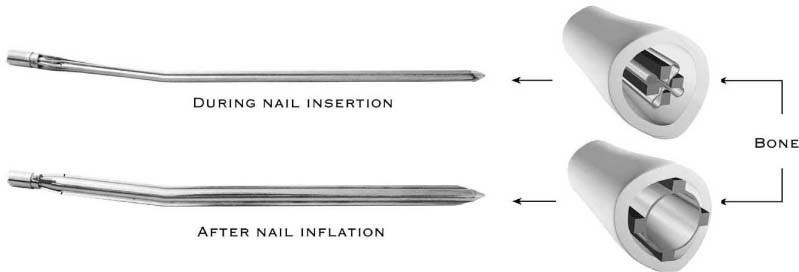
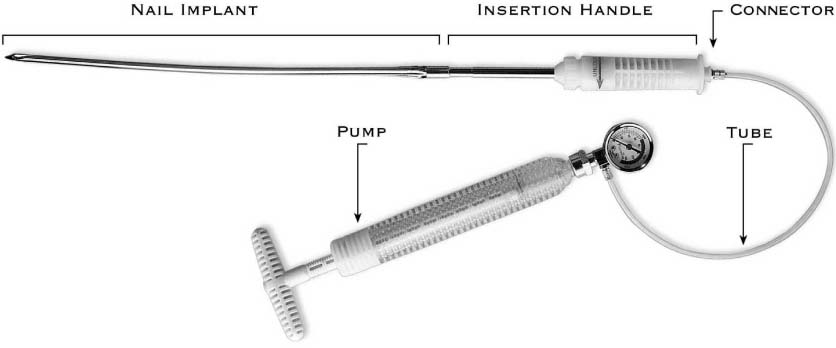
Chapter 30 The changes in long bone caused by osteoporosis are well described and include alterations in the proximal, metaphyseal, and diaphyseal areas. Fixation of fractures in osteoporotic bones is characteristically fraught with complications and problems. As the internal fixation devices are stronger than the bone, cutout, fracture below the implant, or implant failure are commonly observed. Fractures that have occurred in the midshaft of the long bone are not amenable to stabilization with either plating or external fixation. Intramedullary nailing with or without interlocking screws is currently the standard treatment of these fractures,1–3 a procedure that also entails complications mainly due to the large medullary canal that is pathognomonic in patients with osteoporosis. In addition, weakening of the bone by the use of interlocking screws may cause further fractures below the end of the nail. Despite the larger diameter of the medullary canal in osteoporotic bones, reaming is still necessary to introduce the largest intramedullary nail in the canal. Reaming, however, injures the medullary vascular system, resulting in relative avascularity of significant portions of the diaphyseal cortex.4–6 It also reduces the strength of the bone by 15 to 64%, depending upon the extent to which it is carried out.7–9 The drilling of a hole in a bone inevitably reduces its breaking strength. The presence of a screw also weakens the bone to the same extent as an unfilled hole, but this effect diminishes with the production of new bone.10 The osteoporotic bone in the distal femoral metaphysis can compromise distal locking screw purchase. Moran and coworkers3 supplemented their distal locking screws with intramedullary polymethylmethacrylate in several cases. However, because of the differences of stiffness that had been created, further fracture below the intramedullary nail became unavoidable. The need for reaming and fixing a distal locking screw significantly prolongs operative and fluoroscopy time. The threat of thromboembolism increases with the duration of the surgical procedure,11–13 as does the wound infection rate.14 Excessive radiation exposure to the surgeon’s hands and body are a major concern with closed intramedullary nailing: several studies have shown that the greatest dose of radiation occurs during nail insertion and distal targeting.15,16 The avoidance of both reaming and the use of an interlocking screw would directly reduce operative and fluoroscopy time and associated complications. An inflatable nail that can adapt itself to the changing diameter of the medullary canal and produce a satisfactory grip along the fractured bone would make reaming and interlocking screws unnecessary. The inflatable intramedullary nail expands within the medullary canal and does not require reaming or interlocking screws.17 It is a stainless steel, sealed pressure tube consisting of four longitudinal bars connected radially by four thinner stainless steel membranes. The implant is supplied in its small diameter configuration. Upon expansion, the nail is capable of increasing its diameter by more than 65% (range from 6.5 through 14 mm to 10 through 22 mm, for pre- and postinflation, respectively). The nail with the reduced diameter has flexible characteristics and is easily inserted into the medullary canal. Once in position, it is reexpanded by inflation under controlled pressure with saline (up to 70 bar). This expansion of the nail within the medullary canal causes abutment of the longitudinal bars to the inner surface of the canal along its entire length. The expanded nail adapts to the different shape and diameter of the medullary canal, resulting in excellent fixation of the fracture (Fig. 30–1). FIGURE 30–1 The inflatable-expandable nail during and after inflation. FIGURE 30–2 The inflatable intramedullary nailing system: the inflation pump, the insertion handle, and the nail. The inflatable nail is a single-use system that features three main components (Fig. 30–2): 1. The nail is a stainless steel construct with the shape of a thin-walled annealed tube with four longitudinal bars for reinforcement. The tube is sealed with a conically shaped cap at the distal end, and a female threaded cap containing an internal check valve at the proximal end (Fig. 30–1). The inflatable nail is provided with a specific longitudinal curvature for use in individual long bones (humerus, femur, or tibia), as well as different diameters and length. Sterile inflation liquid (saline), which is inserted into the nail through its check valve under fluoroscopy and controlled pressure, is used to expand the nail to the desired diameter. 