Chapter 24 Acute Elbow Dislocations and Management
Introduction
The elbow is the second most commonly dislocated major joint in the body after the shoulder, with an annual incidence of 6.1 dislocations per 100 000 population. Elbow dislocations constitute approximately 10–25% of all elbow injuries and approximately 6.8% of all treated fractures or dislocations.1–3
The most common mechanism of injury is a fall onto the outstretched hand in which the elbow is extended and the shoulder is abducted. This is most often seen with high-energy mechanisms such as motor vehicle accidents and sports injuries. The median age for an elbow dislocation is 30 years.3 Almost all complete elbow dislocations without large periarticular fractures cause rupture of the medial and lateral collateral ligaments. Fortunately, the vast majority of these injuries can be treated conservatively without surgical intervention.
Elbow dislocations are classified according to the direction of forearm displacement relative to the distal humerus. Most consist of posterior or posterolateral displacement although less commonly lateral and anterior displacement of the forearm can also occur. Elbow dislocations can also be classified as simple or complex, and this is determined by the presence or absence of concomitant bony fractures. Simple dislocations are characterized by the absence of associated fractures, while complex dislocations are associated with large periarticular fractures. It should be noted that although pre- and post-reduction radiographs reveal large periarticular fractures in 12–60% of cases (complex elbow dislocations), operative exploration has documented unrecognized soft tissue injuries in nearly 100% of elbow dislocations.4 The most common complex dislocation pattern is an acute elbow dislocation with a fracture of the radial head. However, complex elbow dislocations encompass a wide range of bony and ligamentous injuries that result in elbow instability and usually require surgical intervention. As a result, the rest of this chapter will focus on the anatomy, diagnosis, treatment and outcomes of simple elbow dislocations.
Background/aetiology
Dunning et al performed a biomechanical cadaveric study in which sequential sectioning of the radial collateral and lateral ulnar collateral ligaments was performed in 12 cadaveric elbows. After each stage of the sectioning protocol, internal/external rotation and varus/valgus laxity were evaluated with an electromagnetic tracking device. They noted no significant difference in the magnitude of internal/external rotation and varus/valgus laxity of the ulna, with only the radial collateral or lateral ulnar collateral ligament intact. It was therefore concluded that, when the annular ligament is intact, either the radial collateral ligament or the lateral ulnar collateral ligament can be transected without inducing posterolateral rotatory instability of the elbow.5 The results of this study suggest that surgical approaches which violate only the anterior or posterior half of the lateral collateral ligament complex should not result in posterolateral rotatory instability of the elbow. Therefore a surgical approach to the radial head, for example, can transect the radial collateral ligament and not result in instability. Similarly, a surgical approach that violates the lateral ulnar collateral ligament would also not result in instability provided the radial collateral ligament complex was intact.
Some osseous relationships have also been described in the context of simple elbow dislocation. Wadstrom et al evaluated the anatomical relationship of the semilunar notch of the ulna in patients with elbow dislocation. They compared lateral radiographic views of 100 patients with elbow dislocations with radiographs from 150 patients without dislocation or other radiographic pathology. They noted a lower coronoid process as well as a more prominent tip of the olecranon in the radiographs of patients who had sustained an elbow dislocation. They concluded that the dislocation mechanism was at least partially hyperextension, with the tip of the olecranon acting as the pivot point.6
Presentation, evaluation and initial treatment
Patients with acute elbow dislocation tend to present with pain, soft tissue swelling and an obvious deformity of the elbow (Fig. 24.1). A thorough neurovascular examination of the upper extremity should always be performed. Closed elbow dislocations are rarely associated with vascular injury, and only a handful of brachial artery injuries associated with closed simple elbow dislocation have been reported.7 In open dislocations, however, the brachial artery is more often disrupted due to the forcible hyperextension of the elbow. Median and/or ulnar nerve injury is also commonly associated with such injuries. Neurapraxia has been reported to occur in approximately 20% of elbow dislocations and usually involves the anterior interosseous branch of the median nerve and/or the ulnar nerve. Ulnar nerve palsy has been reported in 14% of adult elbow dislocations, and the incidence is much higher in paediatric elbow dislocations with an associated medial epicondyle fracture. Most neurological deficits are transient, but entrapment of the median nerve within the elbow joint following reduction is relatively common in paediatric elbow dislocations and if not recognized will cause permanent disability.8 The wrist and shoulder joints should be carefully examined to rule out a concomitant upper extremity injury, which have been noted in 10–15% of acute elbow dislocations.9 Of note, the distal radio-ulnar joint (DRUJ) and forearm interosseous membrane should always be examined for tenderness and instability to rule out an associated interosseous membrane disruption.
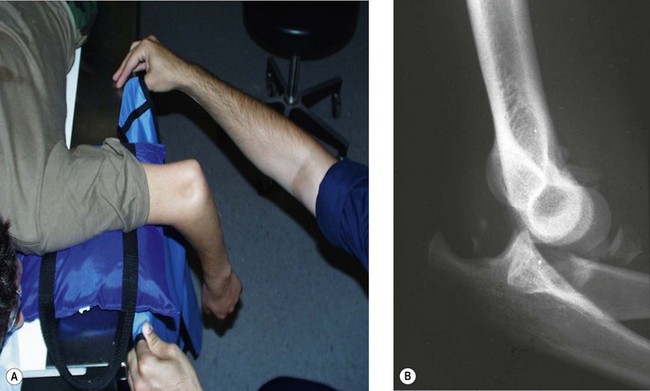
Simple elbow dislocations are acutely treated with reduction. Reduction requires adequate muscular relaxation and appropriate analgesia. This is usually done in the emergency department with intravenous or intramuscular medication. The acute treatment of the posterior or posterolateral dislocated elbow in the emergency department is to place the patient in the prone position and to supinate the patient’s arm. With the proximal part of the arm over a padded bolster on the edge of the examining table, pressure is applied to the olecranon tip in a distal and posterior direction as the elbow is gradually flexed, resulting in reduction. Muscular relaxation is necessary for adequate reduction, and the quality of the reduction often provides a clue to postreduction stability. A palpable reduction ‘clunk’ is a favourable sign of joint stability (Fig. 24.2).10
After determining that the elbow reduction is stable in 30° of flexion, post-reduction AP and lateral radiographs should be performed to document concentric reduction in two planes. In difficult cases, fluoroscopy may be of significant assistance. The radiographs should be assessed for joint widening, irregularity or malalignment. Persistent instability or joint widening may indicate posterolateral rotatory instability or the interposition of soft tissue or osteochondral fragments (Fig. 24.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree