Fig. 46.1
Macroglossia in a patient with AL amyloidosis. The tongue is firm to palpation. Note the non-reducible impression in the tongue caused by the teeth

Fig. 46.2
The same patient of Fig. 46.1. Periorbital purpura. Frequently the purpura is bilateral, and the patient gives no history of trauma to the area of ecchymoses
Differential Diagnosis
Petechiae and ecchymoses in systemic amyloidosis may resemble many causes of purpura or coagulopathy. Lesions around eyes may resemble simple bruising. Amyloidosis waxy plaques of eyelids may resemble syringomas in its early stages; the differential, later, might include histiocytoses, mucinoses, xanthomatoses, necrobiotic xanthogranuloma and cutaneous metastases. Lichen amyloidosis requires differential diagnoses with lichen simplex chronicus and hypertrophic lichen planus. Lichen amyloidosis could be misdiagnosed almost be confused with prurigo nodularis, papular mucinosis, pemphigoid nodularis, epidermolysis bullosa pruriginosa and underlying scleroderma. The differential diagnosis for macular amyloidosis includes lichenification, the so-called atopic dirty neck and notalgia paresthetica. The so-called atopic dirty neck shares with amyloidosis the same rippled pigmented appearance. Differential diagnoses to consider with nodular amyloidosis include cutaneous sarcoidosis, lupus vulgaris and granuloma annulare and primary skin tumours such as basal cell carcinoma, xanthomas, granuloma faciale and skin lymphoma.
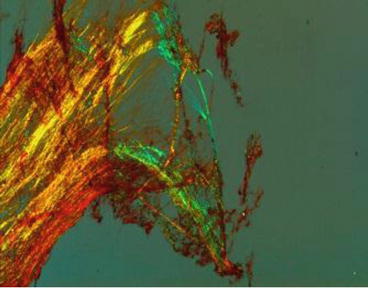
Biopsy
The diagnosis of amyloidosis requires the histological demonstration of amyloid deposits. This is a positive Congo red-stained tissue specimen with the characteristic apple-green birefringence in polarised light. In systemic amyloidosis, abdominal subcutaneous fat aspiration (Fig. 46.3) or biopsy of minor salivary glands is convenient and a non-invasive method that demonstrates amyloid deposits in 70–85 % of patients (Figs. 46.4 and 46.5). The diagnosis of cutaneous localised amyloidosis is based on the presence of amyloid fibrils in skin biopsy. In macular and lichenoid forms, the amyloid deposits are confined to the papillary dermis. Immunohistochemistry stains are negative for cytokeratin, and electron microscopy shows characteristic fibrillar and linear amyloid. In nodular cutaneous amyloidosis, the amyloid deposits are located in the papillary, subpapillary and reticular dermis, with infiltration of the blood vessel wall. Immunohistochemistry stains are negative for cytokeratin and positive for kappa and/or lambda immunoglobulin light chains.