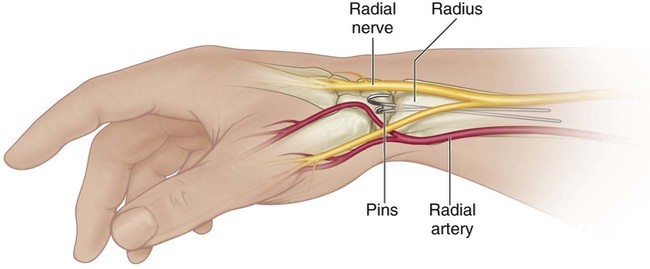
• Completely displaced fractures have 60–80% rate of redisplacement after incomplete reduction. • Following redisplacement, outcomes and complications are similar with re-reduction and casting vs. re-reduction and pin fixation. • Pin fixation reduces the incidence of remanipulation but caries concomitant risks for infection, neurovascular injury, and general anesthesia. • Consider pin fixation if re-reduction is unstable or incomplete. • The DSBRN pierces the brachioradialis (BR) and emerges between the extensor carpi radialis longus and brevis 8 cm proximal to the radial styloid. • It then crosses over the extensor retinaculum before dividing into medial and lateral branches. • It lies dorsal to proper pin position (Fig. 2).
Closed Reduction and Pinning of Distal Radius Fractures
Indications
 Unstable distal radius fracture unable to be controlled by cast alone
Unstable distal radius fracture unable to be controlled by cast alone
 Displaced distal radius fracture that is in unacceptable alignment following a reduction and casting maneuver
Displaced distal radius fracture that is in unacceptable alignment following a reduction and casting maneuver
 Redisplacement following a previous reduction and casting maneuver
Redisplacement following a previous reduction and casting maneuver
 Other consideration that may preclude circumferential cast immobilization:
Other consideration that may preclude circumferential cast immobilization:
 For distal radial physeal fractures, multiple reduction attempts or repeated late reduction attempts should be avoided. If reduction remains unacceptable, consider allowing the fracture to heal and observing the deformity over time, proceeding with late corrective osteotomy if remodeling does not occur.
For distal radial physeal fractures, multiple reduction attempts or repeated late reduction attempts should be avoided. If reduction remains unacceptable, consider allowing the fracture to heal and observing the deformity over time, proceeding with late corrective osteotomy if remodeling does not occur.
 Distal ulnar fractures often accompany distal radial fractures. Acceptable alignment for distal ulnar fractures includes up to 50% translation and 20° of angulation.
Distal ulnar fractures often accompany distal radial fractures. Acceptable alignment for distal ulnar fractures includes up to 50% translation and 20° of angulation.
Surgical Anatomy
 Dorsal sensory branch of the radial nerve (DSBRN)
Dorsal sensory branch of the radial nerve (DSBRN)
Portals/Exposures
 Pins are placed using a “nick-and-spread” technique.
Pins are placed using a “nick-and-spread” technique.
 For physeal fractures or fractures near the physis, the pin entry site is through the radial styloid (Fig. 4A).
For physeal fractures or fractures near the physis, the pin entry site is through the radial styloid (Fig. 4A).
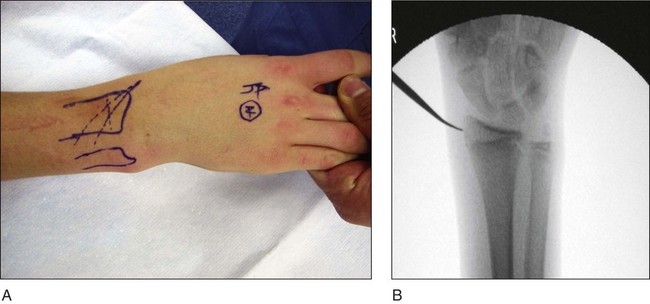
 For more proximal metaphyseal fractures, the pin entry site is started just proximal to the distal radial physis to avoid placing pins across the physis.
For more proximal metaphyseal fractures, the pin entry site is started just proximal to the distal radial physis to avoid placing pins across the physis.
8: Closed Reduction and Pinning of Distal Radius Fractures