Meniscal preservation is essential for maintaining articular cartilage homeostasis, joint congruence, stability, and proprioception (
1). In younger and more active patients, meniscal repair remains the preferred method of treatment for unstable meniscal tears and may play an important role in optimizing knee function (
2,
3) and delaying the progression of degenerative disease. Owing to the important physiologic role that meniscal tissue plays in the knee, meniscal repair is advocated in young athletically active patients (
4). The indications for repair may be heightened in those patients who present with meniscal tears and associated concomitant pathology such as anterior cruciate ligament tears or those requiring articular cartilage resurfacing or axial realignment osteotomies (
5). Furthermore, as our knowledge and understanding of meniscal pathophysiology, healing, biomechanics, and minimally invasive repair improve, indications for repair are likely to expand. All-inside arthroscopic methods using novel suture-based devices represent a potentially effective and minimally invasive approach to meniscal repair. Adjuvant biologic therapies, such as platelet-rich plasma also appears promising and may increase the potential of repairing “irreparable meniscal tears” and improve the clinical success of surgically repaired “biologically-at-risk” tears.
CLINICAL EVALUATION
Knee kinematics predicts that internal rotation of the femur on the tibia forces the medial meniscus posteriorly and toward the center of the joint. If a meniscal attachment is abnormally loaded (peripheral or otherwise), as the posterior portion of the meniscus is forced toward the center of the joint, it may be caught between the femur and tibia, and resultant meniscal tearing can occur with further extension of the joint.
Patients with meniscal injuries typically present with clinical symptoms of focal joint line pain, swelling, and discomfort at the extremes of motion as well as specific mechanical symptoms such as catching, locking, and loss of extension. Physical examination should include evaluation and assessment of anatomic and mechanical axial alignment as well as signs of effusion, antalgia, loss of motion, focal joint line point tenderness, joint locking/clicking, and pain with squatting in terminal flexion and with axial compression. Manual examination for meniscal pathology has been reported to have a sensitivity and specificity of 55% to 85% and 29% to 67%, respectively (
6). Provocative maneuvers for meniscal pathology include McMurray’s test, the Apley grind or compression test, the Thessaly test, the Steinmann test, and Childress (squat) test (
6,
7 and
8). McMurray’s test is performed by placing a varus or valgus stress to a flexed knee while extending, and is a reliable examination maneuver for diagnosing meniscal tears. The sensitivity of McMurray’s test has been reported at 16% to 37%, with specificity at 77% to 98%, and a positive predictive value of 83% (
6,
7). Similarly, the Apley grind or compression test, performed by flexing the knee, rotating, and compressing, has been reported to have a sensitivity of 13% to 16%, a specificity of 80% to 90%, and overall accuracy of 28%. The Thessaly test, in which the patient stands flatfooted on the floor and rotates at the knee in 20° of flexion internally and externally, has been reported to have a sensitivity, specificity, and overall accuracy of 89%, 97%, and 94%, respectively for medial meniscus tears and 92%, 96%, 96%, respectively for lateral meniscus tears (
8). The Steinmann test is performed as a flexed knee is internally and externally rotated at the foot, whereas the Childress (squat) test elicits symptoms with the patient fully squatting with feet in internal and external rotation. The Bounce home test is performed with the patient supine by holding the great toe or forefoot and then attempts to identify a sharp endpoint as a fully flexed knee is taken to full extension or even hyperextension. A positive test occurs when full extension is unable to be obtained.
Clinical assessment for meniscal tears should always include plain roentgengrams, which should be evaluated to assess for crystal arthropathy, osteoarthritis, osteonecrosis, osteochondral defects, and calcification. Radiographs
should include extension weight bearing anteroposterior, lateral, notch, and patella skyline views. Weight-bearing 45° flexion posteroanterior comparison views should also obtained to assess a narrowed joint space in cases where articular cartilage wear is suspected. Routine magnetic resonance imaging is often not necessary for diagnosis of meniscal injury but may prove valuable in a more comprehensive evaluation of the knee.
DECISION MAKING—REPAIR VERSUS RESECT
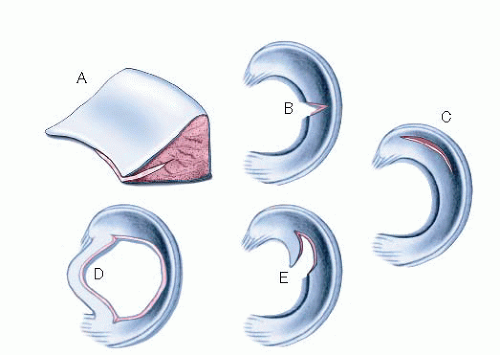
Decision making regarding meniscal repair is dependent upon tear characteristics (i.e., tear pattern, geometry, location, vascularity, size, stability, tissue viability, or quality), associated pathology, previous surgeries, and patient expectations and goals (
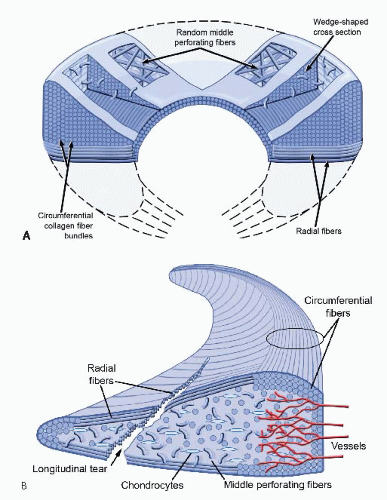
10). Vertical longitudinal tears (77.5% of medial meniscal tears and 59.4% of lateral meniscal tears (
9)) with minimal deformation in the vascularized peripheral meniscus are generally considered anatomically optimal for repair owing to their vascular potential for healing. Deformed or frayed oblique flaps, radial, horizontal cleavage, or degenerative complex tears within the avascular white-white zone have traditionally been treated with resection (
10). Patient age, activity level, and postoperative rehabilitation compliance must also be taken into account before a decision is made regarding repair versus resection (
Table 56.1).
Small, peripheral tears less than 7 mm in length and incomplete tears noted in the posterior horn of the lateral meniscus in a relatively asymptomatic patient (such as a patient undergoing concurrent anterior cruciate ligament reconstruction) can be left alone and be expected to heal. Shelbourne and Heinrich (
11). concluded that posterior horn lateral meniscus tears, stable incomplete radial flap tears, or peripheral or posterior third tears within 1 cm of the popliteus tendon can be treated successfully and left in situ.
In contrast, surgical intervention is indicated in patients with unstable tissue, substantial peripheral longitudinal tears, mechanical symptoms, or when nonoperative measures (modification of activities, inflammation reduction, and physical therapy) fail.
Meniscal excision may alter load transmission, contact stresses, and tibiofemoral patholaxity (particularly in knees with associated anterior cruciate ligament [ACL] deficiency). Posterior root tears of the medial meniscus have been shown to increase peak contact pressure by 25% in the medial compartment and 13% in the lateral compartment than with an intact meniscus (
12). Repair of the tear site returned peak contact pressures to baseline and showed significant improvement in medial compartment contact pressures, tibial external rotation, and lateral tibial translation. In addition, meniscectomy in athletes has been shown to lead to knee instability, radiographic changes, and reduction in functional activities as early as 4.5 years postsurgery (
13). Clinical outcomes following partial meniscectomy reveal that radiographic progression of medial compartment osteoarthritis after medial meniscectomy was greater than lateral compartment osteoarthritis after lateral meniscectomy (
14). Furthermore, when less than 50% of the meniscal rim remains, radiographic progression may be seen.
Fabricant et al. (
15) reported on a level 1 prognostic prospective study of 126 arthroscopic partial meniscectomies evaluating first year postoperative recovery revealed that female gender and extent of chondral pathology affected knee pain, knee function, and overall physical knee status (effusion, flexion, extension, gait, and general progress) significantly. Age, body mass index, depth of meniscal excision (amount of meniscus removed from any zone), involvement of one or both menisci, and extent of meniscal tear (total number of zones involved) showed no association. Extent of the meniscal tear affected overall physical knee status but not knee pain or function. Meniscal excision and involvement of one or both menisci had no impact on recovery. McDermott and Amis (
16) pointed out that negative factors affecting longterm prognosis include the amount of tissue resected, the location of resection (posterior horn worse than anterior
horn or bucket-handle tears), the disruption of retained circumferential fibers, lateral meniscectomy (worse than medial), a preexisting chondral lesion, varus alignment of the affected knee, ACL deficiency or ligamentous patholaxity, and increased postmeniscectomy activity levels. Further support is provided by a retrospective comparative study of medial versus lateral arthroscopic partial meniscectomies suggesting that a more optimal prognosis can be predicted with patients less than age 35, vertical tears, absence of cartilage damage, and an intact meniscal rim following meniscectomy (
17). In addition to the consideration of the natural history of meniscal resection, patient counseling of the procedural risks, benefits, expected recovery and rehabilitation as well as the outcomes of selected treatment options are essential. Recovery time and re-tear risks should also be addressed and may play a role in decision making when an expeditious and more predictable return to work or sport is preferred.
Timing
Controversy remains regarding what the ideal interventional period for isolated meniscal tears is. Tenuta and Arciero (
18) evaluated 51 patients with 54 meniscal repairs with second-look arthroscopy at an average of 11 months after repair. Time to surgery did not effect healing; however, meniscal repairs that did not heal when carried out with ACL reconstruction had a longer time to repair (60 weeks) than those that healed (19 weeks). Henning et al. (
19) reported a significant difference in repair outcomes within 8 weeks of injury to those performed later, although the repairs performed later may have been more complex. Cannon and Vittori (
5) evaluated 90 meniscal repairs, 68 in conjunction with ACL reconstructions. Isolated meniscal tears repaired within 8 weeks were more clinically successful (57%) than those carried out later than 8 weeks (47%). Similarly, those repaired in conjunction with ACL reconstruction had a 96% healing rate within 8 weeks of injury versus 91% for repairs carried out later than 8 weeks postinjury.
Scott et al. (
20) reported on 260 meniscal repairs at an average of 47.3 weeks from initial injury (median 19 weeks). They found no difference in healing rates in patients with a span of more than 3 weeks from injury to surgery to those operated on within 3 weeks of injury. They concluded that chronicity of symptoms did not alter prognosis of healing. Noyes and Barber-Westin (
4) evaluated 30 meniscal repairs in patients 40 years of age or older, 20 chronic, and 10 acute (within 10 weeks of injury), for tears extending into the central one-third of the meniscus or with a rim width of 4 mm or more. Chronicity of the injury also yielded no significant effect on repair. Noyes and Barber-Westin (
21) later evaluated 71 meniscal tears that extended into the avascular region in patients 19 years of age and younger. Average time from injury was 40 weeks (range 1 to 256 weeks). Forty repairs were performed acutely (1 to 12 weeks) and 31 for a chronic condition. No difference was found between success (or failure) of repair and length of time from injury to repair.