Allograft Prosthetic Composite and Endoprosthetic Replacement of the Proximal Femur
Krista A. Goulding
Mark Spangehl
Chris Beauchamp
INTRODUCTION
Reconstruction of the proximal femur after tumor resection or in instances of failed arthroplasty remains a significant challenge, despite advances in surgical technique and prosthetic design. Depending on the pathology, a number of reconstructive techniques are in use, the most common being allograft prosthetic composite (APC) and endoprosthetic replacement (EPR) (1,2,3,4,5,6,7,8,9,10,11,12). In addition to sarcomatous lesions and failed hip arthroplasty with uncontained, circumferential, segmental bone loss (13), indications for an APC or segmental arthroplasty include metastatic disease and failed internal fixation of hip fractures. Culprits in the development of this magnitude of bone loss can include infection, aseptic loosening, or nonunion of fracture with implant cutout, among others.
INDICATIONS: WHEN TO CHOOSE EPR VERSUS APC?
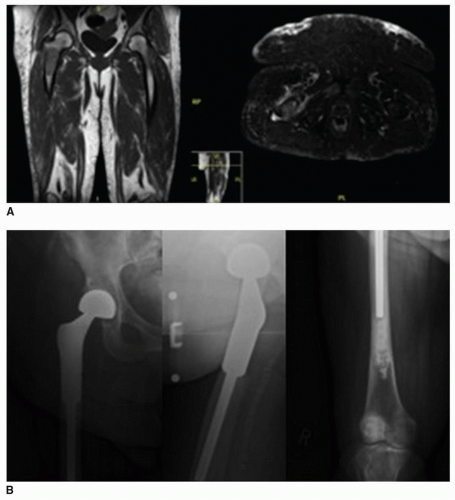
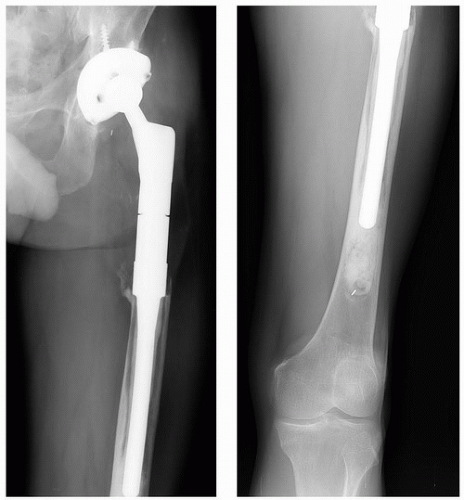
It is important to consider the goals of surgery when contemplating an APC or endoprosthetic reconstruction. In a patient with bony malignancy and a short anticipated survival, full weight bearing and immediate mobilization are paramount to relieving pain and ensuring quality of life (1). As a result, endoprosthetic reconstruction is most commonly favored in older patients with metastatic disease (Fig. 29-1). Patients at significant risk of problems with bone healing, those requiring radiotherapy or a prolonged course of chemotherapy, as well as individuals in whom the abductor mechanism cannot be reconstructed are also best managed with an EPR (Table 29-1). That segmental
endoprostheses are readily available, are modular, and carry less risk of infection contribute to their widespread use (13). Disadvantages of this mode of reconstruction include a 10% rate of aseptic loosening (1,9,10,11,14) (Fig. 29-2), trochanteric escape (Fig. 29-3), and dislocation, which has been reported in up to 28% in some studies (1,9,10,13,15). Revision surgery requiring complete implant removal may also be more difficult if a long, cemented stem is used.
endoprostheses are readily available, are modular, and carry less risk of infection contribute to their widespread use (13). Disadvantages of this mode of reconstruction include a 10% rate of aseptic loosening (1,9,10,11,14) (Fig. 29-2), trochanteric escape (Fig. 29-3), and dislocation, which has been reported in up to 28% in some studies (1,9,10,13,15). Revision surgery requiring complete implant removal may also be more difficult if a long, cemented stem is used.
TABLE 29-1 Ideal Patient Selection for an Allograft Prosthetic Composite or an Endoprosthetic Reconstruction | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
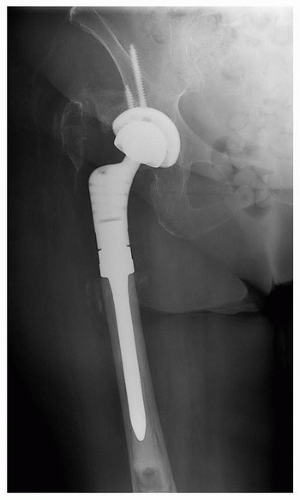 FIGURE 29-3 Plain radiograph of a cemented proximal femoral endoprosthetic reconstruction showing trochanteric escape with significant proximal migration of the fragment. |
Implant durability and restoration of function, although always desirable, becomes much more critical in patients with long anticipated survival (1,13). Consequently, the arthroplasty patients or a young individual with good prognostic factors who is expected to survive a sarcoma represent potential candidates for an APC. This construct has the advantage of restoring bone stock, providing an anchor to which the abductors can be attached, and facilitating further revision surgery due to the shorter and uncemented nature of the prosthesis within the host proximal femur (1,13,15). Disadvantages primarily include the risk of infection, which can be as high as 20%, and nonunion at the host-graft junction in 10% of cases (4,5,6,12,13,15,16). The possibility of disease transmission (HIV, hepatitis, other viral disease), albeit rare, is also a consideration in recommending this surgical modality (13,15). Abductor dysfunction and graft resorption are significant concerns as are fractures, occurring in up to 60% of patients (13,15,16,17).
PREOPERATIVE PLANNING
In the setting of a known or suspected neoplasm, the appropriate oncologic workup should be carried out, including imaging, blood work, biopsy, and tumor staging. Magnetic resonance imaging of the tumor should cover the entire lesion, and ideally, span the length of the entire bone involved to identify any skip metastases. The site of the femoral osteotomy should be planned out with a minimum distance of 2 cm from the most distal aspect of the lesion. Computed tomography (CT) of the chest, abdomen, and pelvis should be obtained, in addition to other nuclear medicine scans where appropriate. If the lesion is not known to be metastatic in nature, the case should be discussed in a multidisciplinary tumor board meeting, and neo- or adjuvant therapy organized with medical or radiation oncologists where needed.
Cases of failed arthroplasty should be worked up for infection. Inflammatory markers, such as ESR and CRP, should be ordered and joint aspiration carried out under sterile technique with ultrasound or CT guidance. Samples should be sent for a cell count, aerobic and anaerobic cultures, as well as mycobacterium and acid-fast bacilli. In our institution, aspirates are also sent for a synovial fluid CRP and alpha-defensin test (18,19,20), which together show promise in diagnosing periprosthetic joint infection with a sensitivity of 97% and a specificity of 100% (18). If the patient is indeed infected, a two-stage exchange, with placement of an antibiotic-impregnated spacer and a prolonged course of intravenous antibiotics in consultation with colleagues with expertise in infectious disease, should precede reconstruction.
Medical and nutritional optimization should be prioritized in order to reduce the risk of medical complications and afford the best chance of achieving bony union. Smoking is a relative contraindication to an APC. Informed consent should be obtained after an in-depth discussion of the risks and benefits of surgery.
ALLOGRAFT SELECTION
To select the size of implant or allograft, full-length radiographs of the femur and an anteroposterior radiograph of the pelvis should be obtained. Leg lengths should also be assessed clinically and radiographically for discrepancy, and any deformity of the distal portion of the femur should be noted. A CT scan can be helpful in measuring the size of the host bone canal at the level of the planned resection. Plain radiographs of the allograft are mandatory to identify that the correct bone has been ordered and to measure the width of the canal (Fig. 29-4). The intramedullary canal of the allograft should be slightly larger than that of the distal host bone, in order to facilitate cementing the prosthesis into the allograft while maintaining press-fit fixation in the host bone (Table 29-2). Measuring the host canal size is crucial because a fully porous-coated, distal fixation stem (Fig. 29-5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree