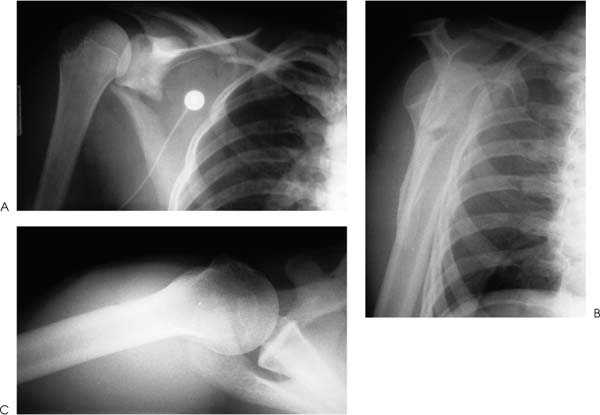
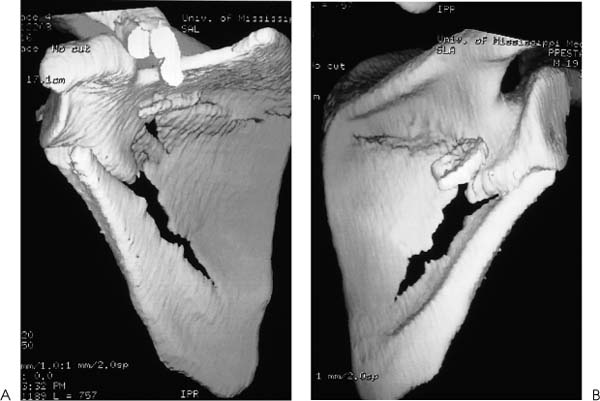
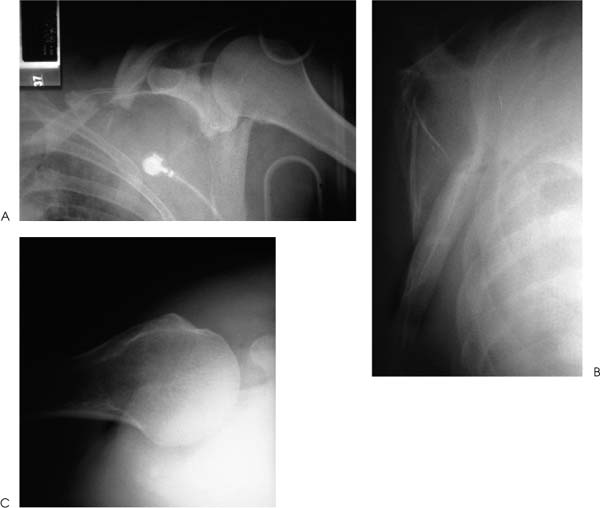
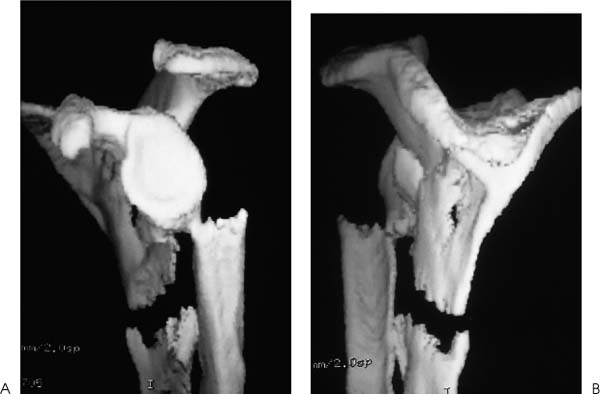
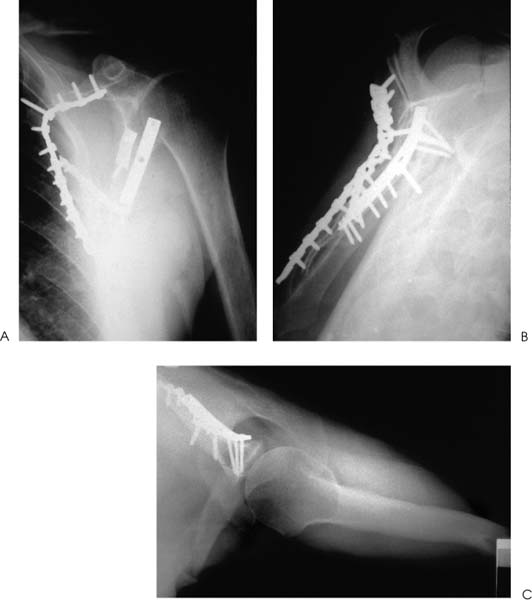
Case 8 A 31-year-old man presents several hours after a motor vehicle collision in which he was thrown from the car after veering off the road. He complains of shoulder and chest wall pain. He denies any numbness or other complaints. Range of motion of the shoulder demonstrates 90 degrees of passive forward flexion and 20 degrees of active forward flexion with severe pain. He has mildly limited passive external rotation and internal rotation and is neurovascularly intact in the upper extremity. Palpation of the shoulder, shoulder blade, and clavicle demonstrates moderate swelling and tenderness. Ecchymosis is noted in the area of the scapula clavicle and ribs. Figure 8–1. Anteroposterior (AP) (A), scapular Y (B), and axillary (C) views of the shoulder are demonstrated. 1. Proximal humerus fracture 2. Scapular fracture 3. Rotator cuff contusion 4. Clavicle fracture 5. Scapula and clavicle fratcure An anteroposterior (AP), scapular Y view, and axillary view of the shoulder are obtained (Fig. 8–1). Extraarticular Scapular Fracture and Clavicle Fracture. Periscapular ecchymosis and swelling suggest fracture. Radiographs confirm an extraarticular fracture of the scapula. A midshaft clavicle fracture and multiple rib fractures are also demonstrated. Significant displacement is seen radiographically. The AP radiographic view best demonstrates the scapular body fracture in this patient. The scapular Y view and axillary view are not as helpful in visualizing the fracture, emphasizing the importance of multiple views in patients with shoulder trauma. Careful neurovascular assessment is important in these injuries. Scapular body fractures generally result from high-energy injuries, such as motor vehicle accidents as in the case presented here. Rib fractures, chest injuries, clavicle fractures, and neck injuries occur commonly in association with scapular body fractures. Direct violence and sudden contraction of divergent muscles may cause fractures of the body of the scapula. Of all scapular fractures, body fractures have the highest incidence of associated injury. These fractures may be highly comminuted and markedly displaced. A three-dimensional computed tomography (CT) reconstruction of the fracture demonstrates nicely the medialization of the glenoid with impingement of the lateral border of the scapula on the joint capsule area (Fig. 8–2). Figure 8–2. Medial-lateral (A) and lateral-medial (B) CT scanning demonstrates the significant medialization of the glenoid and impingement of the lateral border of the scapula on the joint capsule area. (Radiographs and CT scans courtesy of Peter A. Cole, M.D., Jackson, Mississippi.) Treatment of extraarticular scapular body and glenoid neck fractures is usually non-operative. Most extraarticular scapular fractures treated symptomatically, followed by progressive range of motion and strengthening exercises, generally obtain good functional status. However, some residual loss of motion or weakness may persist, and this potential for functional loss should be discussed with the patient at the initiation of treatment. Exceptions to the rule for nonoperative treatment of extraarticular fractures do exist. When a glenoid neck fracture occurs in association with a displaced and unstable clavicle fracture, the glenoid becomes destabilized. Open reduction and internal fixation of the scapula should be carried out as in the patient presented in this case (Fig. 8–3). Another exception to nonoperative treatment for extraarticular glenoid body fractures includes those glenoid body fractures with moderate to severe translational or angulatory displacement, particularly when it occurs along with a clavicle fracture (Fig. 8–4). General guidelines for the operative treatment of glenoid neck fractures with significant malposition include translational displacement greater than or equal to 1 cm and/or angulatory displacement greater than or equal to 40 degrees in either the transverse or the coronal plane. Figure 8–3. AP (A), scapular Y (B), and axillary (C) views of the scapula demonstrate open reduction and internal fixation using AO plates and screws. CT scanning is usually necessary to define the degree of translational or angula-tory displacement (Fig. 8–5). If surgical management is indicated, the glenoid neck is approached posteriorly. The interval between the infraspinatus and teres minor muscles is developed to gain access to the inferior glenoid process and the lateral scapular border. After reduction of the fracture, fixation is generally achieved with a 3.5-mm contoured reconstruction plate or plates (Fig. 8–6). Figure 8–4. AP (A), scapular Y (B), and axillary (C) radiographic views demonstrate a fracture of the glenoid body with transitional and angulatory deformity. Figure 8–5. Anterior (A) and posterior (B) CT scanning three-dimensional reconstructions help to better define fracture fragment displacement and orientation. Figure 8–6. AP (A), scapular Y (B), and axillary (C) radiographic views demonstrating fracture fixation of this displaced fracture. PEARLS • CT scanning is the key to accurately diagnosing the translational and angulatory displacement of glenoid neck fractures. • Glenoid neck fractures occurring in association with displaced clavicle fractures may be adequately stabilized by open reduction and internal fixation of the clavicle only, without exposure and fixation of the glenoid body itself.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree