Chapter 150 Allograft Prosthetic Composite Reconstruction of the Knee
The goal of surgical management of musculoskeletal tumors about the knee is to obtain wide surgical margins and if possible preserve a functional mobile knee. In most cases, satisfactory results are obtained.33 Reconstruction options for attaining a mobile knee include use of an osteoarticular allograft, an oncology prosthesis, or an allograft prosthetic composite; the latter two approaches are used most commonly.41,42 Each method of reconstruction has its advantages and disadvantages. The specific option that is chosen should be based on a multitude of factors, because one method is not necessarily better than another.
An osteoarticular allograft has the advantage of offering a biologic solution to the problem; in the absence of complications, results can be good.1–3 The disadvantages though can be considerable. Fixation problems, nonunion, delayed weight bearing, fracture, graft dissolution, ligamentous instability, degenerative arthritis, extensor weakness, and disease transmission are only some of the problems associated with this method of reconstruction.4,11,36,38
Reconstruction with an endoprosthesis has the advantage of being predictable. These implants are modular, easily available, and easily implanted, and they deal with bone loss very well.16,17 Fixation is often immediate, weight bearing can be started early, stability is built in,28 and disease transmission is eliminated. Two main concerns have arisen, however. The first involves the issue of soft tissue attachment, namely, the extensor mechanism and the difficulty of obtaining secure, functional fixation. This usually results in an extensor lag. Current metallic prostheses do not provide an attachment surface that has an environment for stable, functional soft tissue ingrowth, because they are nonbiologic constructs with metal coatings that are being utilized. Research into this problem is currently under way using foam metals that provide a much more predictable surface for soft tissue attachment. Tantalum and foamy titanium are looking like promising materials for this purpose. However, attempts at assuring soft tissue attachment to metal so far have not been clinically successful. Efforts to reconstitute the extensor mechanism have included securing the native tendon to transposed gastrocnemius fascia, or into the fibula. Incorporation and maintaining appropriate tension are difficult to achieve and are often inconsistent. Thus the quadriceps pull is weak in extension of the knee. This is reflected in the persistent degree of extensor lag often found in this patient group. The other major issue involves the long-term durability of the device itself, as these are often implanted in a young patient population.45 This is further compounded by the long lever arms present at the points of weakness of these devices as a result of the large defects they must bridge.27,28,49
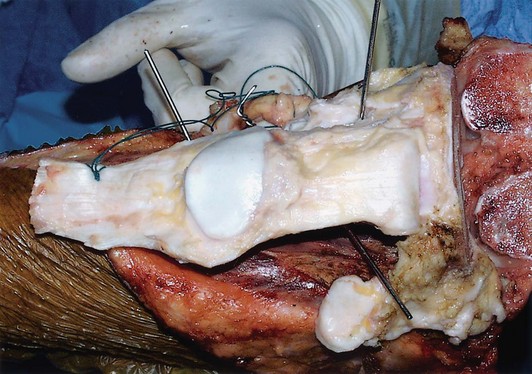
Allograft prosthetic reconstruction of the proximal tibia combines the benefits of osteoarticular allografts (soft tissue extensor reconstruction) with all of the advantages of prosthetic replacement; thus reconstruction of all or parts of the extensor mechanism from the quadriceps tendon to the tibial tubercle is possible by taking advantage of the secure allograft patellar tendon insertion22 (Fig. 150-1). The combination of bulk allograft and metallic prosthesis provides a biologic construct to which tendons and ligaments can be attached and into which they can incorporate over time. Long-term durability remains an issue, but many of the major disadvantages of osteoarticular allografts are diminished or eliminated with the addition of a prosthesis. It must be acknowledged that with allograft prosthetic reconstruction, the cost, the supplies needed and the operating room/anesthesia time can be greater, as the procedure is technically more demanding and therefore has a potentially higher complication rate.20,40,43,47 Allograft prosthetic reconstruction was first undertaken and continues to be performed in the belief that these risks are outweighed by the benefits of a more biologic reconstruction that leads to a better functioning limb, as the extensor mechanism is anatomically reconstructed. Distal femoral allograft prosthetic composites on the other hand offer little if any advantage over endoprosthetic replacement.9,10,31 In general, any time a bulk allograft is used, concerns include nonunion, dissolution, infection, fracture, disease transmission, and risk for postoperative wound complications.5,12,37,39,43 In addition, if anything less than a fully constrained device is used, instability of the knee can be an issue.
Our experience with allograft prosthetic composite (APC) over endoprosthetic reconstruction of the proximal tibia has supported superior performance of the APC with regard to extensor mechanism strength and subsequent function. Gilbert and associates demonstrated consistently good functional results with an acceptably low complication rate.21 Donati and colleagues reported on a large series of 62 patients at the Rizzoli Institute and noted a Musculoskeletal Tumor Society score of satisfactory in 90.4% of patients with a 5-year survival rate of 73.4%. Their reported survival rates were comparable with those of reconstruction with a modular prosthesis. Because of a high infection rate, not seen in other series, the authors advised not using this technique for patients receiving chemotherapy.15 What has never been objectively determined is whether there is a clinically relevant difference between these two reconstructive options with respect to validated outcome scores and biomechanical function as determined by gait analysis.6,40,47 The few studies published to date have looked at long-term survival of the reconstruction choice primarily, and not at the functional difference between surviving reconstructive options. Most of these studies look at and compare outcome scores only, with no formal analysis of dynamic function.6,47
Basic Principles of Allograft Prosthetic Reconstruction
One of the major complications of using allografts is graft fracture. This problem is aggravated by graft dissolution. One of the advantages of using a prosthesis with an allograft is that the prosthesis can reconstruct the joint surface and can also provide graft fixation while maintaining the strength of the allograft. This is why it is important to span the entire length of the graft and extend into the host bone. Fixation by any means should not stop within the substance of the allograft.23,24
We believe a press-fit stem is ideal; unfortunately for tumor reconstruction, many patients receive chemotherapy that has a detrimental effect on bone ingrowth.14,25,26 In addition, no good press-fit options for the tibia are available. Cementing the composite may be a better choice if certain conditions can be met. The major problem with cement in an APC reconstruction involves the cement technique itself. The usual method described is cementation in two steps: first, cementing the prosthesis to the graft, and second, cementing the composite to the host bone. This results in a poor cement technique in both instances. When the prosthesis is cemented to the allograft, it is difficult to contain the cement within the graft and keep it from running out both ends of the graft. When cementing into the host bone, it is difficult to keep the cement out of the graft-host junction, contributing to problems with healing. If cement is chosen as the method of fixation, we cement the stem into the allograft and the host at the same time with standard third-generation techniques. When the cemented stem is inserted into the host bone, the stem must not have any influence on the graft-host junction relationship; therefore rigid provisional fixation must be used to hold the graft and the host bone together, so they can be prepared and cemented in a single step.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree