Approximately 2 million sports and recreation concussive injuries occur per year in the United States, which may be an underestimate because of inconsistent data reporting. The field of concussion management has evolved rapidly over the last 10 years, and with these advances comes new understanding of the significant symptomatic and cognitive impairments of concussion. These sequelae are more fully realized and may last longer than previously thought. Data have emerged regarding pathophysiology of concussion, risk factors, outcome, effects of repetitive injury, subtypes of concussive injury, and treatment protocols. This evidence calls for more conservative management of concussion, particularly in younger athletes, and demonstrates the shortcomings of concussion guidelines.
Approximately 2 million sports and recreation concussive injuries occur per year in the United States . Due to inconsistent data reporting, this is likely an underestimation of actual cases. The field of concussion management has evolved rapidly over the last 10 years, and with these advances comes new understanding of the significant symptomatic and cognitive impairments of concussion. These sequelae are more fully realized and may last longer than previously thought. Data have emerged regarding pathophysiology of concussion, risk factors, outcome, effects of repetitive injury, subtypes of concussive injury, and treatment protocols. This evidence calls for more conservative management of concussion, particularly in younger athletes, and demonstrates the shortcomings of concussion guidelines.
The practice of concussion management is moving from a general grading or guideline system toward individualized management based on scientific evidence of varied symptom presentations and recovery courses. Management protocols currently individualize assessment with the use of neurocognitive testing and comprehensive symptom evaluation. These evidence-based paradigms are emerging as the standard of care for management of concussion and return-to-play decisions.
Definition
Over the years, various academic organizations have proposed specific definitions of concussion; however, any definition of concussion has yet to be accepted universally. This lack of consensus becomes especially problematic when evaluating athletes in the field and determining whether an athlete has sustained a concussion or is experiencing pre-existing or unrelated symptoms. The Committee on Head Injury Nomenclature of Neurological Surgeons and the American Academy of Neurology (AAN) have proposed two such definitions that have been widely cited. The Committee on Head Injury Nomenclature of Neurological Surgeons defined concussion as “a clinical syndrome characterized by the immediate and transient post-traumatic impairment of neural function such as alteration of consciousness, disturbance of vision or equilibrium, etc., due to brain stem dysfunction.” The American Academy of Neurology defined concussion as “any trauma induced alteration in mental status that may or may not include a loss of consciousness.”
Most recently, the Centers for Disease Control and Prevention proposed a comprehensive definition of concussion. This definition aims to educate clinicians of the individualized nature of the injury, identifying key concepts that allow for a flexible approach to diagnosing and managing the injury. The Centers for Disease Control and Prevention definition reads :
“A mild traumatic brain injury (mTBI) or concussion is defined as a complex pathophysiologic process affecting the brain, induced by traumatic biomechanical forces secondary to direct or indirect forces to the head. MTBI is caused by a jolt to the head or body that disrupts the function of the brain. This disturbance of brain function is typically associated with normal structural neuroimaging findings (ie, CT scan, MRI). MTBI results in a constellation of physical, cognitive, emotional and or sleep-related symptoms that may or may not involve a loss of consciousness (LOC). Duration of symptoms is highly variable and may last from several minutes to days, weeks, months, or longer in some cases.”
Pathophysiology
Recent work by Giza and Hovda and colleagues in animal models has led to insight regarding the pathophysiology of mild traumatic brain injury (TBI). Their findings suggested that concussion is a metabolic brain injury, rather than structural, with acute, posttraumatic changes occurring in intracellular and extracellular environments. These changes result from excitatory amino acid–induced ionic shifts associated with increased Na/K ATPase activation and resultant hyperglycolysis . This process is accompanied by a decrease in cerebral blood flow that is not well understood, although it may be secondary to accumulation of endothelial calcium, which is thought to cause widespread cerebral neurovascular constriction. The resulting “metabolic mismatch” between energy demand and energy supply has been postulated to propagate a cellular vulnerability that is particularly susceptible to even minor changes in cerebral blood flow, increases in intracranial pressure, and apnea. Such metabolic dysfunction is theoretically linked to second impact syndrome and may form the basis for the less severe—although potentially incapacitating—postconcussion syndrome .
Animal models have indicated that this dysfunction can last up to 2 weeks or theoretically longer in the human model and can occur in athletes with normal Glasgow coma scores . Traditional neurodiagnostic techniques (eg, CT scan, MRI, neurologic examination) are almost invariably normal after concussive insult . It should be stressed, however, that these techniques are invaluable in ruling out more serious pathology (eg, cerebral bleeding and skull fracture) that may occur with head trauma.
Pathophysiology
Recent work by Giza and Hovda and colleagues in animal models has led to insight regarding the pathophysiology of mild traumatic brain injury (TBI). Their findings suggested that concussion is a metabolic brain injury, rather than structural, with acute, posttraumatic changes occurring in intracellular and extracellular environments. These changes result from excitatory amino acid–induced ionic shifts associated with increased Na/K ATPase activation and resultant hyperglycolysis . This process is accompanied by a decrease in cerebral blood flow that is not well understood, although it may be secondary to accumulation of endothelial calcium, which is thought to cause widespread cerebral neurovascular constriction. The resulting “metabolic mismatch” between energy demand and energy supply has been postulated to propagate a cellular vulnerability that is particularly susceptible to even minor changes in cerebral blood flow, increases in intracranial pressure, and apnea. Such metabolic dysfunction is theoretically linked to second impact syndrome and may form the basis for the less severe—although potentially incapacitating—postconcussion syndrome .
Animal models have indicated that this dysfunction can last up to 2 weeks or theoretically longer in the human model and can occur in athletes with normal Glasgow coma scores . Traditional neurodiagnostic techniques (eg, CT scan, MRI, neurologic examination) are almost invariably normal after concussive insult . It should be stressed, however, that these techniques are invaluable in ruling out more serious pathology (eg, cerebral bleeding and skull fracture) that may occur with head trauma.
On-field management
The diagnosis of cerebral concussion can be difficult, even in ideal circumstances. Athletes may have had neither direct trauma to the head nor loss of consciousness (LOC). Athletes may be unaware that they have been injured immediately after the injury and may not show any obvious signs of concussion, such as clumsiness, gross confusion, or obvious amnesia. To complicate this situation, athletes at all levels of competition may minimize or hide symptoms in an attempt to prevent their removal from the game, which creates the potential for exacerbation of the injury. Appropriate acute care and management of athletes with concussion begin with a detailed and accurate assessment of the nature and severity of the injury. As with any serious injury, the first priority is always to evaluate an athlete’s level of consciousness and airway, breathing, and circulation.
Sideline presentation of symptoms may vary widely from athlete to athlete, depending on the biomechanical forces involved, severity of injury, affected brain areas, and an athlete’s prior history of injury. Given the subtleties and variation in the presentation of a concussive injury, a thorough assessment of all signs and symptoms is crucial in making an accurate diagnosis of concussion. After a concussion, athletes may present with as few as one symptom or a constellation of many postconcussion symptoms, any and all of which are important from a diagnostic and management standpoint ( Table 1 ).
| Signs observed by staff | Symptoms reported by athlete |
|---|---|
| Appears to be dazed or stunned | Headache |
| Is confused about assignment | Nausea |
| Forgets plays | Balance problems or dizziness |
| Is unsure of game, score, or opponent | Double or fuzzy/blurry vision |
| Moves clumsily | Sensitivity to light or noise |
| Answers questions slowly | Feeling sluggish or slowed down |
| Loses consciousness | Feeling “foggy” or groggy |
| Shows behavior or personality change | Concentration or memory problems |
| Forgets events before play (retrograde) | Change in sleep pattern (appears later) |
| Forgets events after hit (posttraumatic) | Feeling fatigued |
Key acute signs
Loss of consciousness
Upon ruling out more severe injury, the acute evaluation continues with assessment of concussion. Several possible tools are available to guide physicians in their evaluation, including the acute concussion evaluation and the materials in the Centers for Disease Control and Prevention’s toolkit for physicians, “Heads Up: Brain Injury in Your Practice” . First, a clinician should establish the presence of any LOC. By definition, LOC represents a state of brief coma in which the eyes are typically closed and the athlete is unresponsive to external stimuli. The athlete who has a concussion is infrequently rendered unconscious, with studies indicating that 4% to 10% of sports-related concussions result in LOC . Prolonged LOC (>1–2 min) in sports-related concussion is much less frequent , and athletes with LOC are typically unresponsive for only a brief period. Any athlete with documented LOC should be managed conservatively, and return to play is contraindicated.
Confusion
Confusion or disorientation, by definition, represents impaired awareness and orientation to surroundings, although memory systems are not directly affected. Confusion is often manifested by an athlete appearing stunned, dazed, or glassy-eyed on the sideline. Confusion is frequently revealed in athletes having difficulty with appropriate play calling, answering questions slowly or inappropriately, or repeating oneself during evaluation. Teammates are often the first to recognize that an athlete has been injured given the level of disorientation and difficulty in maintaining the flow of the game. Upon direct evaluation by the physician or athletic trainer, the athlete may be slow to respond. To assess properly the presence of confusion, simple orientation questions can be asked to the athlete (eg, name, current stadium, city, opposing team, current month and day) ( Box 1 ).
On-field cognitive testing
Orientation (ask the athlete the following questions)
What stadium is this?
What city is this?
Who is the opposing team?
What month is it?
What day is it?
Posttraumatic amnesia (ask the athlete to repeat the following words): girl, dog, green
Retrograde amnesia (ask the athlete the following questions)
What happened in the prior quarter or half?
What do you remember just before the hit?
What was the score of the game before the hit?
Do you remember the hit?
Concentration (ask the athlete to do the following)
Repeat the days of the week backward, starting with today
Repeat these numbers backward: 63, 419
Word list memory
Ask the athlete to repeat the three words from earlier (girl, dog, green)
Retrograde and anterograde amnesia
A careful evaluation of amnesia is of paramount importance in the athlete who has a concussion. Amnesia may be associated with loss of memory for events preceding or after injury. Specifically, posttraumatic amnesia or anterograde amnesia (synonymous terms) is typically represented by the length of time between trauma and the point at which the individual regains normal continuous memory functioning. As outlined in Box 1 , on-field anterograde amnesia may be assessed through immediate and delayed (eg, 0, 5, 15 minutes) memory for three words (eg, girl, dog, green). It should be noted that confusion and anterograde amnesia are not mutually exclusive and may be hard to dissociate. To help clarify this issue, anterograde amnesia represents a loss in memory from the point of injury until the return of a full, ongoing memory process. Confusion in and of it itself is not associated with memory loss. These two markers of injury may be assessed properly once the athlete’s confusion is clear and lucid mental status returns. At that point, simply ask the athlete to recall the specific events that occurred immediately subsequent to trauma (eg, memory of returning to sideline, memory for subsequent plays, memory of later parts of contest). Any failure to recall these events properly indicates anterograde amnesia. Any presence of amnesia, even in seconds, has been found to be highly predictive of postinjury neurocognitive and symptom deficit .
Retrograde amnesia, although given less focus in the literature, is also an important injury severity marker of concussion. Retrograde amnesia is defined as the inability to recall events that occurred during the period immediately preceding trauma. To assess on-field retrograde amnesia properly, athletes may be asked questions pertaining to details occurring just before the trauma that caused the concussion. As Box 1 highlights, asking athletes to recall details of the injury is a good starting point. From there, asking athletes to recall the score of the game before the hit, events that occurred in the plays preceding the injury, and events that occurred in the first quarter or earlier in practice is a practical assessment strategy. It should be noted that the length of retrograde amnesia typically “shrinks” over time. For example, as recovery occurs, the length of retrograde amnesia may contract from hours to several minutes or even seconds, although by definition, a permanent loss of memory preceding injury occurs. Once again, even seconds of retrograde amnesia may be considered pathognomonic and predictive of outcome.
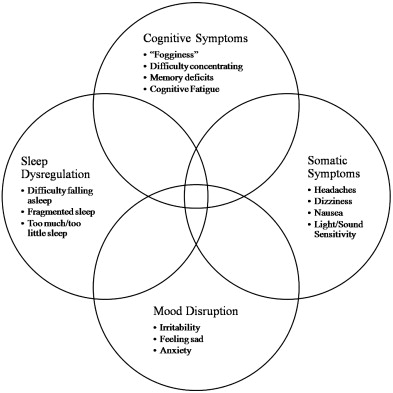
Symptoms
A thorough assessment of symptoms is critically important in an appropriate evaluation of a concussion. Four classes of symptoms should be assessed (ie, somatic, cognitive, emotional, sleep), although certain symptoms are more prevalent or may be manifested in the earlier or later stages of the injury ( Fig. 1 ). For obvious reasons, sleep-related symptoms are not present on the day of the injury; however, they may be a significant issue after the first night’s sleep. The following sections highlight several key symptoms often seen early in the injury.
Headaches (somatic)
Headaches are the most commonly reported symptom of concussion and have been reported in up to 70% of athletes who have concussion . Assessment of postconcussion headache is often complicated by the presence of musculoskeletal or myofascial pain–driven headaches that result from whiplash injury, cognitive fatigue headaches (discussed later), or premorbid headache and migraine exacerbation. Headaches caused by concussion may not develop immediately after injury and often do not develop until many hours after injury. Postconcussion headache is worsened with physical exertion; if the athlete complains of worsening headache during exertional testing or return to play, conservative management is indicated. The quality and location of the postconcussion headache seem to be consistent across the duration of recovery and infrequently change in location or character, with the exception of headaches influenced by myofascial pain generators, which can evolve during treatment. Although headache after a concussion does not necessarily constitute a medical emergency, a severe or progressively severe headache, particularly when accompanied by vomiting or rapidly declining mental status, may signal a life-threatening situation and should prompt immediate transport to hospital and CT scan of the brain.
Because of the prevalence of headache in individuals who have concussion, the relationship of headache to outcome was examined recently. One study examined high school athletes who had concussion and reported headache at approximately 1 week after injury versus athletes who did not report headache at that postinjury assessment. Results indicated that athletes with headaches performed significantly worse on measures of reaction time and memory, reported significantly more symptoms on the Post-Concussion Symptoms Scale, and were more likely to have experienced on-field anterograde amnesia than were athletes who did not report headaches . Another recent project that examined headache type and outcome from concussion emphasized the importance of properly characterizing the postconcussion headache. Athletes who reported posttraumatic headaches with migrainous features (eg, nausea, vomiting, photophobia, or phonophobia) demonstrated more pronounced cognitive deficits at postinjury testing than athletes with no headaches or athletes with headaches without migrainous features .
Balance (somatic)
The vestibular system is susceptible to injury with trauma of the head and neck and can occur in the absence of skull base fractures or intracranial pathology . Benign paroxysmal positional vertigo, labyrinthine concussion, perilymphatic fistulae, central vestibular disorders, endolymphatic hydrops, and cervicogenic vertigo have been reported after TBI, and several studies have documented balance deficits in athletes who have concussion . Vestibular therapy, including repositioning techniques for benign paroxysmal positional vertigo, has been successful in managing these symptoms , and referral to a trained vestibular therapist is warranted in athletes with debilitating or ongoing vestibular symptoms.
Mental “fogginess” (cognitive)
Another frequently reported symptom gaining recent research attention is a reported sensation of feeling “foggy” after concussion . Such data have suggested that the presence of “fogginess” after injury may be associated with a more severe course and protracted recovery. High school athletes who endorsed feeling “foggy” on a symptoms inventory were compared with concussed athletes who did not endorse a sense of “fogginess.” Results indicated that the group that felt foggy demonstrated significantly slower reaction times, attenuated memory performance, and slower processing speed via computerized neurocognitive testing. Athletes who felt foggy also endorsed a significantly higher number of other postconcussion symptoms when compared with the group who did not endorse fogginess.
Mood disturbances (emotional)
Changes in mood are another commonly reported or observed symptom after TBI. Most often, athletes report increased irritability or having a “shorter fuse.” Other emotional changes may occur, however, such as sadness, depression, nervousness, and anxiety. Affect may be described by the athlete or parent as flattened or labile. Emotional changes may be brief (eg, a linebacker bursts into tears for 30 seconds on the sideline) or may be prolonged in the case of a more significant injury (athlete reports persistent depression).
Neurocognitive assessment
The most significant advancement in the field is the development and clinical implementation of neurocognitive testing programs that allow for a reliable and valid approach to quantifying major manifestations of the injury, tracking athletes in terms of recovery, and providing a dependent variable to research individual factors in recovery effectively . Neurocognitive testing has contributed to the development of a more individualized and data-driven approach to concussion management. Because concussion is a “functional” rather than “structural” brain injury, neurocognitive testing recently was deemed the cornerstone of proper concussion management through the implementation of baseline testing (preseason/preinjury) and subsequent postinjury evaluations conducted until recovery is complete .
During the initial stages of recovery from sports concussion, computer-based neurocognitive testing procedures have several advantages and relatively few disadvantages when compared with more traditional (ie, “paper-and-pencil” tests) neurocognitive testing procedures. First, the use of computers allows for the evaluation of large numbers of student athletes with minimal manpower. This technology promotes the baseline assessment of an entire athletic team within a reasonable time period using minimal human resources. Second, data acquired through testing can be stored easily in a specific computer or computer network and can be accessed at a later date (eg, after injury). Not only does computerized testing promote the efficient clinical evaluation of the athlete but it also greatly expands the possibilities for research. Third, the use of the computer promotes more accurate measurement of cognitive processes, such as reaction time and information processing speed. Computerized assessment allows for the evaluation of response times that are accurate to 0.01 seconds, whereas traditional testing only allows for accuracy up to 1 to 2 seconds. Fourth, the use of the computer allows for the randomization of test stimuli that may help to improve the reliability of data across multiple administration periods, which minimizes the “practice effects” that naturally occur with multiple exposures to the stimuli. Finally, computer-based approaches allow for the rapid dissemination of clinical information to sports medicine clinicians.
In summary, many benefits are derived from a computer-based approach insofar as the technology has appropriate sensitivity, reliability, and validity to measure the subtle aspects of concussive injury. It should be noted that more comprehensive neurocognitive testing may be indicated in the postacute management of injury and for athletes who exhibit protracted and complicated recoveries. Some clinicians use a “hybrid” approach of complementary computerized and paper-and-pencil test batteries to delineate an athlete’s status.
A potential disadvantage of computer-based neurocognitive testing involves its inappropriate use as a “stand-alone” diagnostic instrument. This approach fails to recognize the complexity of the injury and may not incorporate other pertinent data, such as a detailed clinical interview, overall symptom presentation, medical/concussion history, and the results of other diagnostic studies (eg, balance testing, vestibular assessment).
Currently, several computer-based management approaches have been developed and validated to help determine management and return-to-play issues after concussive injury. Specifically, four computer-based models have been detailed in the scientific literature, including ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing), CogState, Headminders, and ANAM (Automated Neurocognitive Assessment Matrices). Each of these test batteries has examined important aspects of reliability and validity in their approach to measuring concussive injury. Specific computerized test batteries have published additional data examining sensitivity/specificity of their test battery and the “added value” of their assessment tool when compared with the assessment of symptoms in isolation .
Neurocognitive deficits that result from concussion have been documented in many studies, and cognitive testing seems to be a highly valuable tool in documenting impairment or incomplete recovery from concussive injury. Neurocognitive deficits associated with concussion also have been documented in studies of collegiate football players, high school football players, amateur soccer players, and samples of athletes who have concussion across multiple sports. Neurocognitive evaluation is a sensitive tool that may be used to assess the often subtle and potentially debilitating effects of concussive injury. Neurocognitive test data seem to provide objective, quantifiable, and individualized standards to better determine safe return to participation and overall management of the athlete who has concussion and should be considered a critical factor in concussion management.
Treatment paradigm
There are no curative medical treatments for concussion, and clinical observation suggestions that exertion—both physical and cognitive—can delay recovery. This finding underscores the importance of early identification, evaluation, and management of a concussion and the resultant symptoms and prevention of additional injury or exacerbation of a current injury through early return to physical exertion or early return to play. In the initial days after injury, athletes should be instructed on the benefits of proper sleep hygiene, physical rest, and cognitive rest.
Based on published data, approximately 80% of athletes spontaneously recover within 3 weeks of trauma, with the remaining 20% having a “protracted” recovery . Given the strong relationship between exertion and recovery, there has been interest in creating specific concussion rehabilitation protocols that focus on graded exertional protocols from a physical and cognitive perspective. Research is forthcoming regarding this issue.
The diagnosis of postconcussion syndrome is controversial in the medical community, because the symptoms associated with concussion can appear vague and be mistaken for other clinical issues. Despite this debate, distinct symptom clusters and neurocognitive deficits after concussion have been identified. Specific treatment recommendations also may include pharmacologic interventions based on symptom clusters that the athlete may be experiencing. From a treatment standpoint, it has been the philosophy of these authors to avoid pharmacologic intervention until the athlete is at 3 weeks or longer into recovery and there is functional disability as it relates to the experienced symptoms (eg, difficulties in school, severe symptoms) ( Fig. 1 ).
A detailed history is imperative for evaluation and treatment of concussion, including mechanism of injury, location of the impact, length of LOC (if present), presence of retrograde or anterograde amnesia, initial symptoms, and treatment. A comprehensive review of ongoing symptoms should be undertaken. Symptoms consistent with concussion fall into four categories: cognitive, somatic, emotional, and sleep disturbance.
Cognitive
Neurocognitive testing has provided objective data illustrating the multitude of cognitive derangements after concussion. Clinically, individuals may complain of feeling foggy, not being able to think quickly, or not being able to focus attention to complete everyday tasks. Students often complain of declining academic performance. Short-term memory deficits and prolonged reaction times are also apparent. There is clear evidence that the cognitive deficits after TBI improve with the addition of neurostimulant medications . Most of these data involve the more severely brain injured populations; however, the improvements in neurocognitive testing are compelling. Anecdotally, substantial clinical improvement has been noted in individuals treated with methylphenidate, amantadine, or atomoxetine. (Please note that these are off-label uses for these medications.)
Somatic
Headaches are one of the most common symptoms after concussion. Getting specific information regarding the character of the headache is important, because posttraumatic headaches can be caused by multiple underlying causes, including musculoskeletal, vascular, neuropathic, and iatrogenic factors. A thorough history and physical examination help to narrow down these potential causes and help to dictate a treatment plan. Some varieties of posttraumatic headache have been found to be amenable to the same treatment guidelines available for primary headaches and migraines . Prophylactic treatment with beta-blockers, calcium-channel blockers, and antidepressants can play a role. Infrequent posttraumatic migraines also may benefit from abortive medications in the triptan family. Musculoskeletal or tension headaches can be further identified by complaint of pain at the temples or tender spots and decreased neck range of motion on physical examination.
Of particular note, some individuals complain of headaches that occur only in the setting of “cognitive exertion.” For example, athletes who have concussion may complain of headaches that occur and worsen with activities, including taking notes in class or taking tests. Often these individuals also endorse significant cognitive symptoms. These headaches are associated with symptoms of “feeling foggy” or difficulty concentrating. Such headaches have been dubbed by these authors as “cognitive-fatigue” headaches: those that occur in clear relationship with cognitive exertion. For this subtype of headache, treating the cognitive symptoms (rather than the headaches themselves) may prove to be more efficacious. Preliminary data suggest that neurostimulants may aid in headache management by improving the cognitive deficits that act as their trigger. Further research in this arena is warranted.
Emotional
Prolonged, unresolving cognitive and somatic symptoms may cause many individuals to become frustrated and anxious. Mood disorders, including depression, are frequently seen after TBI. These emotional disturbances may worsen perception of cognitive impairment or pain. Initiation of selective serotonin reuptake inhibitors has been shown to be particularly helpful and may have an added benefit of headache prevention.
Sleep disturbance
Disorders of sleep are also well documented after TBI . Although individuals may initially complain of hypersomnia, several weeks after injury they often complain of difficulty falling asleep or staying asleep. Normal sleep-wake patterns can quickly become dysregulated. Proper sleep hygiene, including going to bed and waking at the same times daily, limiting caffeine intake, reducing daytime naps, and eliminating TV watching in bed, should be advocated. Medications such as trazodone, amitriptyline, or melatonin can be used to improve the quality and quantity of sleep. Benzodiazepines and nonbenzodiazepine hypnotics should be avoided because of their amnestic qualities and potential worsening of cognitive functioning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







