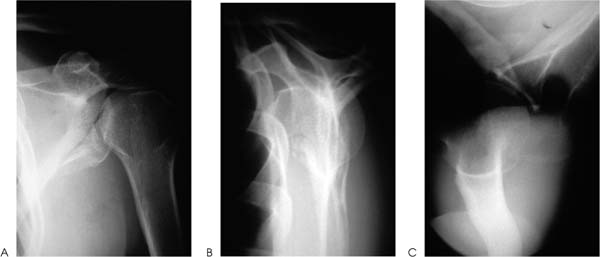
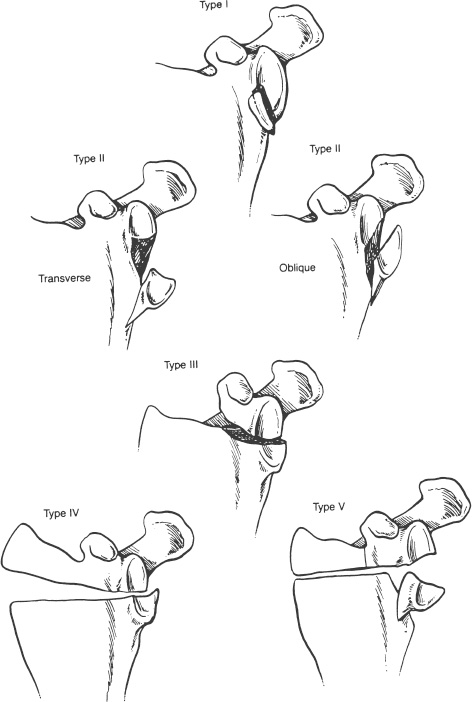
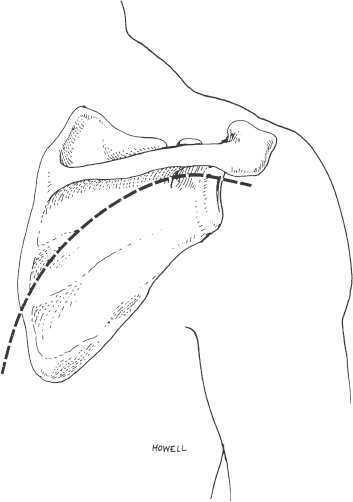
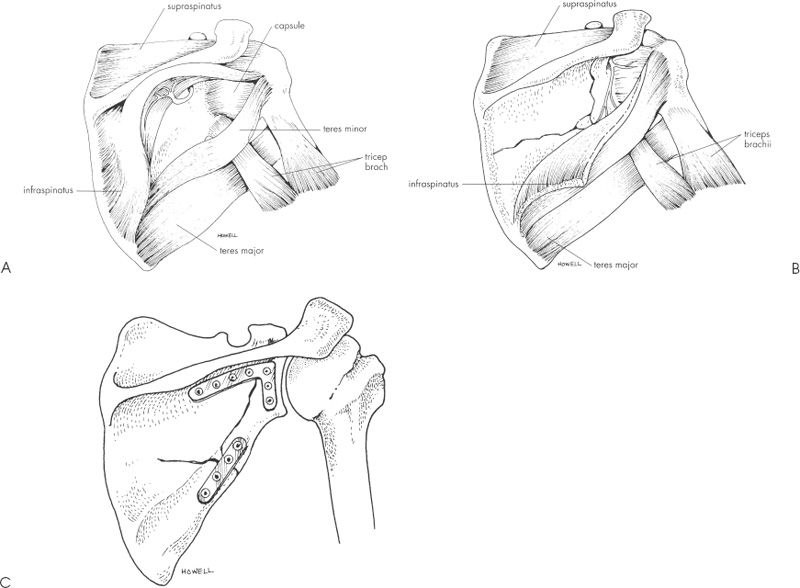
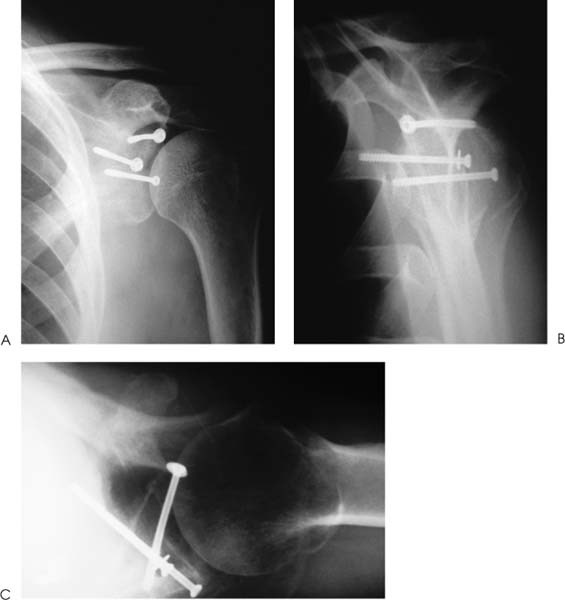
Case 7 A 23-year-old, unrestrained, male passenger presents to the emergency room several hours after a motor vehicle accident. He presents with a number of abrasions about his chest and shoulder girdle. He has a contralateral, closed midshaft femur fracture. He complains of left thigh and leg pain as well as right shoulder pain. He denies any numbness of his right upper extremity. He has no neck or chest complaints. Evaluation demonstrates moderate swelling about the shoulder and shoulder girdle. He is tender to palpation and there are a number of abrasions along the anterior and lateral aspect of his shoulder. He is neurovascularly intact. Passive range of motion of the shoulder includes forward flexion of 90 degrees, external rotation of 40 degrees, and internal rotation of 60 degrees. Stability testing is difficult secondary to pain and swelling, but appears to be grossly normal. Crepitation is also appreciated through a range of motion of the shoulder. Figure 7–1. Anteroposterior (AP) (A), scapular Y (B), and axillary (C) radiographs of the affected shoulder. 1. Proximal humerus fracture 2. Scapular fracture 3. Rotator cuff tear 4. Shoulder dislocation An anteroposterior (AP), scapular Y view, and axillary view of the shoulder are obtained (Fig. 7–1). Management of intraarticular glenoid fractures depends primarily on the degree of displacement of the articular surface. Ideberg classified intraarticular glenoid fractures, providing helpful insights into the best method of treatment (Fig. 7–2). The glenoid fracture presented in this case can be best classified as a type II according to Ideberg’s classification. A significant amount of displacement is seen in this young patient. Open reduction and internal fixation was preferred by the authors in this case. Figure 7–2. Ideberg’s classification of intraarticular fractures of the glenoid. (From Rockwood C Jr., et al. Fractures in Adults. Philadelphia: Lippincott-Raven Publishers, 1996, p. 1176, Fig. 18–21. With permission of Lippincott-Raven Publishers.) Displaced, intraarticular fractures of the glenoid are usually best approached posteriorly. An oblique posterior incision is made (Fig. 7–3). Patient positioning is important, and either the lateral decubitus position or the prone position is acceptable. However, prone positioning precludes the use of an additional anterior approach if required. Following dissection of the subcutaneous tissues and exposure of the deltoid, the deltoid is released from the scapular spine. The infraspinatus tendon and the posterior part of the capsule of the glenohumeral joint are incised 1 cm medial to the greater tuberosity. This muscular and capsular flap is then retracted to expose the glenohumeral joint. A Fukuda retractor can be placed into the joint posteriorly to allow for visualization of the glenoid articulation. The interval between the infraspinatus and teres minor can then be identified and developed to gain access to the posterior and inferior aspects of the glenoid cavity, and lateral border of the scapula. Depending on the classification of the intraarticular glenoid fracture, exposure of the scapular body may or may not be necessary. Fracture fragment stabilization can be accomplished using a variety of screws and plates, depending on the clinical situation. The glenoid cavity can also be approached posterosuperiorly. The incision used for the posterior approach is extended over the superolateral aspect of the shoulder. The glenoid fossa can be exposed as described for the posterior approach. The interval between the clavicle and the scapular spine can be developed. The trapezius muscle and underlying supraspinatus tendon can be split in line with their fibers to expose the superior aspect of the glenoid cavity and the base of the coracoid process. A portion of the posterior clavicle can sometimes be removed to aid in exposure. Both the posterior approach and the posterosuperior approach place the suprascapular nerve in jeopardy as the nerve passes through the suprascapular notch, the supraspinatus muscle, the spinoglenoid interval, and the infraspinatus muscle. The axillary nerve and posterior humeral circumflex artery are also at risk with this approach. Figure 7–3. An oblique incision to the scapular body and neck is made. (From Hawkins RJ, et al. Atlas of Shoulder Surgery. New York: Mosby-Year Book, 1996, p. 220, Fig. 7–35. With permission.) Fixation of the glenoid fracture is accomplished with screw and plate fixation, but knowledge of the areas of the scapula that will accept screws is important. Four regions of substantial bone are available: the scapular neck, the coracoid process, the base of the scapular spine, and the lateral border of the scapular body. Fixation can be achieved with interfragmentary compression screws, 3.5-mm reconstruction plates, and Kirschner wires as necessary. The choice of implants depends on the fracture pattern and the available bone stock. The key to achieving a successful result is the realignment of the glenoid articulating surface (Fig. 7–4). The patient represented here had successful fracture fixation using this approach (Fig. 7–5). Figure 7–4. Posterior approach to the glenoid and scapular neck and body. (A) Following release and retraction of the deltoid posteriorly, the infraspinatus and capsule can be released or split to expose the glenoid neck and scapular body. Care must be taken to identify and protect the suprascapular nerve. (B) Alternatively, the infraspinatus muscle can be subperiosteally elevated from the infraspinatus fossa to expose the body and neck of the scapula. Again, suprascapular nerve identification and protection is important. (C) Fracture stability can be achieved using a number of implants. (From Hawkins R, et al. Atlas of the Shoulder Surgery. New York: Mosby-Year Book, 1996, pp. 221–223, Figs. 7–37, 7–39, 7–40. With permission.) Figure 7–5. Postoperative AP (A), scapular Y (B), and axillary (C) radiographs demonstrating fracture fixation of this intraarticular glenoid fracture. Postoperative rehabilitation depends on the stability achieved at the time of surgery. Generally, excellent stability is achieved with scapular fracture fixation and early motion is allowed. Protection of any released tendinous structures is important in the early postoperative phase, but by 4 weeks postoperatively few limitations are required. Ideberg classified intraarticular glenoid fractures into several types. Treatment of these fractures depends on the displacement and articular step-off at the glenoid. When significant displacement is present, particularly in a younger adult, open reduction and internal fixation is preferred by the authors. A posterior approach is generally used for intraarticular glenoid fractures, as the fracture fragments are more easily reduced and stabilized from a posterior approach. PEARLS • CT scanning is a variable adjunct to the treatment of these intraarticular injuries. The amount of articular step-off is easily demonstrated. • Serial radiographic follow-up is important to ensure that progressive intraarticular displacement does not occur. • Nonoperatively managed patients with intraarticular scapular fractures should undergo early range of motion exercises to help ensure shoulder motion recovery. Prolonged immobilization after these injuries usually results in significant loss of shoulder motion for which recovery is often difficult and prolonged.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Postoperative Management
Discussion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree