Abductor Muscle and Greater Trochanteric Complications
James I. Huddleston III., Jeffrey A. Geller, Dennis W. Burke and Henrik Malchau
Key Points
Introduction
Sir John Charnley strongly advocated for osteotomy of the great trochanter in primary total hip arthroplasty (THA) to optimize soft tissue tensioning and stability.1,2 The advent of modularity in modern THA systems has enhanced surgeons’ ability to restore offset and leg length, as well as to optimize fixation without osteotomizing the greater trochanter. As a result, most contemporary hip surgeons do not routinely use the transtrochanteric approach for uncomplicated primary total hip arthroplasties. Nevertheless, trochanteric osteotomy remains a valuable technique for revision surgery, as well as in primary cases involving severe protrusio acetabuli, ankylosis of the hip joint, heterotopic ossification, femoral deformity associated with dysplasia, and severe periarticular scar.3–8
Management of complications associated with the abductor mechanism in total hip arthroplasty can be challenging. These complications are not uncommon and may have a significant impact on a patient’s functional status. This chapter reviews the complications associated with osteotomy and fracture of the greater trochanter as well as nerve palsy, avulsion and bursitis of the abducture musculature. Treatment options and results of techniques used to address these complications are discussed as well. Last, the authors present a novel technique for treating tendinous avulsion that has shown early success.
Bony Complications
Nonunion
Nonunion rates of the osteotomized greater trochanter vary and depend on the method of fixation.9 Numerous first-generation techniques that used stainless steel and cobalt-chrome alloy monofilament wires demonstrated nonunion rates of 0 to 7.9% in studies that ranged in size from 75 to 1162 patients.10–16 Risk factors for the development of nonunion when wires alone were used include male gender, revision surgery, and a primary diagnosis of rheumatoid arthritis. Technical factors that may predispose to nonunion with this technique include small size of the osteotomy fragment, lack of sufficient wire tension, limited surgical experience, wires placed around the lesser trochanter, and apposition of the trochanter to a bed that is primarily cement.12,17,18 The need for revision surgery, an antalgic gait, pain, femoral loosening, and lower Charnley hip scores have all been associated with nonunion of the greater trochanter.16 The development of nonunion after greater trochanteric osteotomy has not been associated with the type of wiring technique or the osteotomy variant used.19,20 The rate of wire breakage based on a meta-analysis of studies reported from 1978 to 1993 involving 2910 total hip arthroplasties is 22% with various wiring techniques.10–12,18,20–22
In 1977, Dall and Miles introduced multifilament cables as the second-generation fixation technique for greater trochanter osteotomy.23 The major advantages of cables over wires are that they offer greater strength and greater compression at the osteotomy site, while providing greater resistance to deformation.18,24-31 Despite improvement in mechanical properties, breakage rates for cables have been reported to be as high as 12% (20/160 hips).22 The use of cables alone in the practice of modern total hip arthroplasty is generally reserved for fixation of extended trochanteric osteotomies (Fig. 103-1). Cables may produce wear debris from micromotion that occurs between filaments, and this debris has been implicated in third-body wear of the bearing surface, which can affect rates of component loosening.32,33
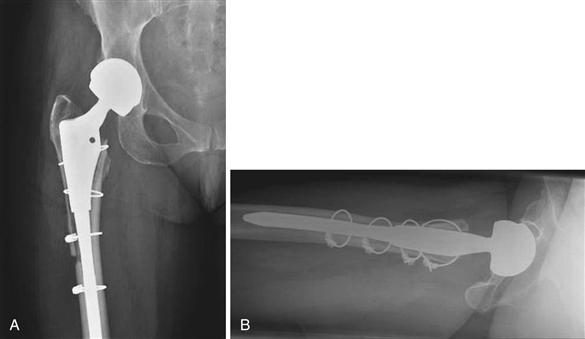
Figure 103-1 A, Anteroposterior (AP) and (B) lateral radiographs show an extended trochanteric osteotomy that united with multifilament cables alone.
Cable grip systems were introduced to address the shortcomings of wires and cables alone for trochanteric fixation (Fig. 103-2). In 1983, Dall and Miles reported that their new cable grip device was better at capturing the trochanter and prevent trochanteric escape.23 When compared with wires and cables alone, cable grip systems have been shown to withstand 1.5 times the load to failure and require 2 to 2.5 times the load needed to produce 2-cm of trochanteric displacement.27 Nonunion rates with use of a cable grip system in four series vary from 0.9% to 38% in series ranging in size from 40 to 321 hips.23,24,28,30

Figure 103-2 Anteroposterior (AP) hip radiograph shows nonunion of an osteotomized greater trochanter fixed with a Dall-Miles cable grip system.
Fourth-generation trochanteric fixation implants comprise locking plates that allow for adjuvant cable and/or wire fixation (Fig. 103-3). The ability to extend the length of the construct and retighten the cables is a major advantage of these systems. Early clinical results reported for these constructs are promising. One study of 42 patients reported significantly lower incidences of cable breakage (P < .025) and trochanteric nonunion (P < .05) with a 4th generation cable plate when compared with wires and cables alone.34 A more recent study of four cases describes healing of the fracture or osteotomy with full abductor function and significant improvement in hip scores in all four patients at a minimum of 20 months’ follow-up.35

Figure 103-3 Anteroposterior (AP) hip radiograph shows an ununited extended trochanteric osteotomy despite use of a long cable-plate system.
The extended trochanteric osteotomy (ETO) was first described by Wagner36 in 1989 and has been modified and popularized by Paprosky and associates.37 Wagner’s osteotomy is performed in the coronal plane, whereas Paprosky’s is a sagittal plane osteotomy. It is most commonly used in revision surgery for removal of well-fixed implants and/or polymethylmethacrylate, although the ability to correct femoral deformity, improve exposure, and potentially improve the accuracy of femoral canal preparations are additional potential benefits. Complications associated with this technique include fracture, malunion, and nonunion. The incidence of ETO nonunion has been reported to be significantly lower when compared with sliding and traditional trochanteric osteotomies.3,38 In one series of 192 consecutive revision THAs, in which an ETO was used for improved exposure, the authors reported two cases of nonunion (1.2%) and one case of malunion (0.6%) among 166 patients at a minimum of 2 years’ follow-up.8 In another series, the rate of ETO nonunion was 1.4% (1/74). Five of 73 ETOs united with less than 5 mm of migration, and 68 ETOs united with no migration.39
Clinical manifestations of trochanteric escape include pain, limp, and reduced abductor strength. Trochanteric migration of 5 to 20 mm has been shown to lead to nonunion and may be associated with development of a Trendelenburg gait pattern.11,27 Displacement greater than 2 cm has been shown to lead to significant abductor weakness.40
Early detection of postoperative trochanteric problems is important to optimize chances of successful treatment. The presence of broken hardware or fragment migration seen on postoperative radiographs is cause for concern, although broken hardware is not pathognomonic for nonunion. Relative indications for revision of the fixation include migration during the first 6 weeks postoperatively, symptomatic nonunion, and symptomatic broken wires, cables, or plates. During revision surgery, all fibrous tissue should be débrided, and bleeding at the bony edges should be ensured when possible. Postoperatively, patients should be placed on trochanteric precautions to include no active abduction and toe touch weight bearing for at least 8 weeks and up to 3 months. Use of a hip abduction orthosis should also be considered.
Instability is a dreaded complication associated with nonunion of an osteotomized greater trochanter. The mechanism is often due to a decrease in abductor tension across the hip41 but also may be due to trochanteric impingement against the pelvis anteriorly. Although some authors have reported a higher dislocation rate with nonunion, others have not.42 In a series of 8944 THAs performed via a transtrochanteric approach, Woo and Morrey reported a nonunion rate of 2.2% (194 patients). Most dislocations that they observed occurred in patients who experienced trochanteric migration greater than 2 cm. The dislocation rate was 17.6% in patients with trochanteric nonunion and 2.8% in patients with trochanteric union.43,44 Although decreased abductor power from nonunion is clearly a contributing factor to instability, component malposition should also be considered.
The use of trochanteric advancement to treat instability is less common today owing to modularity that allows for optimization of leg lengths and femoral offset. If trochanteric advancement is used, the technique described by Chin and Brick, in which the abductors are released from their origins on the outer iliac wing through a separate incision on the iliac crest, may be helpful to gain additional length, thereby decreasing tension on the repair.45
Heterotopic Ossification
It is unclear whether heterotopic ossification (HO) is more common with trochanteric osteotomy.46 After primary THA, one study failed to show a difference in rates of HO among three approaches (posterior, transtrochanteric, and anterolateral).47 With use of the transtrochanteric approach in routine THA, the rate of HO has been reported at 7% in 1500 low-friction arthroplasties performed by Eftekar.48 A rate of 90% has been reported when the transtrochanteric approach was used for complicated primary and revision THAs.49 It is generally accepted that the risk of HO is higher in patients with hypertrophic osteoarthritis, ankylosing spondylitis, closed head injury, or a history of ectopic bone formation. Given this, the surgeon may consider HO prophylaxis in select high-risk cases.
Fracture
It is estimated that periprosthetic fractures occur intraoperatively in approximately 1% to 20% of primary THA cases.50–55 The incidence of isolated greater trochanter fractures is unknown and has been estimated to be as high as 5%.56 In a series of primary total hip arthroplasties performed through an anterior approach, the rate of intraoperative greater trochanter fracture was 0.7% (3/437 THAs).57 The rate of postoperative greater trochanter fractures is unknown. It has been estimated that postoperative periprosthetic femoral fractures occur in less than 1% of primary total hip arthroplasties.58 Intraoperative fractures should be treated with reduction and internal fixation. Given the relatively high rates of nonunion associated with the use of wires and cables alone, we advocate the use of a cable-plate system. Postoperative greater trochanter fractures with less than 2 cm of displacement have been successfully treated without operative intervention and with 6 to 12 weeks of limited weight bearing and no active abduction exercises until the fracture has united.56 It is recommended that most fractures with more than 2 cm of displacement be treated with open reduction and internal fixation, if adequate fixation is likely to be achieved.
Soft Tissue Complications
Bursitis
The prevalence of trochanteric bursitis after THA ranges from 4% to 17% in series of patients ranging in size from 75 to 1162.59–63 Although the cause of trochanteric bursitis is multifactorial, the final common pathophysiology likely involves repetitive microtrauma, scar tissue formation, alterations in lower extremity biomechanics, and/or changes in hip mechanics after THA.64 Risk factors include a direct lateral approach,60 limb length discrepancy, younger age, and increased lateral offset. Most patients will experience resolution of their symptoms with physical therapy and local corticosteroid injection. In one study, 32 of 689 patients (4.6%) developed trochanteric bursitis after THA. In all, 80% of the 25 patients for whom follow-up was available experienced resolution of their symptoms after corticosteroid injection. A total of 11 of 25 (45%) patients needed multiple injections. The authors commented that nonresponders may benefit from operative treatment to remove trochanteric bursae and local scar tissue.59
Trochanteric bursitis after THA is more common in the setting of trochanteric hardware because these devices can easily cause local soft tissue irritation, given that they reside near a bony prominence. Unfortunately, relief of symptoms after removal of hardware is less predictable than desired. In a series of 36 patients with trochanteric bursitis reported by Bernard and Brooks, less than 50% of patients who underwent removal of trochanteric wires reported successful pain relief.31 Treatment modalities other than hardware removal include stretching, ultrasound, and injections of local anesthetic and corticosteroids.
Nerve Injury
Peripheral nerve injury occurs in 0 to 3% of primary THAs65–68 and in 2.9% to 7.6% of revision THAs.65,66,69 The incidence of superior gluteal nerve injury is, however, unknown. Injuries of the superior gluteal nerve can lead to abductor weakness with resultant limp or instability. Splitting of the gluteus medius muscle greater than 5 cm from the tip of the greater trochanter is considered a risk factor for injury to the superior gluteal nerve. This is a concern when the lateral approach to the hip is utilized.41,60,70
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








