Amputations
CASE PRESENTATION
A 2-year-old child presents for emergent evaluation regarding a finger amputation. He was playing at home 3 hours earlier when his finger was caught in the wheel of an exercise bicycle. There was a traumatic avulsion of the digit but no other injuries. Patient and family were subsequently transported via ambulance to the emergency department for care, accompanied by the amputated part.
CLINICAL QUESTIONS
What are the indications for replantation and revascularization of digits in children?
What is the preferred method of caring for the amputated digit during transport to a medical facility?
What are the important aspects of the history and physical examination of the patient with an amputation?
How soon after injury should replantation and/or revascularization be performed given concerns regarding tissue necrosis?
What are the surgical principles and techniques of replantation and revascularization?
What postoperative measures are taken to maximize viability following replantation and/or revascularization?
What are the anticipated results following replantation?
THE FUNDAMENTALS
Perhaps no surgical procedure better demonstrates the power of reconstructive surgery and requires greater surgical skill than digital replantation. Replantation of amputated parts, by the use of microsurgical techniques, has been performed in children and adolescents for decades; indeed, the first replantation was performed in a 12-year-old boy who sustained a transhumeral-level amputation in a train accident in 1962.1 Reports of successful digital replantation soon followed.2 Following the great advances in microsurgical techniques in the 1970s, similar procedures have been performed throughout the upper extremity in patients of all ages. As technology has advanced and experience grown, so too has our ability to perform tissue replantation in the pediatric hand and upper limb. The fundamental principles and techniques of revascularization and replantation should be familiar to the pediatric hand and upper extremity surgeon.
Clinical Evaluation
The lowest ebb is the turn of the tide.
—Henry Wadsworth Longfellow
While the initial clinical evaluation is often rushed and conducted under stressful circumstances, a few salient points should be covered in every situation. In addition to history regarding hand dominance, functional demands, and pertinent medical conditions and comorbidities, an understanding of the mechanism of injury is critical. Clean, sharp, guillotine-like amputations have a much more favorable prognosis than contaminated, crush and/or avulsion injuries, and as much information as possible should be gleaned regarding the injury mechanism.3
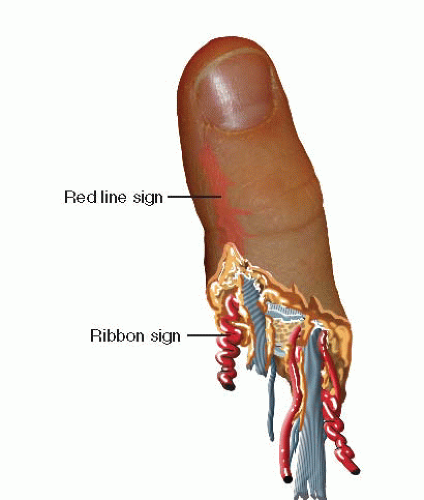
Physical examination should characterize the level of tissue loss, degree of wound contamination, and associated soft tissue injury (Figure 36-1). The “red-line sign,” for example, refers to the hematoma formation along the digital neurovascular sheath and is seen in cases of crush and avulsion injuries, connoting a more extensive zone of vascular injury and poorer prognosis (Figure 36-2). Similarly, the “ribbon sign” may be seen on the amputated part, signifying extensive injury and the need for more complex reconstructive techniques.4 Further examination of the limb proximal to the zone of amputation should be performed to assess for upstream or segmental proximal injuries. If there is excessive arterial bleeding from the wound, simple compressive bandages should be applied. Vascular clamps and electrocautery should not be used in the emergency department, for fear of imparting greater vascular injury. A tetanus booster and prophylactic antibiotics are administered at the time of initial evaluation.
Radiographs should be obtained of the affected hand and upper limb, in addition to all available amputated part(s). Assessment of the skeletal injuries will allow for proper preoperative planning and provide further information regarding the zone and energy of injury.
The proper care of the amputated part during transport and prior to replantation is well established. The amputated digit should be wrapped in moist, salinesoaked gauze and placed in a plastic bag. The entire bag is then placed in a container on an ice bath and transported with the patient.5, 6 and 7 Every effort should be made to save all identifiable parts, as “spare parts” may be used orthotopically during surgical reconstruction. In general, for digital amputations, up to 12 hours of warm ischemia and 24 hours of cold ischemia can be accepted prior to replantation.7 For more proximal amputation—in which there is more muscle tissue—6 hours of warm and 12 hours of cold ischemia are considered acceptable for successful replantation.
Surgical Indications
General indications for replantation in adults include thumb amputations, multiple-digit amputations, amputations through the wrist or proximal, as well as single-digit amputations distal to the flexor digitorum superficialis (FDS) insertion.8 However, replantation of any amputated part is almost always attempted in a child.
Contraindications to replantation include severely crushed, mangled, or contaminated parts, particularly with segmental injury; amputations in patients with significant medical comorbidities or inability to comply with postoperative restrictions and rehabilitation; and amputations with excessive warm ischemia time.
While these indications are generally well accepted, it is imperative that a frank discussion be had with the patient and/or family regarding the surgical options, treatment priorities, and expected outcomes. Successful replantation, defined as tissue viability, does not always equate with full functional restoration. Furthermore, each patient and family is accompanied by their own set of personal and cultural biases; reconciling the hopes and desires of the family with the realistic expectations of surgical treatment is an important ongoing process that begins at the time of presentation.9
SURGICAL PROCEDURES
Great things are done when men and mountains meet.
—William Blake
The treatment principles for the management of digital or upper limb amputations are intuitive. Generally speaking, attention to the amputated part should not detract from care of the overall patient, particularly in multitrauma or more involved injuries. Life comes before limb, and every effort is made to avoid infection, particularly in the severely traumatized extremity. Replantation procedures should not burn bridges to future reconstructive efforts, and heroic, complex operations should not be performed for patients or families unwilling or unable to participate in the postoperative recovery.
Surgically, replantation proceeds through a sequence of established steps: (1) identification of vessels and nerves, which may be tagged with marking sutures for later repair;
(2) thorough irrigation and debridement; (3) skeletal fixation with judicious bony shortening; (4) extensor tendon repair; (5) flexor tendon repair; (6) arterial anastomosis with or without interpositional vein grafting; (7) nerve repair; (8) venous anastomosis with or without interpositional grafting; and (9) loose skin closure. While there are variations in technique, and each patient presents different challenges, the fundamental steps are the same.
(2) thorough irrigation and debridement; (3) skeletal fixation with judicious bony shortening; (4) extensor tendon repair; (5) flexor tendon repair; (6) arterial anastomosis with or without interpositional vein grafting; (7) nerve repair; (8) venous anastomosis with or without interpositional grafting; and (9) loose skin closure. While there are variations in technique, and each patient presents different challenges, the fundamental steps are the same.
♦ Replant of Sharp Amputation with Direct Repair
Sharp traumatic amputation represents one of the most favorable situations for digital replantation.10, 11, 12, 13 and 14 Surgery begins even prior to the patient entering the operating room. Whenever possible, the amputated part is transported to the operating theater while the patient is being evaluated in the emergency department. The part is first cleaned with chlorhexidine, betadine, and/or sterile saline solution, and all foreign material is debrided. Under loupe and microscopic visualization, midaxial incisions are created radially and ulnarly (Figure 36-3). Skin flaps are carefully raised. Volarly, each digital artery and nerve is atraumatically identified and circumferentially dissected using microsurgical instruments. Vessel clamps or fine sutures (our preference is to use a blue 6-0 polypropylene suture [Prolene, Ethicon, Inc., Somerville, NJ]) may be used to tag the very ends of the vessels and nerves for later identification. The distal flexor tendon may similarly be identified and a core suture placed for subsequent tenorrhaphy. Dorsal dissection is more delicate, particularly, as the veins of the avascular segment are collapsed and prone to further injury. The dorsal skin flap is raised, and the plane of dissection is performed between the subdermal and deep fatty layers, where the dorsal veins are identified. These may be similarly clipped or tagged for later use. The extensor tendon stump is also identified, and sutures may be placed. Direction is then turned to the bone. With the use of a microsagittal saw or sharp bone cutter, judicious shortening of a few millimeters is performed, with care taken not to crush the phalanx or injure the adjacent soft tissues.15,16 Smooth K-wires are then placed in a retrograde fashion (longitudinally or obliquely) in preparation for subsequent fixation to the hand. While plates and screws or interosseous wiring may also be used and have mechanical strength advantages, we find that K-wires are simple, faster, efficacious, and do not add bulk or tension to the surrounding soft tissues.16, 17, 18, 19, 20, 21 and 22 Once the soft tissue preparation, bony shortening, and skeletal fixation have been performed, the amputated part is placed in moist gauze on sterile ice to maintain cold ischemia until ready for replantation.
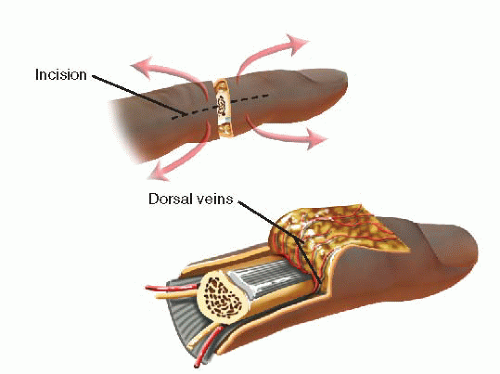 FIGURE 36-3 Midaxial incisions utilized for preparation and exposure of the vessels, nerves, tendons, and bone during replantation. |
The patient is simultaneously brought to the operating room and anesthetized. Adequate intravenous access is obtained, a urinary catheter placed, and the ipsilateral upper extremity prepped and draped into the surgical field. In cases of proximal replantation or extensive zones of injury, the ipsilateral lower limb is also prepped and draped into the field in the event that vein graft from the leg needs to be harvested.
The amputation site is similarly exposed using midaxial incisions. The digital arteries, nerves, veins, and flexor and extensor tendons are identified and mobilized. Core sutures may again be placed in the flexor tendon to facilitate repair later and prevent recurrent retraction into the more proximal tendon sheath or palm. Thorough irrigation and debridement is performed, removing all nonviable tissue and foreign material. Skeletal shortening of the proximal bone may be performed in a fashion that will appropriately engage the amputated part; in general, transverse shortening is the easiest and most reliably performed.
Bony fixation is then performed, reapproximating the amputated part to the prepared recipient site. The previously placed K-wires are passed into the more proximal bone, and longitudinal alignment and rotational position secured (Figure 36-4). Flexor and extensor tenorrhaphies are then performed in the standard fashion23




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree