CHAPTER 73 Adult Scoliosis
Adult scoliosis encompasses a broad spectrum of deformity in the mature spine. It can result from scoliosis in childhood or arise de novo from degenerative changes within the spinal motion segments. Scoliosis in the adult differs significantly and importantly from scoliosis affecting the child or adolescent. Important differences include curve types and patterns, rate of deformity progression, rigidity of deformity, patient comorbidities, and clinical symptoms and presentation. The differences between the adult and child with scoliosis lead to significant differences in the goals of care and strategies for treatment.1 In the child with scoliosis, the primary goal of care is to avoid the consequences of deformity progression. Adults with scoliosis characteristically present with pain, functional limitations, neural symptoms, and symptomatic deformity resulting in a measurable impairment on health-related quality of life. Improvement of present pain and disability is an important and measurable goal of treatment for adults with scoliosis. The value of care for adults with scoliosis may be measured quantifiably by a change in patient-reported quality of life measures.
Impact of Adult Scoliosis
Adult scoliosis is a common disorder of the spine with a wide variation in reported prevalence. The prevalence of scoliosis in adults has been estimated by population-based studies, and radiographic studies including DEXA scans and radiographic studies on populations that are representative of age-adjusted norms. Reported rates of scoliosis range from 1.4% to 68%.2–5 The source of variability is related to differences in definitions of scoliosis, methods of defining cohorts, sample size, and screening tools. Healey and Lane6 identified curves over 10 degrees in more than 50% of elderly females with back pain and osteoporosis. Robin and colleagues7 identified some degree of scoliosis in 70% of adults in a cohort of 554 patients between ages 50 and 84, with 30% of those having curves greater than 30 degrees. Ten percent of patients with a straight spine at enrollment developed a new onset of scoliosis during the 7- to 13-year follow-up period. More recently, Schwab and colleagues8 identified scoliosis of greater than 10 degrees in 68% of healthy, adult volunteers older than age 60. The prevalence of scoliosis affecting the adult increases with age because of the significant rate of occurrence of de novo cases with aging of the spine.9 There is significant evidence that scoliosis is a common condition with a high prevalence on older populations.
The impact of scoliosis on health-related quality of life has also been reported with significant variability. The studies of Robin and colleagues and Schwab and colleagues reporting high prevalences of scoliosis in elderly adults both demonstrate little effect on self-reported health status including pain compared with adults without scoliosis. In contrast, other large studies comparing adults with scoliosis to unaffected controls demonstrate significant impairment in adults with scoliosis.10–14 In a long-term follow-up study of adults with late-onset adolescent scoliosis compared with unaffected controls, adults with scoliosis complained of chronic back pain more often than controls (61% vs. 35%).15 However, overall adults with late-onset adolescent scoliosis are equally productive and function at a relatively high level. Similarly, in a long-term follow-up of adults treated with bracing for adolescent idiopathic scoliosis, adults with scoliosis had measurably more back pain and functional limitations than unaffected controls.16 In a comparison of adults with scoliosis and unaffected controls matched for age, gender, and educational level, Berven and colleagues17 demonstrated measurable impairment of the adults with scoliosis in domains that include pain, function, mental health, and appearance. The development and validation of a disease-specific measure of health status for adults with scoliosis enables an accurate measure of clinical impact and change in health status for adults with scoliosis.18 Measurement of clinical impact and change in health status as a result of treatment is important in defining the value of care for adults with scoliosis.
The costs to the U.S. health care system involved in treating adult deformity are significant. In 2005 the overall cost of spine-related expenses was $86 billion.19 In 2004 $3.7 billion were spent on 134,000 hospital inpatient stays for patients older than 18 with a hospital discharge diagnosis of spinal deformity.20 In addition, there were 410,000 outpatient physician visits by adults with spinal deformity in 2004.21 The outpatient sector including emergency department visits and prescription medications is a significant and rapidly growing cost to our healthcare system.22 In a healthcare economy with limited resources, it is important to identify diseases and disorders that have a significant impact on patient-based assessment of quality of life and to identify treatments that may have a clinically significant impact on improving health-related quality of life. The management of adults with spinal deformity is an area with tremendous potential for improving health-related quality of life.
Classifying Adult Scoliosis
A classification of adult scoliosis is useful to accurately characterize a deformity pattern, to guide treatment and decision making, and to form a basis for the uniform reporting of results of care that may lead to an evidence-based approach to care.23 Adult scoliosis may be broadly divided into scoliosis that existed before skeletal maturity and scoliosis that developed after skeletal maturity, or de novo scoliosis. A nominal classification system for scoliosis was initially introduced by the Terminology Committee of the Scoliosis Research Society in 1969.24 The classification was etiologic and divided disorders of the spine into categories including idiopathic, congenital, neuromuscular, associated with neurofibromatosis, mesenchymal, traumatic, secondary to irritative phenomena, and other. A nominal classification is useful to lend insight into diagnosis and associated comorbidities. The importance of recognizing the etiology of spinal deformity is demonstrated by the disparity of previous publications on natural history and outcome in scoliosis treatment.25–27 The limitations of a nominal system are that it provides little insight into clinical symptoms and lacks guidance for care of specific curve types and locations. In adult scoliosis, global sagittal balance and symptomatic degenerative changes within the deformity are important determinants of the clinical impact of scoliosis on health status and strategies for care. Therefore specific radiographic features of adult deformity are a useful basis for a classification system in the adult.
King and colleagues introduced an ordinal classification system for thoracic idiopathic scoliosis that was intended to provide guidance for treatment of thoracic deformity in children and young adults.28 The authors demonstrated that the classification has significant value in determining the appropriate levels for fusion for thoracic deformities, and with the use of distraction instrumentation, the system led to a low rate of late decompensation and revision surgery. However, the classification has significant limitations including in applicability to current segmental instrumentation systems,29 applicability to patients with lumbar deformity,30 and recognition of alignment and deformity in the sagittal plane.31–33
The Lenke Classification of adolescent idiopathic scoliosis was developed by members of the Harms Study Group with the intent to be comprehensive and encompass all curve types, to be based on objective criteria for each curve type, to emphasize sagittal plane alignment, and to be easily understood and applied.34 The Lenke classification provides a standardized and useful framework for determining the extent of spinal arthrodesis in deformity.35,36 However, there is significant variability in the observed choice of levels by surgeons because of specific structural characteristics within the deformity, and most importantly because of considerations that are apparent from the patient’s clinical presentation that “override” radiographic considerations.37
The adult with spinal deformity presents with clinical and radiographic characteristics that are distinct from the adolescent with spinal deformity. In the adult with scoliosis, specific radiographic parameters have a significant impact on health-related quality of life. Global sagittal alignment has the most significant impact on pain and function, compared with other radiographic parameters including curve location, curve magnitude, and coronal balance.38 Schwab and colleagues39 developed a classification of adult scoliosis that emphasized the clinical impact of specific radiographic parameters including lumbar curve apex, lumbar lordosis, and intervertebral subluxation within the deformity. Further development of this system will include other radiographic parameters including pelvic incidence, trunk inclination, and lumbopelvic relationships.40
The recognition of symptomatic degenerative changes within the deformity including stenosis, spondylolisthesis, and rotational subluxation is critical for an effective classification system in the adult. Similarly, global imbalance of the spine in the sagittal and coronal plane is rare in adolescent idiopathic scoliosis but has an important impact on health status and treatment options in the adult patient. In the Scoliosis Research Society (SRS) Classification of Adult Deformity, Lowe and colleagues41 incorporated radiographic parameters with clinical modifiers. The SRS Classification of Adult Deformity is presented in Table 73–1. The SRS Classification for Adult Deformity is intended to be used by physicians to group patients with similar radiographic presentations and to assist useful multicenter collaborations and comparisons of similar cases. Further work in identifying key factors that influence surgical decision making and outcomes of care will lead to developments of useful classifications for adult scoliosis.
TABLE 73–1 Scoliosis Research Society Classification of Adult Spinal Deformity
| Adult Spinal Deformity Modifiers | |
| Regional sagittal modifier (include only if outside normal range as listed) | |
| (PT) Proximal thoracic (T2-T5) | ≥+20° |
| (MT) Main thoracic (T5-T12) | ≥+50° |
| (TL) Thoracolumbar (T10-L2) | ≥+20° |
| (L) Lumbar (T12-S1) | ≥–40° |
| Lumbar degenerative modifier (include only if present) • (DDD) ↓ disc height, facet arthropathy, spinal stenosis based on radiograph and/or magnetic resonance imaging | |
| Global balance modifier (include only if imbalance present) | |
Clinical Presentation of Adult Scoliosis
The adult with scoliosis may present to a physician caring for disorders of the spine with symptoms that are directly related to the deformity or with pain or symptoms of spinal origin that are unrelated to the presence of scoliosis. Patients with symptomatic adult spinal deformity characteristically present with symptoms related to back pain, radicular symptoms, deformity, progression of the deformity, coronal or sagittal imbalance, or neural compromise. Smith and colleagues42 identified back pain and radicular pain as a complaint in 99% and 85% of patients with adult scoliosis presenting to a neurosurgical practice, and nearly 10% of patients had neural symptoms including weakness and myelopathy. Correlation of clinical symptoms with deformity patterns and degenerative changes within the spine is an important challenge for the physician caring for patients with adult scoliosis. Recognizing patterns of referred pain and radicular pain is useful in identifying a source of pain or spinal origin and in directing nonoperative and operative care.43,44 Careful attention to the patient’s clinical symptoms and goals of care is important in aligning the physician and patient toward a shared process of decision making and toward a satisfactory outcome of care.45
The adult with scoliosis characteristically presents with symptoms that include axial and neurogenic pain, as well as progressive truncal imbalance.46–49 Degenerative changes within the spinal column are an important component of the clinical presentation of adult scoliosis. Spinal stenosis, rotatory subluxation, and nerve compression occur frequently in adult scoliosis and are an important consideration in the patient’s decision to pursue care.50–52 Glassman and colleagues studied a matched cohort of patients with scoliosis who chose to pursue surgery, compared with patients who chose nonoperative care. The authors found that patients who chose surgery had more frequent leg pain, more frequent episodes of moderate to severe back pain, and a higher mean level of daily back pain. Patients who chose surgery also self-reported more impairment with social function and appearance. In a similar study comparing adult scoliosis patients who chose surgical versus nonoperative care, Pekmezci and colleagues demonstrated that functional measures including walking ability and vitality were important determinants of patient preference for surgery over nonoperative care. These studies clearly indicate the importance of identifying and recognizing the patient’s symptoms and goals for care in planning an approach to care.
Present pain and disability are common in the adult presenting with adult scoliosis. These symptoms are not as prevalent in adolescent idiopathic deformity.53–55 The differences in curve patterns and in clinical presentation between the adult with scoliosis and the adolescent with idiopathic scoliosis underlie the fundamental differences in the goals of treatment and surgical strategies for these populations. In the adolescent with idiopathic scoliosis, the goal of care is to prevent progression of deformity and consequences of deformity progression including pain, functional limitations, and truncal imbalance. In the adult with degenerative scoliosis, the goal of care is to improve present pain and disability. The presence of measurable compromise in health-related quality of life in the adult with degenerative scoliosis offers a measurable variable of the success of management and a quantifiable approach for developing an evidence-based approach to care based on patient self-assessment of changes in health status.
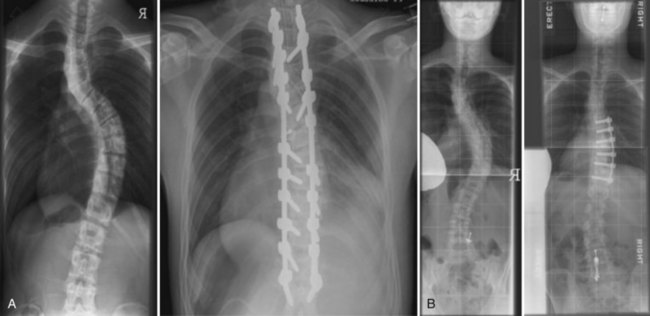
Deformity and concern about progression of deformity are also important considerations in the clinical presentation of the patient with adult scoliosis. Deformity in adult scoliosis may involve malalignment in the coronal, axial, and sagittal planes. Patients with coronal plane deformity often complain of waist asymmetry and ribs abutting the pelvis. The ribs on the concavity of the fractional curve or convexity of the thoracolumbar major curve may approximate the iliac crest and pelvic brim, and patients may complain of painful impingement most commonly in the transition from sitting to standing. Patients with sagittal plane deformity may complain of fatigue and pain on trying to stand erect. Patients may compensate for sagittal plane deformities in the spine with hyperextension of the hips and flexion of the knees. An assessment of pelvic tilt on clinical examination and on standing radiographs is useful in assessing the overall sagittal balance of the spine. Patients with rotation of the spine may complain of rib prominence and apical pain with sitting. Patients with prominent rib deformity may also complain of dissatisfaction with appearance and fit of clothing. Correction of deformity is one of the most reliable goals of surgical intervention for deformity. However, many patients with significant deformity may have limited complaints referable to the deformity. Therefore careful communication with the patient is critical to recognize the role of deformity in the patient’s clinical presentation. Figure 73–1 demonstrates a patient with significant coronal deformity with little pain or functional limitation. A correction of deformity in this patient would be unlikely to improve health-related quality of life in the absence of significant preoperative compromise or deficits.
Progression of deformity in the adult is common and is a reason for which ongoing follow-up of adults with scoliosis is an important role of the physician caring for disorders of the spine. Weinstein and colleagues56 followed a cohort of 194 adult idiopathic scoliosis patients for more than 40 years and noted that 68% had progression of their deformity after skeletal maturity. Thoracic curves greater than 50 degrees had the greatest progression followed by thoracolumbar and lumbar curves. With aging, other important changes in spinal curves include progression of curve size, a loss of lumbar lordosis, and reduced flexibility within the deformity.57,58 Deviren and colleagues59 demonstrated a correlation between age and lateral subluxation within the deformity and the presence of radicular pain. Age-related changes in the spine are an important cause of progressive deformity and progressive symptoms in the adult with scoliosis.
Clinical Evaluation
Activity and walking tolerance are important measures of function. The increasing requirement of walking aids such as a cane or walker may be due to loss of coronal and sagittal balance or to progressive neural dysfunction. Evaluation of gait is an important component of the physical examination. Gait disturbance may be caused by neurogenic etiology, pain, or functional or true leg length inequality. An antalgic gait may be due to axial pain or to radicular pain. Recognition of pathologic gait patterns including ataxic and spastic gaits is important in identifying upper motor neuron pathology including cervical stenosis, myelopathy, and neurodegenerative conditions.60–62 Pelvic obliquity and functional leg-length discrepancy may lead to gait disturbance with characteristic tilting toward the functionally short side for stride clearance. Patients may require support while standing due to fixed coronal imbalance.
An assessment of deformity is an important component of the clinical evaluation. The patient’s self-perception of the deformity may be different than the assessment of a family member or physician.63,64 Donaldson and colleagues65 demonstrated that significant variability in surgeon assessment of deformity may lead to inconsistencies in recommendations regarding operative care. Communication between the physician and patient regarding deformity is important to clarify the patient’s goals of care. Impairment of appearance and self-image is also an important clinical consideration in patients with adult scoliosis and an important goal of deformity correction.66
Careful physical examination is important in the assessment of deformity, localization of pain, and detection of neural deficits. On examination of the patient from the posterior aspect, note the waist asymmetry, trunk shift, and relative heights of the iliac crests. Measurement of leg lengths is important in determining whether pelvic obliquity may be related to a deformity between the pelvis and spine or due to leg-length discrepancy. A plumb line dropped from the spinous process of C7 will demonstrate clinical displacement relative to the midsacral point. The deviation of this line from the gluteal cleft measures the coronal imbalance. The flexibility of the deformity may be determined by testing the patient’s lateral bending or by lifting the patient under the axilla to assess passive correction. Clavicle asymmetry, or elevation of the clavicle contralateral to the major structural curve, will alert the surgeon to the importance of including the upper thoracic curve in the instrumented construct to prevent exacerbation of shoulder asymmetry.67 Figure 73–2A and B demonstrate the importance of extending fixation to include the upper thoracic curve in patients with preoperative elevation of the shoulder ipsilateral to the convexity of a major curve.
Physical examination must also include consideration of the sagittal profile. Inspecting from the side view demonstrates the patient’s lumbar lordosis, sagittal profile, and hip or knee flexion. Patients may compensate for a fixed sagittal malalignment with bending at the knees and extension at the hips. Asking patients to stand with knees fully extended, and noting pelvic tilt on physical examination will yield a more accurate assessment of fixed sagittal plane deformity. Resolution of deformity in the sitting posture may implicate flexion at the pelvic-femoral junction in the cause of sagittal malalignment. The Thomas test performed with the patient supine and pelvis level will demonstrate whether there is a contracture at the pelvic-femoral junction. Recognizing deformity in the sagittal plane is important for surgical planning and for effective improvement of sagittal plane malalignment.68
Radiographic Evaluation of Coronal Imbalance
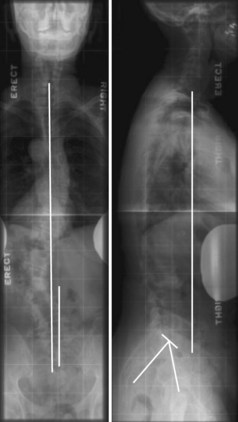
Radiographic assessment of the adult with scoliosis requires standing 36-inch posteroanterior (PA) and lateral views. To obtain a true representation of coronal and sagittal balance, the patient’s knees and hips should be fully extended and leg-length discrepancy should be balanced with standing blocks. The film should also include the center of the femoral heads and the C7 vertebrae in order to measure pelvic incidence, pelvic tilt, and global spinal balance (Fig. 73–3). The Cobb angles should be measured on the PA and side-bending radiographs. The stable, neutral, and apical vertebrae should also be identified on the PA and side-bending films to aid with preoperative planning. The central sacral line (CSL) is the vertical line extended from the spinous process of S1, perpendicular to the pelvis on the PA radiograph. The stable vertebra is the vertebra that is most closely bisected by the CSL. The neutral vertebra is the nonrotated vertebra at the caudal end of the curve. The apical vertebra is the farthest from the CSL. In adult scoliosis, there is often lateral subluxation of the vertebral bodies and spondylolisthesis within the deformity. Degenerative changes including lateral subluxation and spondylolisthesis are associated with spinal stenosis and neurogenic symptoms. Inadequate plain film evaluation may lead to an incomplete assessment of the causes and extent of deformity.69
Radiographic assessment of flexibility of the spine is useful for the preoperative surgical planning. Supine side-bending films are commonly used and give the surgeon an indication of the flexibility of the major and fractional curves. In patients with more severe deformity, other techniques to assess flexibility of deformity include traction radiographs,70 the push prone technique,71 and fulcrum-bending technique.72 In short radii and larger curves, traction radiographs may give a better indication of flexibility than bending due to constraints between the rib cage and pelvis. The lateral flexion and extension film is useful to measure sagittal plane flexibility and to identify fixed kyphotic deformities. Sagittal plane mobility is an important consideration in surgical planning including the use of osteotomies and the choice of end vertebra. Dynamic instability on flexion and extension films may influence the extent of surgical instrumentation and fusion.
Neural deficits and radicular symptoms are an important clinical presentation of adult scoliosis. Advanced imaging with magnetic resonance imaging (MRI) or computed tomography (CT) scan is important to assess the role of decompression of the neural elements. Spinal canal stenosis and foraminal narrowing are common findings that may need to be addressed if they correlate with findings on history and physical examination. Intrinsic intervertebral disc degeneration is best measured with MRI, and facet arthropathy is most apparent with CT scan. Consideration of advanced and symptomatic degeneration of the caudal motion segments is important in selection of fusion levels. In the osteoporotic patient with compression fractures, MRI is also helpful in detecting recent fractures that may be amenable to nonoperative or less invasive surgical options (vertebral augmentation). In patients with previous fusions or attempted fusions, CT and bone scans are useful to assess bony union or the presence of a pseudarthrosis.73,74
Treatment of Adult Scoliosis
Guidance on when to do more, less, or nothing at all can be useful for the surgeon who is considering a spectrum of options and strategies for care. There is tremendous variability in the management of adult spinal deformity among physicians who care for patients with spinal deformity. Although some of this is driven by the range of pathology and complex expression of the aging spine with deformity, the presence of variability in treatment is also related to the absence of an evidence-based approach to adult deformity. The roles of nonoperative care, decompression alone, limited stabilization, or long fusions have been incompletely defined, and indications for each approach remain in evolution. Shared decision making regarding care for the adult with scoliosis requires clear and extensive communication between the physician and the patient in order to empower the formation of an informed choice. An informed choice regarding healthcare alternatives is based on considerations of the magnitude of the intervention, the expected change in health status, and durability of the change in health status over time. The evidence for each alternative remains incomplete and requires ongoing prospective investigation.75
Nonoperative Care in Adult Scoliosis
Nonoperative approaches to the management of adult scoliosis are directed toward improvement of pain and function, not toward correction of deformity or affecting the pattern of curve progression. There is limited evidence to support the efficacy of nonoperative care for the adult with symptomatic scoliosis.76 Van Dam reported that nonoperative care in adults with scoliosis is most useful in patients with limited pain and symptoms and that patients with significant symptoms received limited benefit from analgesics, orthoses, physical therapy, and activity modification.77 Dickson and colleagues reported on a cohort of patients who were operative candidates and choose nonoperative care. Compared with patients who choose surgery, the group treated nonoperatively had significantly more pain and functional limitations. Smith and colleagues78 reviewed the change in health status of 170 adults with scoliosis treated nonoperatively. The authors found no improvement in pain, disability, or SRS-22 score at 2-year follow-up.78 Each of these studies may be criticized for the absence of a specified protocol for nonoperative care.
Specific treatments for the nonoperative management of adult scoliosis include analgesics, orthotics, physical therapy, manual manipulation, activity modification, behavioral therapy, and injections.79–81 Glassman and colleagues82 reviewed the nonoperative resources used by 123 adults with scoliosis. Sixty-eight patients (55%) reported the use of one or more nonoperative modality including medications, physical therapy, exercise, injections/blocks, chiropractic care, pain management, bracing, and bed rest at a mean treatment cost over the 2-year period of $10,815. Patients treated nonoperatively reported no improvement in pain or disability over a 2-year follow-up. This study brings into question the value of nonoperative treatment commonly used for adult scoliosis patients. Cooper reported on the effect of transforaminal lumbar epidural injections on adults with scoliotic stenosis.83 The author defined a successful outcome as patient satisfaction and at least a two-point improvement on pain and function scores. The authors found good early results, with 60% of patients reporting success at 1 week after injection. However, the results declined significantly with only 27% of patients reporting success at 2-year follow-up. Injections including selective nerve blocks and facet blocks may be useful in identifying symptomatic neural compression and localizing pain generators.84–86 The value of discography in decision making regarding extension of arthrodesis to the lower lumbar spine and pelvis is limited.87,88
Operative Care in Adult Scoliosis
Aging population demographics and advances in surgical technique and anesthesia, combined with changing patient attitudes toward pain and limitations, have contributed to increased surgical rates for adult spinal deformity.89 Compared with the adolescent population, surgery for adult deformity is often more complex and technically difficult. Patients are older and may have significant medical comorbidities. These factors contribute to a high reported rate of complications that can result in the need for reoperation and questioning the value of limited improvement in health-related quality of life compared with the risk of surgery.90
The surgical goals in treating the patient with degenerative scoliosis include neural decompression, improvement of back pain, and restoration of spinal alignment.91,92 Indications for surgery in adult scoliosis include the following:
As discussed in the section on clinical presentation, patients who choose operative care over nonoperative care are more likely to have radicular pain or more severe pain and measurable functional limitations. The decision to pursue operative care over nonoperative care requires an assessment of the expected benefits of surgery compared with the cost of intervention including the risk of perioperative complications. In a debate on operative versus nonoperative care of adult scoliosis, Akbarnia and colleagues reviewed literature that included significant risks to scoliosis in the adult including reported complications of 56% to 75%, unplanned reoperations in 18% to 58%, and unproven benefits regarding improvement in health-related quality of life.93 However, since their review, several studies comparing operative and nonoperative management of adult scoliosis have consistently demonstrated better outcomes with operative care.94–96 Smith and colleagues97 reported on the risk of perioperative complications compared with improvement of health status measure by Oswestry Disability Index. The authors identified more perioperative complications in older adults but a parallel improvement in health status and disability. They concluded that the benefits of operative management of scoliosis in the adult appear to exceed the significant risks for all age groups.
Preoperative Planning and Medical Considerations
Comorbidities are an important determinant of health status and perioperative complications.98 Improvements in surgical techniques and perioperative care have expanded our ability to care for adults with significant comorbidities including pulmonary and cardiac disease, osteoporosis, and nutritional deficiency. With proper planning and patient preparation, medical conditions affecting adult patients can be optimized to decrease, although not eliminate, the perioperative risk.99 Additional potential benefits include decreasing hospital length of stay and recovery for the patient, as well as decreasing overall costs, and therefore use of resources is of benefit to society as a whole. With increasing review of quality of care, it is doubly important that we be vigilant in identifying and optimizing patient baselines preoperatively whenever possible.
Preoperative cardiac and pulmonary assessment is of special importance in the adult patient, especially in a surgical era when age is not a contraindication to major deformity correction. Preoperative pulmonary function testing is useful in patients with a history of frequent pneumonias, associated neuropathic (cerebral palsy, poliomyelitis) or myopathic (muscular dystrophy, primary myopathies) weakness, or subjective dyspnea. Irreversible preoperative vital capacity compromise is a predictor of postoperative respiratory complications.100,101 Other areas of physical health to assess include bone quality, nutritional status, obesity, and tobacco use. Each of these areas may be optimized before considering elective surgical correction. In addition to physical health, the surgeon may consider social, financial, and psychologic well-being of the patient because spinal deformity surgery and subsequent recovery will surely affect all of these areas. Patients who are in optimal physical shape, irrespective of their age, and who are participating in some aerobic activity, have ceased smoking for at least 2 to 3 months, and who are nutritionally sound are more likely to respond to the nonoperative approach and will be better prepared for recovery after surgery.102
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree