Acromioclavicular Separations: Arthroscopic Reconstruction of The Acromioclavicular Joint
Daniel T. Richards
James J. Guerra
Acromioclavicular (AC) joint dislocations are common injuries encountered in orthopedic medicine. Treatment strategies vary greatly ranging from nonsurgical to complete reconstruction. Despite a recent resurgence of interest in the orthopedic literature about AC joint injuries, treatment recommendations remain controversial. For lesser grade injuries, current literature has reaffirmed the success of nonoperative treatment for many AC joint separations. However, for injuries with significant displacement, surgical management is recommended to restore the normal kinematics of the shoulder. Modern biomechanical testing and recent anatomical dissection have demonstrated inconsistencies related to the more traditionally recommended surgical techniques while providing insight into improving the surgical management of both acute and chronic injuries. Much of this research has focused on the combined use of ultrastrong synthetic materials in combination with biologic grafts.
This chapter presents the most current anatomical, biomechanical, and surgical considerations relating to the treatment of AC joint injuries with a particular focus on arthroscopic surgical techniques.
CLINICAL EVALUATION
History and Physical Exam Findings
As with any acute injury, a complete history and physical exam should be performed for any patient suspected of having an injured AC joint. The history will help determine treatment options for the patient and should focus on the injury mechanism, treatment timing, and the potential for postinjury morbidity. Age, desired sport, and occupational demands warrant special consideration should operative intervention be contemplated. On physical exam, concomitant traction injuries should be noted and a careful examination of the affected shoulder be completed.
Incomplete injuries to the AC joint will likely result in pain localized to the upper shoulder. At times, this pain can be poorly localized. The AC joint has dual innervation from the suprascapular nerve as well as the lateral pectoral nerve, and pain can be referred to their respective dermatomal distributions. Isolation of the AC joint as the location of injury can be accomplished by eliciting pain with direct palpation or provocative maneuvers such as the cross-chest adduction test. Relief of pain with injection of a local anesthetic confirms the diagnosis. With complete injuries, there is almost always pain, swelling, and deformity of the AC joint. Subtle deformities can be confirmed with radiographs.
Diagnostic Imaging
Radiographs are usually sufficient for evaluating potential AC joint injuries. Specific views for optimal assessment have been described. In general, three orthogonal views are adequate to initially evaluate the shoulder for a traumatic injury. These views include an AP, a scapular-Y, and an axillary. If an AC joint injury is further suspected, additional views may be indicated.
Although the AP and scapular-Y views of the shoulder can indicate an AC joint injury, more specific views can reveal additional, more subtle findings. The Zanca view angles the X-ray beam 10° to 15° cephalad in a true AP orientation to eliminate the overlap of the scapular spine (1). The X-ray power should be reduced to 30% to 50% of normal to avoid overpenetration of the less dense AC joint. The Zanca view will reveal any relative displacement of the clavicle. Bilateral Zanca views on the same X-ray cassette allow for comparison with the contralateral side (Fig. 4.1). Bearden et al. (2) demonstrated in their study
that the mean distance between the superior border of the coracoid and the inferior border of the clavicle was 1.1 to 1.3 cm. As this distance will vary between patients and radiographic techniques, it is necessary to compare side-to-side differences. Distances of >25% to 50% compared with the unaffected side have been shown to be diagnostic for a complete CC ligament disruption (3).
that the mean distance between the superior border of the coracoid and the inferior border of the clavicle was 1.1 to 1.3 cm. As this distance will vary between patients and radiographic techniques, it is necessary to compare side-to-side differences. Distances of >25% to 50% compared with the unaffected side have been shown to be diagnostic for a complete CC ligament disruption (3).
The axillary view, although not specific, can be helpful in type IV injuries in which the clavicle is posteriorly displaced. In addition, the cross-arm view can illuminate the degree of injury by accentuating the displacement of the clavicle (4) (Fig. 4.2). Although classically described and often cited in the evaluation of AC joint injuries, weighted stress radiographs are no longer thought to be the gold standard and have been largely superseded by bilateral Zanca views.
Classification of AC Joint Injury
Most AC joint injuries are the consequence of a force directed inferiorly at the acromion with the arm adducted. This motion forces the entire shoulder girdle down. During the initial motion, the AC joint remains congruent. However, the clavicle eventually impacts the first rib, inhibiting further inferior translation. The clavicle will either fracture, with the first rib acting as a fulcrum, or the AC ligament complex will sequentially fail.
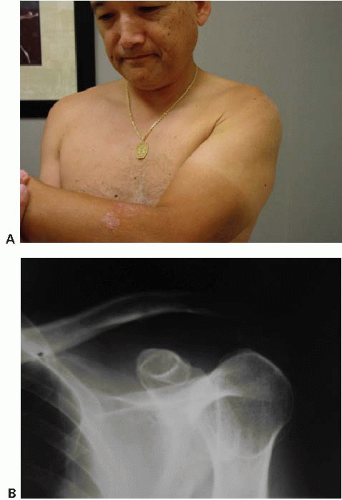 FIGURE 4.2. A: Clinical photograph of a cross-chest adduction view. B: Radiograph demonstrating the accentuated displacement of the clavicle. |
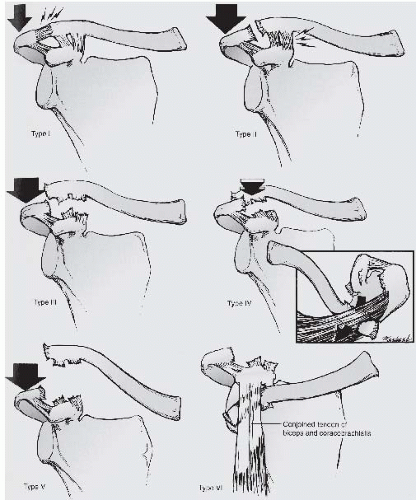
Although first recognized by Hippocrates (5), it was not until 1917 when the first description of the sequential failure of the AC joint complex was published by Cadenat (6). Tossy (7) later proposed a classification scheme including three degrees of injury ranging from type I injuries, which represent a sprain of the AC ligaments, to type III with complete disruption and separation of the clavicle and scapula. Rockwood et al. (3) expanded Tossy’s classification, adding three additional injury grades for a total of six.
Rockwood’s classification (Fig. 4.3) begins with a minimal injury to the AC joint proper. This injury pattern, type I, represents a sprain of the joint capsule and surrounding ligaments without displacement. In a type II injury, the AC joint capsule and surrounding ligaments are disrupted but without significant elevation of the clavicle, usually <50%. The coracoclavicular (CC) ligaments are intact preventing superior displacement but increased anterior-posterior translation will often be apparent. With further significant force a type III injury occurs. The AC ligament complex as well as the CC ligament complex rupture resulting in up to 100% displacement of the clavicle relative to the scapula. Type IV injuries, best visualized on axillary radiographs, occur when the clavicle is forced posteriorly through the trapezius and are generally irreducible
on physical exam due to soft-tissue interposition. Type V injuries are secondary to violent force and represent complete soft-tissue disruption of the clavicle from the scapula with up to 300% displacement of the clavicle. This displacement occurs because of the disruption of the deltotrapezial fascia. Finally, the extremely rare type VI injury occurs when the clavicle becomes displaced and entrapped beneath the coracoid or acromion.
on physical exam due to soft-tissue interposition. Type V injuries are secondary to violent force and represent complete soft-tissue disruption of the clavicle from the scapula with up to 300% displacement of the clavicle. This displacement occurs because of the disruption of the deltotrapezial fascia. Finally, the extremely rare type VI injury occurs when the clavicle becomes displaced and entrapped beneath the coracoid or acromion.
TREATMENT
Nonoperative Treatment Considerations
Lesser grade AC joint injuries, types I and II, can be treated successfully nonoperatively and conservative care is the mainstay of management. Various regimes have been used effectively. Initial immobilization with a sling for comfort followed by unrestricted use and symptomatic pain relief usually affords excellent results. Use of a corticosteroid and anesthetic preparation for high demand patients or athletes may speed recovery. If symptoms persist despite extensive conservative care, an arthroscopic distal clavicle resection of no more than 8 to 10 mm is appropriate. Conversely, treatment strategies for types IV, V, and VI almost always include surgical intervention. Patients with these injury types will often suffer significant morbidity if left untreated, and an AC stabilization procedure is generally indicated.
The controversy lies in the treatment for type III injuries. At the onset, these injuries can be debilitating and painful with a cosmetic deformity that may be unacceptable to patients. However, many patients will do well with conservative care and return to near normal function despite persistent deformity. The general consensus currently is to treat most type III injuries initially conservatively and surgery is reserved for recalcitrant cases that remain persistently symptomatic beyond 3 months (8, 9 and 10).
Operative Indications for Surgical Reconstruction
Hundreds of techniques have been proposed to stabilize or reconstruct the AC joint. Many have proven inadequate or physiologically unsound. AC joint separations that are considered for surgery are usually divided into acute and chronic categories, with approximately 6 weeks defining the two. As our understanding of the biomechanics and surgical techniques has improved, that distinction has become increasingly less defined. For the purpose of simplicity, however, we will maintain that division between acute and chronic injuries.
If an acute injury is determined to be best managed surgically, the use of an AC joint stabilization technique such as a Bosworth screw, suture or wire cerclage, K-wire fixation or ultrastrong suture pulley system is favored (11). For chronic cases, it is necessary to utilize a soft-tissue graft, preferably a free graft, along with a synthetic backup to reconstruct the AC joint complex. Although the Weaver-Dunn procedure has been traditionally recommended to reconstruct chronic AC joint separations, recent studies have demonstrated that the transferred coracoacromial ligament has a quarter of the strength of the native CC complex. Moreover, even with modern surgical techniques, failures with the Weaver-Dunn procedure have been reported in up to 50% of patients (12, 13).
Special Anatomic and Motion Considerations
The AC joint is more than just a link between two bones. It provides for a complex articulation and multiplanar motion between the axial and appendicular skeleton. Appreciating the complex anatomy and motion of the joint is the key to a satisfactory reconstruction.
The AC joint is usually described as an arthrodial joint linking the distal clavicle to the medial border of the acromion of the scapula. The components of this joint consist of the AC capsular ligaments (anterior, posterior, superior, and inferior), the articular disk and the synovial membrane. The CC ligaments as detailed in Grey’s Anatomy are usually described in conjunction with the AC joint since “they form a most efficient means of retaining the clavicle in contact with the acromion.” The CC ligaments consist of two fasciculi, named for their particular geometric shapes: the conoid and the trapezoid. The term AC joint complex is used when referring to both the AC joint proper and the CC ligaments.
Each end of the AC joint is surfaced with hyaline cartilage surrounded by a synovial membrane. Interposed is a meniscal type of fibrocartilage disk. The size, shape, and presence of the meniscus are highly variable and often absent. Its particular function is not clear as it seems to degenerate with age (14, 15 and 16).
The capsular ligaments of the AC joint proper consist of the anterior, posterior, superior, and inferior capsular thickenings and are the primary horizontal stabilizers of the AC joint. Serial sectioning of the AC joint ligaments have shown that the superior and posterior ligaments contribute 56% and 25% of the resistance to posterior translation, respectively (17). Therefore, when performing an arthroscopic distal clavicle resection, care should be taken to maintain the superior and posterior capsule of the AC joint to avoid the painful complication of the posterior clavicle impinging on the spine of the scapula.
Although not part of the AC joint proper, the CC ligament complex with its two bundles contributes greatly to the inherent stability of the articulation (18). Historically, and despite its importance in AC joint stability, the CC ligament has received little in the way of an anatomic description. Improved surgical interventions may be realized through a better understanding of that particular anatomy.
Each ligament bundle assumes the shape of its namesake (Fig. 4.4). Both originate from the coracoid process and insert on the clavicle. The trapezoid ligament is a thin, quadrilateral ribbon-like structure that has a linear origin and insertion both on the coracoid and the clavicle.
The coracoid attachment is along the medial border of the “tubercle of Naples,” sometimes referred to as the coracoid “knuckle.” The tubercle lies just lateral to the scapular notch. The broad width of the trapezoid then wraps over the superior surface of the coracoid in a 45° angle to insert laterally on the clavicle. The clavicular insertion is oriented obliquely in the sagittal plane with its anterior border free and posterior border joining the conoid ligament in an orthogonal orientation, analogous to two contiguous walls of a box.
The coracoid attachment is along the medial border of the “tubercle of Naples,” sometimes referred to as the coracoid “knuckle.” The tubercle lies just lateral to the scapular notch. The broad width of the trapezoid then wraps over the superior surface of the coracoid in a 45° angle to insert laterally on the clavicle. The clavicular insertion is oriented obliquely in the sagittal plane with its anterior border free and posterior border joining the conoid ligament in an orthogonal orientation, analogous to two contiguous walls of a box.
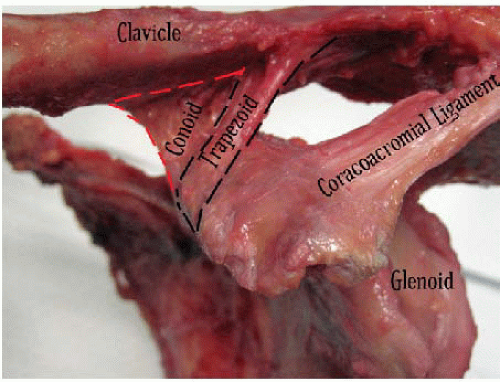 FIGURE 4.4. Cadaver dissection of the coracoclavicular ligaments. Note that the conoid lies in the coronal plane, whereas the trapezoid lies in the sagittal plane
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|