FIGURE 28-1. A: Radiograph of patient with markedly deficient proximal femur and failed femoral component. B,C: Radiograph after reconstruction with proximal femoral allograft.

FIGURE 28-2. A: Radiograph of patient with markedly deficient proximal femur and failed femoral component. B,C: Radiographs after reconstruction with proximal femoral allograft.
Many different methods of joining an allograft to the proximal femur have been described. Each has its own advantages and disadvantages: some require more carpentry than others; some provide more immediate stability between allograft and host bone than others; and some are best suited to circumstances in which the allograft and host bone diameter are well matched, while others are best for cases of markedly discrepant allograft–host bone diameters.
End-to-End Allograft to Host Bone Junction Several different methods of end-to-end allograft to host bone junction joinery have been described including a simple tranverse butt joint, a step-cut joint (Fig. 28-3), and an oblique joint.8–12 Most surgeons now prefer a step-cut because it provides the most rotational stability and also provides a greater surface area for bone healing (Figs. 28-4 and 28-5). The drawback of this method of reconstruction is the need for complex carpentry to gain a perfect fit of the allograft to host bone.
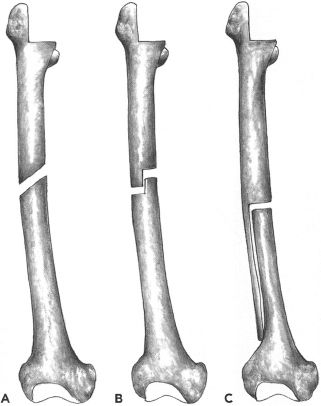
FIGURE 28-3. A: Transverse butt joint between allograft and host bone. B: Step-cut joint between allograft and host bone. C: Oblique joint between allograft and host bone.

FIGURE 28-4. A: Radiograph of patient with deficient proximal bone due to osteolysis. B: Radiographs after reconstruction with a proximal femoral allograft using step-cut joint between allograft and host bone.

FIGURE 28-5. Intraoperative picture of allograft prosthetic composite with step-cut graft–host bone junction. Note the excellent bone apposition.
Technique Careful preoperative planning is essential for a successful allograft prosthetic composite reconstruction. Preoperative radiographs (with markers to calibrate magnification) of the whole host femur are obtained to assess femoral bone loss, femoral geometry, and femoral size. Radiographs of potential bone allografts also are obtained. In most cases, a proximal femoral allograft is appropriate; however, occasionally, a whole femoral allograft is necessary. A donor tibial allograft may be used instead of a femoral allograft in selected cases. The outside diameter of the allograft should be similar to the outside diameter of the host bone. Femoral allografts often come from younger donors with smaller diameter femurs; thus, careful scrutiny of the diameter of potential allografts is necessary. It is important to choose an allograft of sufficient diameter to allow placement (after preparation) of a satisfactorily sized implant to provide stability across the allograft-host junction site.
The hip may be exposed through an anterolateral approach or a trochanteric slide. Alternatively, if the proximal bone and trochanter are absent, the abductors and vastus lateralis may be split in line with their fibers in the midcoronal plane to provide a direct lateral approach to the hip. A posterior approach also may be used, but it disrupts the posterior soft tissue sleeve and may increase the already high risk of dislocation.
The failed prosthesis is removed, and all cement and membrane are removed from the femoral canal. The distal femoral canal is prepared according to the planned distal diameter of the prosthesis. If the prosthesis will be press-fitted into the host bone, then the femur is reamed to the appropriate diameter. Based on the type of planned reconstruction, the proximal femoral allograft is provisionally prepared. If the implant will be cemented into the allograft—as is almost always the case—then the proximal femoral allograft is prepared with broaches and, if desired, reamers. The host bone then is contoured to the shape planned for the junction between the allograft and the host bone, which mostly commonly will be a step-cut. The portion of bone removed to form the step-cut and the length of the step-cut removed depends on the geometry of the bone defect. The step-cut may be oriented with the long host bone side medially or laterally depending on the bone defects present. Next the allograft is provisionally marked for the step-cut (or for the proposed geometry of the graft host bone joint). It is important to mark the allograft carefully if a step-cut is being used, to demonstrate which side of the step-cut will be retained and which side will be removed. Also, the allograft should be marked to provide for greater than the expected required length and circumference of the allograft; more always can be trimmed later after provisional trialing. Once the provisional cut has been made, a trial prosthesis is placed inside the allograft and host femur, and hip reduction is attempted. The length of the allograft is adjusted sequentially to provide the proper length/tension relationship. The allograft is further trimmed to optimize apposition of the allograft–host bone junction, a process that typically requires several iterations. The real prosthesis is cemented into the allograft in appropriate anteversion based on the position of the step-cut. The optimal anteversion should be marked carefully on the allograft before the implant is cemented in place. If a fully porous-coated or similar prosthesis will be press-fit into the host femur, a plastic “Steri-Drape” may be wrapped around the distal prosthesis before it is inserted through the cement to the allograft. The nonsticky portion of the Steri-Drape is wrapped around the prosthesis followed by the sticky portion of the Steri-Drape, providing a sheath for the prosthesis and preventing cement from bonding to the distal stem during the cementation process. Any extra cement is carefully removed as the cement cures.
After the cement has cured, the allograft prosthetic composite is prepared for insertion into the host bone. If a Steri-Drape has been used to protect the distal prosthesis, it is removed at this time. A prophylactic cerclage cable or wire typically is placed around the femur just distal to the allograft prosthetic composite junction if an implant will be press-fitted into the host femur. The distal aspect of the implant then is inserted into the host bone and impacted until the allograft–host bone junction is well-opposed. If the implant is being cemented into the host bone, a cement restrictor is placed in the femur at an appropriate depth. In this case, cement is inserted into the host femur with a cement gun and pressurized, and then the implant is inserted into the cement. It is important to remove all cement possible from the allograft–host bone junction.
After the prosthesis has been inserted and is stable, the allograft–host bone junction is further secured with cables (usually two) (Fig. 28-5). If autogenous host bone is available, it is packed along the allograft–host bone junction. Strut allografts also can be used to enhance the stability of this junction, but primary stability without strut grafts is preferable, because strut graft healing to allograft is unpredictable. If proximal host bone femur fragments are present and have been kept vascular, they may be wrapped around the allograft–host bone junction.
If host greater trochanter is present, the medial surface of the host trochanteric fragment is freshened. The outer cortex of the allograft greater trochanter is removed with a saw, and the trochanter is fixed with wires or suture. Cables are less desirable in these cases because the healing rate at this junction is only about 75%, and if healing does not occur, cable fretting debris may be problematic.
Abductors usually are not sewn to the allograft as this may induce revascularization and re-sorption of the allograft. If possible, the abductor–vastus lateralis sleeve is reapproximated to itself from anterior to posterior over the allograft. Deep drains are placed and the fascia is closed carefully to protect the allograft.
Postoperatively touch weight bearing is recommended until radiographic evidence of allograft–host bone junction healing is visible radiographically, a process that typically takes 3 to 5 months, but can take longer. If union is markedly delayed, autogenous bone grafting may be considered. In most cases a prophylactic hip guide brace for 2 to 3 months postoperatively is used to reduce the risk of early dislocation.
INTUSSUSCEPTION TECHNIQUE
The allograft intussusception technique may be used in special circum-stances when the proximal host femur is absent and the remaining femoral canal is wide and patulous (Fig. 28-6). Alternative treatment methods in these circumstances include cementing a tumor prosthesis into the femur—which may have a high loosening rate if the femur is multiply revised and the canal is sclerotic—or reconstruction with a very-large–diameter uncemented extensively porous-coated or fluted tapered stem.
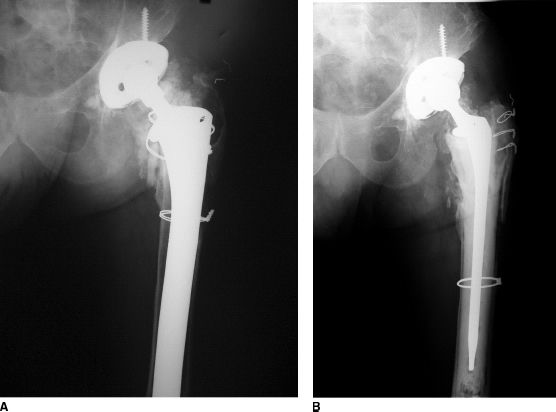
FIGURE 28-6. A: Radiograph of patient’s hip with markedly deficient proximal femoral bone, wide femoral canal, and loose femoral component. B: Radiographs after reconstruction with intussusception allograft prosthetic composite.
This allograft intussusception technique is predicated on the idea that a femoral allograft can be milled until it fits inside a large-diameter host femur. The allograft then is impacted into the femur to achieve a pressfit similar to that obtained by an uncemented implant. The large surface area of the allograft against host bone facilitates healing. The new femoral canal provided by the allograft provides a good interface for cemented prosthesis fixation. This technique is most valuable in patients with severe segmental proximal femoral bone loss in association with a markedly widened femoral canal.
Technique Preoperatively, the surgeon chooses an optimal femoral allograft based on preoperative templating (using radiographs of the allograft) compared to radiographs of the failed hip replacement. Differing magnifications of the two films are taken into account. The surgeon must decide whether the allograft will be inserted with the proximal end of the allograft femur nearest to the hip joint or the distal end of the allograft femur nearest to the hip joint (i.e., with the allograft “right side up” or “upside down”). The narrowest diameter of the allograft femur is proximal to the midpoint of the femur; hence, a longer allograft can be obtained (when needed) by inverting the allograft.
The hip joint is exposed by splitting the iliotibial band and then the gluteus medius in the coronal plane in the direction of their respective fibers. If a greater trochanteric fragment remains, it may be reflected anteriorly as a trochanteric slide or split in half longitudinally in the coronal plane. Exposure of the remaining femur is gained by splitting the vastus lateralis longitudinally. The failed femoral component and remaining cement within the femoral canal are removed. The canal is reamed with either flexible reamers or straight-tapered reamers until the host bone has been freshened. Sometimes the canal is too large to accommodate any reamers, in which case the canal is freshened with back-biting instruments from the cement removal set.
The femoral allograft (usually a whole femur) is brought onto the field. The surgeon should strive to engage a substantial length of the allograft inside the host femur. The femoral allograft is osteotomized at an appropriate level, usually near the narrowest diameter of the graft. Next the external dimensions of the allograft are shaped with a high-speed cutting burr. A barrel-shaped burr works particularly well for this purpose, and the femur is shaped in a manner similar to peeling a carrot, sequentially trimming the allograft to fit the internal shape and dimensions of the femur. The allograft femur is milled to a gently tapered shape, and care is taken not to overprepare the allograft, because a firm pressfit into the host femur is necessary for success. The allograft is shaped and tested in the host bone in an iterative manner until the graft is properly sized. An excellent friction fit between the host bone and the allograft typically is achieved, provided sizing is correct. Next the femoral allograft is prepared provisionally for a long-stem cemented femoral component of the surgeon’s choice using reamers and broaches.
A prophylactic cable is placed around the host femur and tightened provisionally. The allograft is oriented appropriately rotationally, and then it is gently and gradually impacted into the femur. To match the bow of the femur, often it is necessary to start impacting the graft in extra “anteversion,” and to derotate the graft gradually into proper anteversion as it is impacted deeper into the femur. As the graft is impacted, the prophylactic cable is tightened. An excellent press-fit of the allograft must be achieved, and the allograft must be both axially and rotationally stable at the completion of this process (Fig. 28-7).
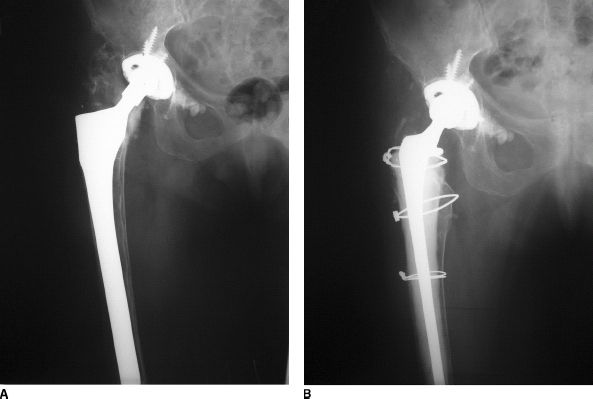
FIGURE 28-7. A: Radiograph of pa-tient’s hip with markedly deficient proximal femoral bone, wide femoral canal, and loose femoral component. B: Radiographs after reconstruction with allograft prosthetic composite.
An important aspect of sizing the allograft is judging where the allograft will seat in the femur to provide appropriate length restoration of the limb. Impacting the allograft into the femur before cementing the implant into the allograft allows the surgeon to adjust soft tissue tension and leg length by modifying the proximal allograft (by trimming) or prosthesis length (by using a calcar buildup) after an optimal pressfit is obtained and the final allograft seating level is determined. Once the allograft is fully seated in the femur, a trial cemented implant is placed in the allograft, and the final allograft neck osteotomy is performed at the optimal level.
The author prefers to use a femoral component length that protects most of the allograft but that does not extend into the host femur beyond the allograft (unless necessary for stability of the construct). A cement restrictor is placed in the femoral canal. Using standard techniques, cement is introduced into the allograft with a cement gun and pressurized, and a cemented stem is inserted in proper anteversion (Fig. 28-8).
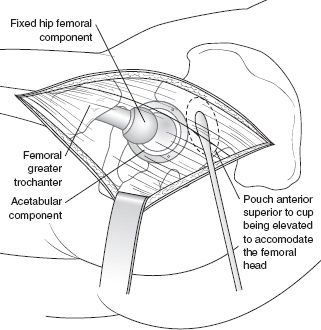
FIGURE 28-8. Diagram of the intussusception allograft technique.
If desired, remaining trochanteric remnants can be reapproximated to the allograft. Other remaining large host bone fragments with muscular attachments are reapproximated to the allograft with cerclage. Available host or allograft cancellous bone is packed around the allograft–host bone junction site to promote healing. Closure is performed in the standard manner, making an effort to close in layers to protect the allograft.
Postoperatively, the patient usually receives a hip guide brace to reduce early dislocation risk. Weight bearing is limited to touch weight bearing for approximately 12 weeks, to give the graft time to heal to host bone. Subsequently, the patient may commence partial weight bearing and may progress weight bearing gradually over the following 2 months, so that by 4 to 5 months the patient is allowed full weight bearing. Healing of the allograft to host bone typically can be identified radiographically by 3 to 6 months after operation.
RESULTS
Short- and midterm results of allograft prosthetic composite reconstruction of failed total hip arthroplasty with marked bone loss have been reported by a number of authors.13–15 These reports consistently document this is an efficacious technique to reconstruct massive proximal femoral bone loss. As expected, clinical results and hip scores typically are less good than those reported for simpler revisions because these patients often have had several revision arthroplasties before and also have deficient abductors or abductor attachments. Complication rates (see below) also tend to be higher due to the complex nature of the procedures.
Longer term results of this reconstruction method have been reported by several authors in large numbers of patients. Blackley et al.16 reported the Toronto experience of 63 revisions with allograft prosthetic composites at 9 to 15 years (mean 11 years) after operation. Five hips failed due to infection, and three due to aseptic loosening. Two hips required reoperation for hip instability and three for problems with allograft–host bone junction site healing. The mean Harris Hip Score increased from 30 points preoperatively to 71 points postoperatively. Defining success as a Harris Hip Score increase of at least 20 points, a stable implant, and no additional surgery related to the allograft, the authors reported success in 78% of hips reconstructed in this manner. Haddad et al.17 reported the Vancouver experience with 55 proximal femoral allograft prosthetic composites followed a mean of 8.8 years (range, 3 to 12.5 years). They found six failures directly related to the allograft prosthetic composite: three graft-host nonunions, two infections, and one allograft fracture. The mean Harris Hip Score increased from 39 to 79 points. Allograft resorption was seen radiographically in seven patients, but had not led to clinical failure in any case. Finally, Wang and Wang18 reported a more cautionary experience in 15 patients followed a mean of 7.6 years after allograft prosthetic composite reconstruction for a total hip arthroplasty revision: ten patients (67%) had an intact construct at last follow-up.
Allograft prosthetic composites have been reported to provide satisfactory results when used for specific indications. Alexeeff et al.19 reported good results in 11 patients revised with a two-stage procedure for infection. No patients failed due to recurrent infection. Other authors have reported success in using allograft prosthetic composites in the reconstruction of comminuted periprosthetic femur fractures around total hip arthroplasty.
COMPLICATIONS
Allograft prosthetic composites are at elevated risk for several specific complications.20 Hip dislocation is more common with allograft prosthetic composites than routine hip reconstructions because abductor attachments often are deficient. Reported dislocation rates range from 11% to 16% in larger series (Table 28.1). When severe abductor deficiency is present, a constrained liner or nonconstrained tripolar construct may be used at the time of allograft reconstruction. At a minimum, a large-diameter femoral head should be used—when possible—to enhance stability. Allograft prosthetic composite patients are at increased risk for infection because of the involved nature of the reconstruction, long operating time, and the use of avascular bone. The infection rate is reported from 4% to 20% in different series (Table 28.1). Consequently, antibiotic impregnated cement is reasonable to use for the cemented portion of these reconstructions, and perioperative intravenous perioperative prophylactic antibiotics are essential in these patients, as in other revision patients.
TABLE 28.1 Complications of Allograft Prosthetic Composite Reconstruction
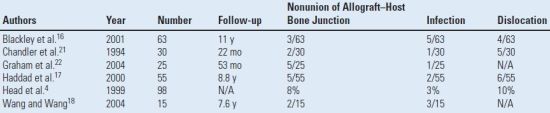
N/A, not available.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








