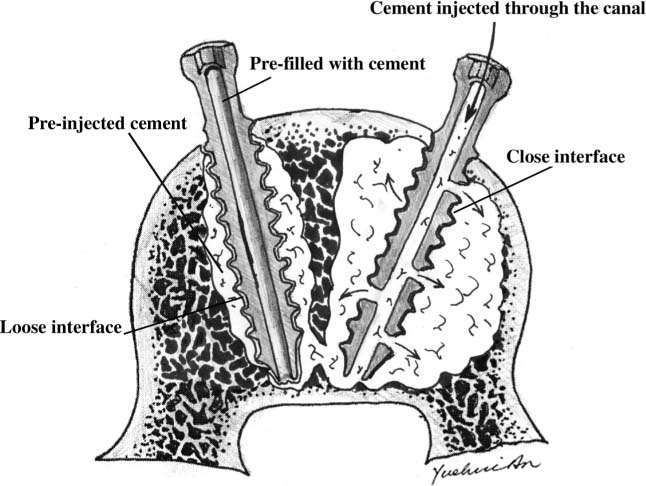
Chapter 21 Osteoporosis is a common bone disorder characterized by decreased bone mass and fragility fractures.1 According to the World Health Organization, 35% of women over 65 years of age in the United States have frank osteoporosis.2 One of every two Caucasian women will have an osteoporotic fracture during her lifetime.3 These osteoporotic fractures are a significant concern and account for the majority of the money spent on this condition.4 With the aging population, the prevalence of osteoporosis is expected to escalate. Not only is the population aging, but people are remaining healthy and active later in life. Nonoperative treatment of fractures in this age group is no longer the only treatment choice. Many orthopaedic surgeons are now performing internal fixation of fractures in octogenarians. However, because of the microarchitectural deterioration seen in this type of bone, adequate screw fixation is a difficult and challenging surgical problem. Several authors have reported on screw loosening and subsequent implant failure in osteoporotic bone.5,6 The most important factor determining the ability of a screw to resist loosening is bone quality.7 As bone mineral density decreases, so does the holding power of screws.8,9 In response to the difficulties of fixation in osteoporotic bone, surgeons have evaluated the effects of screw design,10,11 orientation,12,13 depth of penetration,14,15 and cement augmentation16 on pullout strength. Polymethylmethacrylate (PMMA)17 and, recently, biodegradable calcium phosphate cements18 have been shown to increase the holding power of screws in osteoporotic bone. If PMMA is used to augment screw fixation, a pilot hole is drilled, and the bone cement is injected prior to inserting a screw. However, this leads to variable cement mantles and poor penetration of the cement into the bone. PMMA has been shown to have poor adhesion to bone.19,20 Thus, cement that penetrates into the trabeculae may increase the holding power of the screw. Injectable cements have been used to provide screw fixation in osteoporotic bone. Vertebroplasty has been evaluated not only for treatment of compression fractures in osteoporotic vertebra but also as an adjunct to internal fixation of hardware.21 In this method, PMMA is injected into the vertebral body percutaneously. Brantley and Mayfield22 investigated a cannulated pedicle screw injected with cement for fixation in osteoporotic bone. We have modified this technique for use in other areas in osteoporotic bone, such as anterior spinal surgery. To further increase the holding power, our modifications consisted of adding holes to the shaft of the screw to allow cement to penetrate into the trabeculae of the bone. The purpose of the current in vitro study is to evaluate the ultimate holding power of the new cannulated screw injected with cement compared with a solid screw of the same dimensions augmented with cement. Twenty-six 7.3 mm × 40 mm, fully threaded, cannulated stainless steel screws were obtained (Synthes, Paoli, PA). All screws had a pitch of 1.50 mm with identical internal diameters. Thirteen of the screws were filled with PMMA to serve as solid controls, because a solid stainless steel screw with these dimensions was not commercially available. Thirteen of the cannulated screws were modified to produce the new screw design. Ports were made along the shaft of the screw between the threads with a 1.9 mm drill bit. Holes were only made through one wall of the cannulated screw. Consecutive ports were made along the entire shaft of the screw by rotating the screw approximately 30 degrees for a total of eight holes (Fig. 21–1). FIGURE 21–1 New cannulated screw with side holes (arrows indicate holes). Nine embalmed lumbar vertebral bodies (L3 to L5) were harvested from seven cadavers with an average age of 73 years (five females and two males). Four lumbar vertebral bodies (L1 to L3) were harvested from two fresh-frozen cadavers (two females; 65 and 67 years old). All soft tissues and posterior elements were removed from the specimens. Two 4.73 mm diameter pilot holes were drilled 30 mm into each vertebral body from the anterior side. The midline of each vertebral body was clearly marked. One hole was drilled on the right side of the vertebral body, and the other hole was drilled on the left side, both 20 mm from the midline measured with a digital caliper. The same distance was used for all specimens. Both holes were drilled at a 20-degree angle toward the center of the vertebral body. The holes were drilled with a drill press attached to a secure table. A wooden block with a 20-degree angle was secured to the drill press platform. The vertebral bodies were attached to the wooden block with the cut pedicles facing the platform. In this manner, all holes were drilled with a 20-degree angle plus or minus 3 degrees. Radiographs were taken to insure neither hole crossed the midline. A dual energy X-ray absorptiometry (DEXA) scan (Hologic, Bedford, MA) was used to document the bone mineral density of each fresh-frozen specimen.23 All fresh-frozen vertebral bodies had a T-score of less than –3.00. The World Health Organization defines osteoporotic bone as having a T-score less than –2.50.24 The T-score is the number of standard deviations from the mean bone density of a healthy 30-year-old female. In addition, the absolute numbers for the bone mineral density (g/cm2) and bone mineral content (g) were recorded for each fresh-frozen specimen. Tygon® tubing was attached to a 20 cc syringe for injecting the cement into the pilot hole of the solid screw. PMMA (Surgical Simplex P, Howmedica, Rutherford, NJ) was mixed for 2 minutes according to the manufacturer’s instructions to a viscosity that would allow injection (20 g powder + 10 mL of liquid monomer). The pilot hole for the solid screw was injected with approximately 0.5 to 1.5 mL of PMMA followed by insertion of the screw. Next, the pilot hole for the cannulated screw was injected with 0.5 to 1.5 mL of PMMA followed by insertion of the screw (Fig. 21–2). After insertion, 3.0 to 5.0 mL of PMMA was injected under pressure through the central canal of the screw. The cement was allowed to harden for 30 to 40 minutes before testing in the embalmed specimens and 24 hours for the fresh-frozen specimens. FIGURE 21–2 Illustration of the fixation mechanism of the cementing screw (arrows indicate side holes and the directions of cement flow). Axial pullout tests were performed using a servo-controlled hydraulic mechanical testing system (MTS Systems, Minneapolis, MN). A fixture with a hole in the superior aspect for pulling out screws was constructed to hold the specimen during testing. The ultimate load to failure for both screws was determined. The MTS was run in stroke control (actuator displacement). Screws were pulled out at a displacement rate of 5 mm/min. The same procedure was followed for all 13 vertebral bodies. The order of pull-out was alternated between the cannulated and solid screws. The data were evaluated by using a paired Student’s t-test with each of the 13 vertebrae representing a pair. Statistical significance was set at P<0.05. Each fresh-frozen vertebral body was sectioned after mechanical testing to document the penetration of cement into the bone. The reproducibility of this experimental setup was evaluated by pulling out a 4.5 mm cancellous screw from eight polyurethane blocks.25 The coefficient of variation was found to be only 3.7%. The mechanical properties of the new cannulated screw design were assessed. Three-point bending tests were performed on two cannulated screws and two of the modified cannulated screws to determine how much the screw was weakened by the addition of side ports. The tests were performed on the MTS in a stroke control mode with a compression rate of 1 mm/min. The two inferior posts of the three-point bending apparatus were placed 29 mm apart. In the embalmed specimens, the mean pullout force for the solid screw was 572.2 ± 542 N and for the new cannulated screw was 1011.1 ± 583 N. The cannulated design had a 77% increase in ultimate holding strength compared to the standard solid screw design. The paired Student’s t-test showed the difference to be statistically significant (P = 0.01). The pull-out values for the nine specimen pairs can be seen in Table 21–1. Radiographs taken before mechanical testing confirmed the screw position and the areas of injected cement (Fig. 21–3). The gross specimens revealed a substantial cement mantle surrounding the entire shaft in the cannulated screws with radial cement spokes from each port extending into the surrounding trabeculae. The solid screws had variable amounts of cement along the shaft with almost no extrusion of cement into the trabeculae of the cancellous bone.
AN INJECTABLE CEMENTING SCREW
FOR FIXATION IN
OSTEOPOROTIC BONE
SCREW DESIGN AND TESTING
SCREW PREPARATION
SPECIMEN PREPARATION
MECHANICAL TESTING AND EVALUATION
RESULTS