2. The driver is a stainless steel tube that is cut at its distal end to create a male thread for connection to the nail implant’s proximal end. This tube is connected to the driver’s plastic handle. To prevent relative rotation movement between the driver and the nail during its insertion, a locking mechanism is activated on the driver’s plastic handle. A quick connector is located on the driver’s handle close to its distal end for connection to the inflation device. 3. The nail inflation pump is manually operated by rotation of its handle’s screw. An analog pressure gauge and a pipe joint, which is designed for quick connection to the driver, are installed at the pump outlet. Accessories to these components are the multiuse nail removal handle and the extractor, which when required enables the nail to be removed after deflation. Compared to other commercially available intramedullary fixation devices, the expandable nail’s bending stiffness was higher, its bending strength was similar (Table 30–1), and the torsional stiffness was equivalent or even greater (Table 30–2).17 Its torsional strength was tested in cadaveric bone and was found to be equivalent to that of the other intramedullary fixation devices.
AN EXPANDABLE
INTRAMEDULLARY NAIL FOR
FIXATION IN
OSTEOPOROTIC BONE
THE INFLATABLE NAIL
THE DESIGN
IN VITRO BIOMECHANICAL STUDIES
Nail | Average Bending Stiffness (N • m2) | Average Bending Strength (N • m) |
|---|---|---|
Inflatable 8/12.7 mm, humeral nail | 29.8 | 54.5 |
Inflatable 10/16 mm, tibial nail | 61.6 | 92.5 |
Inflatable 12/19 mm, femoral nail | 78.1 | 172.5 |
Note: The nail sizes in the table appear in abbreviation, x/y mm (x stands for the reduced nail diameter and y stands for the maximal inflated diameter).
Nail | Average Torsional Stiffness (N • m2) |
|---|---|
Inflatable 8/12.7 mm, humeral nail | 4.0 |
Inflatable 8.5/13.5 mm, tibial nail | 5.4 |
Inflatable 10/16 mm, tibial/femoral nail | 9.7 |
Inflatable 12/19 mm, femoral nail | 16.2 |
See Table 30–1 for nail size abbreviations.
The saline solution within the nail is a noncompressible liquid and, as such, causes the nail to expand, causing plastic deformation of its thin wall membranes. Once the nail is expanded, it assumes a final stable condition. Thus, the biomechanical properties of the nail after solution evacuation were found to be close to those of the intact inflated nail. Due to characteristics of the nail and the noncompressible saline, any leak of saline from the nail, however small, will cause its immediate internal pressure to drop to atmospheric pressure, without bone or tissue damage.
The bone-nail interface was also measured. Inflation of the nail up to 120 bar (170% of the manufacturer’s recommendation of 70 bar) caused no harm to the bone. The stresses exerted on the canal inner wall during inflation were significantly below the bone force resistance limits. The inflatable nail’s fatigue strength (500,000 cycles) was more than the expected duration of use until bone healing (assuming 1000 walking steps for patient per day for 1.5 years after implantation [1000 × 365 × 1.5 = 547,500]).
ANIMAL STUDY
Twenty-six healthy sheep were used for the animal experiment.18 A fracture was created in the midshaft of either the femur or tibia and fixed with the inflatable nail. Several observations were made during the nail’s insertion. First, inserting the nail in its narrow configuration was easy due to the small diameter. There were a few fracture angulations, which were possibly due to the small dimension of the nail, and they disappeared after inflation and expansion of the nail. Second, the nail often assumed the shape of an hourglass configuration; thus it expanded more in the wider part of the canal and less in the narrow part, adapting itself to the maximal diameter (Fig. 30–3).
All surgical procedures were carried out uneventfully and all the sheep were able to bear weight on the second or third postoperative day. Full weight bearing was achieved after 7 to 10 days after surgery. The first sign of healing of the fracture was evident at 10 to 14 days postoperatively, and complete healing was achieved after 50 days postoperatively. All the fractures healed uneventfully without loss of reduction.
One of the anticipated problems was the extraction of the nail after the fractures had healed but no such problem was encountered. This was due to the rapid decrease of pressure within the nail while removing the valve as well as to the ability of the nail to “collapse” along the narrow and thin walls. The low contact area between the nail and the intramedullary cavity also contributed to the ease of extraction.
FIGURE 30–3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree