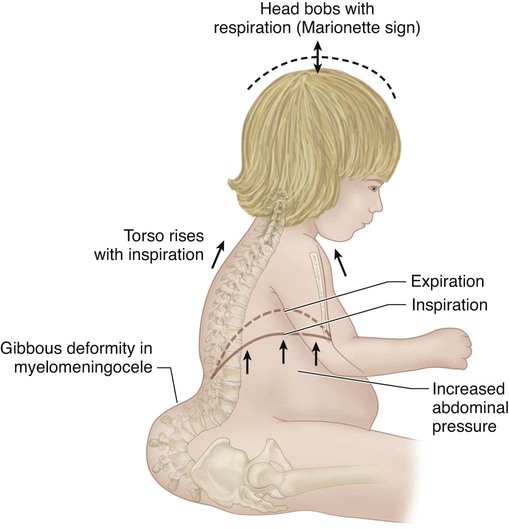
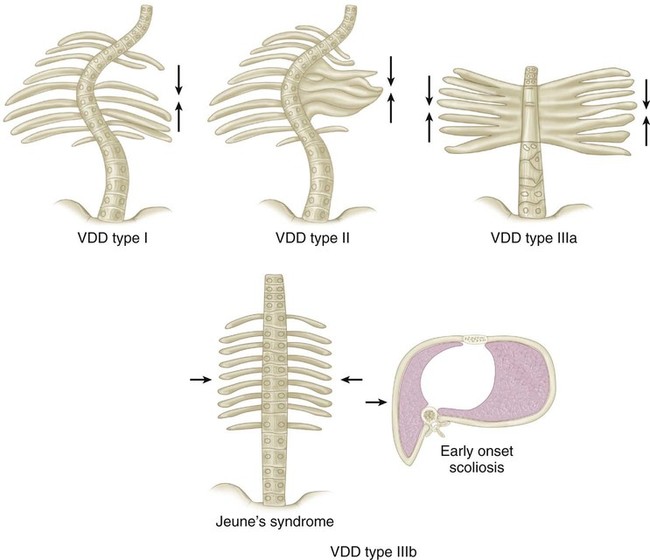
• +0: no assistance, on room air • +1: supplemental oxygen required • +2: nighttime ventilation/continuous positive airway pressure (CPAP) • +3: part time ventilation/CPAP • Normal respiratory rate at birth is 40–80 breaths per minute; that up to age 5 years, 20–40 breaths per minute; and 15–25 breaths per minutes is normal from age 6 to 12 years. Adult values, 15–20 breaths per minute, are reached after 15 years of age (Hoekelman, 1987). • Respiratory rate at rest above these values suggest occult respiratory insufficiency. • The thumb excursion test is performed to clinically measure the ability of each side of the chest to contribute to respiration by rib cage expansion. • The examiner’s hands are placed around the base of the thorax with the thumbs posteriorly pointing upward at equal distances from the spine (Fig. 1). • With respiration, the thumbs move away from the spine symmetrically because of the anterior lateral motion of the chest wall. • Each hemithorax is graded separately: • The concave fused-rib hemithorax often has a +0 thumb excursion test, and if there is significant rib hump deformity of the convex hemithorax, it will also be stiff and also have a +0 thumb excursion test. • This represents a form of secondary thoracic insufficiency syndrome in which the diaphragm, in effect, is doing a pushup against body weight because the “collapsing torso” deformities, such as lumbar kyphosis in myelomeningocele, or severe pelvic obliquity, raise abdominal pressure on the diaphragm by abnormal proximity to the pelvis (Fig. 2) (Campbell and Smith, 2007; Campbell et al., 2003b). • The AP radiograph is analyzed for Cobb’s angle, the interpedicular line ratio, the height of the thoracic spine in centimeters, and the space available for the lung. • The height of the thorax is determined by the radiographic height of the patient’s thoracic spine, and this distance is divided by the normal thoracic spinal height for age, deriving a percentage of normal. • The lateral radiograph defines a loss of sagittal depth of the thorax, due to either pectus excavatum or thoracic spinal lordosis. • The AP and lateral radiographs enable identification of the volume depletion deformities (VDDs) of the thorax in the coronal and sagittal planes of the thorax. • In type I and type II VDDs, windswept deformity of the chest is also common, with severe reduction in transverse volume of the convex hemithorax. Its severity can be defined by measurements of spinal rotation, the posterior hemithorax symmetry ratio, and the thoracic rotation of the CT “scan cut” at the level of maximum deformity. • Both ventilation-perfusion lung scans and 3-mm-cut CT scans with airway reconstruction can define airway compression deformity, if necessary. • The goal of VEPTR surgery is to brace the unstable defect with multiple VEPTRs or use VEPTRs to stabilize ribs transported into the area of defect. • Care must be taken not to damage the lung when the skin incision is over the rib cage defect, and generally there is a large spine defect in the area of the chest wall defect, so care must be taken not to violate the dura in the exposure. • The exposure should cautiously approach the defect area, first proximally, then distally. • Even if gross bony synostosis is not present, longitudinal hemithorax constriction may be present from intercostal muscle scarring, evident on supine lateral bending radiographs when the affected intercostal spaces do not widen while bending into the convex side. • A standard thoracotomy approach would place the spinal cord at risk when this abnormality is present, so the scapula should be cautiously retracted posteriorly and the rhomboid muscles sectioned directly off the edge of the scapula to avoid dural injury. • For the prone position, longitudinal soft rolls are placed under each side of the chest. • A transverse roll is placed under the pelvis. • The patient is immobilized by wide cloth tape padded with hand towels across the buttocks. • The VEPTR expansion thoracoplasty strategy for each VDD of the thorax is different. • In mixed types of VDD, VEPTR surgical treatment should address each individual segment of thoracic deformity with either appropriate longitudinal or lateral expansion of the constricted thorax. • The most common VDD of the thorax is unilateral constriction of the thorax in fused ribs and scoliosis. • The two Freer elevators should touch in the “chopstick” maneuver, to confirm that a continuous soft tissue tunnel has been made.
Vertical Expandable Prosthetic Titanium Rib (VEPTR) Expansion Thoracoplasty
Examination/Imaging
History
 A detailed surgical and respiratory history should be obtained in children with thoracic insufficiency syndrome.
A detailed surgical and respiratory history should be obtained in children with thoracic insufficiency syndrome.
 Onset of clinical deformity, past surgical treatments, and associated morbidities, such as renal, gastrointestinal, central nervous system, and cardiac system abnormalities, must be documented.
Onset of clinical deformity, past surgical treatments, and associated morbidities, such as renal, gastrointestinal, central nervous system, and cardiac system abnormalities, must be documented.
 Past episodes of pneumonia, bronchitis, and asthma attacks or needs for respiratory support during illness should also be documented.
Past episodes of pneumonia, bronchitis, and asthma attacks or needs for respiratory support during illness should also be documented.
Physical Examination
 The child’s ability to respond to pulmonary challenge, such as play activities and running, should be noted. Difficulty in such activities can be a helpful early warning of impending respiratory insufficiency/thoracic insufficiency.
The child’s ability to respond to pulmonary challenge, such as play activities and running, should be noted. Difficulty in such activities can be a helpful early warning of impending respiratory insufficiency/thoracic insufficiency.
 Both the lips and fingertips are examined for any signs of cyanosis and the fingertips for evidence of clubbing, suggesting long-term clinical hypoxia.
Both the lips and fingertips are examined for any signs of cyanosis and the fingertips for evidence of clubbing, suggesting long-term clinical hypoxia.
 If the patient is on oxygen, or dependent on more invasive respiratory support, the degree of respiratory insufficiency should be defined by the assisted ventilator ratings (AVRs) (Campbell and Smith, 2007):
If the patient is on oxygen, or dependent on more invasive respiratory support, the degree of respiratory insufficiency should be defined by the assisted ventilator ratings (AVRs) (Campbell and Smith, 2007):
 The chest is assessed for clinical deformity and the circumference measured at the nipple line and compared to normal values for age to discern percentile of normal (Jones, 1988).
The chest is assessed for clinical deformity and the circumference measured at the nipple line and compared to normal values for age to discern percentile of normal (Jones, 1988).
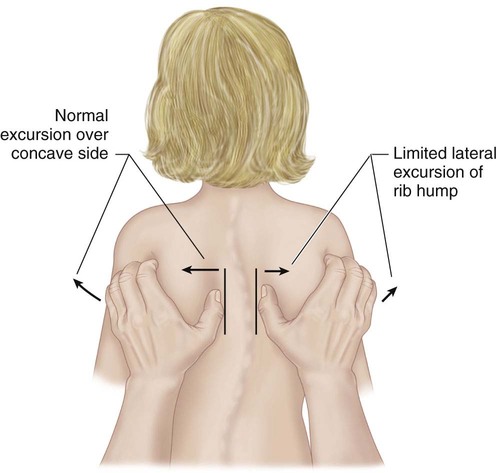
 Greater than 1 cm of excursion of each thumb away from the spine during inspiration is graded as +3, and considered normal.
Greater than 1 cm of excursion of each thumb away from the spine during inspiration is graded as +3, and considered normal.
 0.5–1 cm of excursion is graded +2.
0.5–1 cm of excursion is graded +2.
 Motion up to 0.5 cm is graded as +1.
Motion up to 0.5 cm is graded as +1.
 Assess for a marionette sign: the patient’s head bobs synchronously with respiration.
Assess for a marionette sign: the patient’s head bobs synchronously with respiration.
Imaging Studies
 Weight-bearing anteroposterior (AP) and lateral radiographs of the entire spine, including the chest and pelvis on the same radiograph, are obtained.
Weight-bearing anteroposterior (AP) and lateral radiographs of the entire spine, including the chest and pelvis on the same radiograph, are obtained.
 Computed tomography (CT) scans of the entire chest and lumbar spine are performed at 5-mm intervals, unenhanced, with the scanner set for pediatric dosage to minimize radiation exposure (Campbell and Hell-Vocke, 2003; DiMeglio and Bonnel, 1990; Gollogly et al., 2004a; Gollogly et al., 2004b; Paterson et al., 2001). Usually type I, type II, and type III VDDs have a diminished thoracic volume on CT scan in the coronal plane reconstructions (Fig. 3) (Openshaw et al., 1984).
Computed tomography (CT) scans of the entire chest and lumbar spine are performed at 5-mm intervals, unenhanced, with the scanner set for pediatric dosage to minimize radiation exposure (Campbell and Hell-Vocke, 2003; DiMeglio and Bonnel, 1990; Gollogly et al., 2004a; Gollogly et al., 2004b; Paterson et al., 2001). Usually type I, type II, and type III VDDs have a diminished thoracic volume on CT scan in the coronal plane reconstructions (Fig. 3) (Openshaw et al., 1984).
 CT lung scan volumes can be computed. Full-chest CT scans may be taken at yearly follow-up if percent normal lung volumes are being followed to detect progressive thoracic volume loss.
CT lung scan volumes can be computed. Full-chest CT scans may be taken at yearly follow-up if percent normal lung volumes are being followed to detect progressive thoracic volume loss.
 A more limited CT scan, localized at the level of maximum deformity, may also be followed yearly if CT lung volumes are not thought to be necessary.
A more limited CT scan, localized at the level of maximum deformity, may also be followed yearly if CT lung volumes are not thought to be necessary.
 Magnetic resonance imaging (MRI) studies of the entire spinal cord are obtained to rule out spinal cord abnormalities.
Magnetic resonance imaging (MRI) studies of the entire spinal cord are obtained to rule out spinal cord abnormalities.
 Either ultrasound or fluoroscopy of the diaphragm can be performed to document diaphragmatic function, but dynamic MRI study of the lungs will show great detail of diaphragm and chest wall function (Campbell et al., 2008a).
Either ultrasound or fluoroscopy of the diaphragm can be performed to document diaphragmatic function, but dynamic MRI study of the lungs will show great detail of diaphragm and chest wall function (Campbell et al., 2008a).
 When there is question of early cor pulmonale, echocardiograms are performed to detect tricuspid valve regurgitation.
When there is question of early cor pulmonale, echocardiograms are performed to detect tricuspid valve regurgitation.
Pulmonary Function Studies
 Routine spirometry pulmonary function studies are feasible for children age 5 years or older, and infant pulmonary function tests can be performed in younger patients, if available.
Routine spirometry pulmonary function studies are feasible for children age 5 years or older, and infant pulmonary function tests can be performed in younger patients, if available.
 When there is spinal deformity present, the overall height of the patient is usually decreased, and care must be taken to use arm span instead of height for normalization of pulmonary function test results.
When there is spinal deformity present, the overall height of the patient is usually decreased, and care must be taken to use arm span instead of height for normalization of pulmonary function test results.
 Pulse oximetry studies are also useful to detect significant amounts of hypoxia. An increase in AVR suggests progressive clinical respiratory insufficiency, and this is a strong indication for treatment.
Pulse oximetry studies are also useful to detect significant amounts of hypoxia. An increase in AVR suggests progressive clinical respiratory insufficiency, and this is a strong indication for treatment.
 Comparison of past pulmonary function tests to current ones would be helpful in determining any deterioration of vital capacity as determined by decreasing percent normal vital capacity.
Comparison of past pulmonary function tests to current ones would be helpful in determining any deterioration of vital capacity as determined by decreasing percent normal vital capacity.
Surgical Anatomy
 Instability of the chest wall is documented on radiographs and CT scans, and degree of paradoxical chest wall motion over the bony defect is confirmed on physical examination (Campbell and Smith, 2003).
Instability of the chest wall is documented on radiographs and CT scans, and degree of paradoxical chest wall motion over the bony defect is confirmed on physical examination (Campbell and Smith, 2003).
 Rib fusion is documented on radiographs and CT scans, and confirmed on physical examination by absence of movement with respiration on the thumb excursion test.
Rib fusion is documented on radiographs and CT scans, and confirmed on physical examination by absence of movement with respiration on the thumb excursion test.
 Widespread dysraphism of the posterior elements is common, and the medial edge of the scapula may lie within the spinal canal itself through the defect, best seen on CT scan transverse sections.
Widespread dysraphism of the posterior elements is common, and the medial edge of the scapula may lie within the spinal canal itself through the defect, best seen on CT scan transverse sections.
 Anomalous insertion of the diaphragm proximally may be seen on radiographs, as evidenced by decreasing volume available for the lung, or the diaphragm may be flail when its border inserts into soft tissue only when ribs are absent distally.
Anomalous insertion of the diaphragm proximally may be seen on radiographs, as evidenced by decreasing volume available for the lung, or the diaphragm may be flail when its border inserts into soft tissue only when ribs are absent distally.
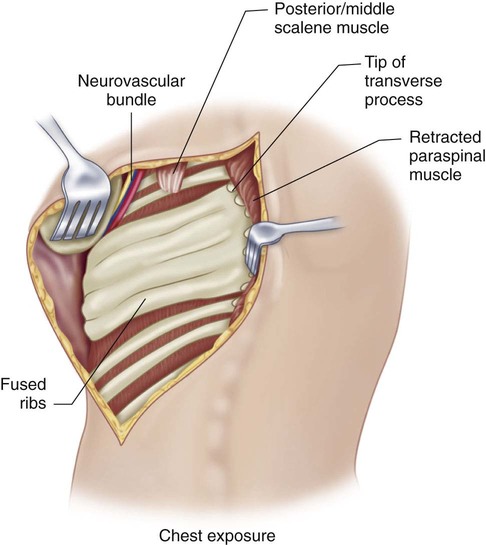
 The brachial plexus may be difficult to locate, but the common insertion of the middle and posterior scalene muscles is a reliable landmark, with the brachial plexus found just anterior to it in the exposure.
The brachial plexus may be difficult to locate, but the common insertion of the middle and posterior scalene muscles is a reliable landmark, with the brachial plexus found just anterior to it in the exposure.
 Stable rib attachment sites for device placement are evaluated on radiographs.
Stable rib attachment sites for device placement are evaluated on radiographs.
Positioning
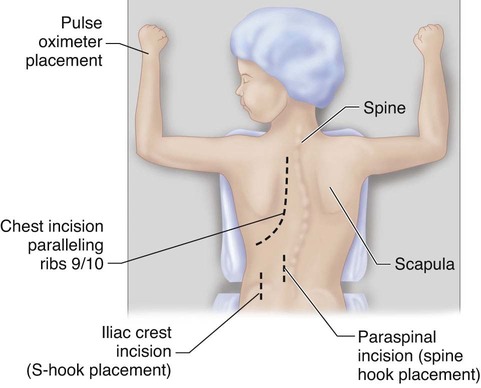
 The prone position is now most commonly used (Fig. 4).
The prone position is now most commonly used (Fig. 4).
 The lateral decubitus position is used in cases of severe scoliosis, with the concave side up, to help correct deformity.
The lateral decubitus position is used in cases of severe scoliosis, with the concave side up, to help correct deformity.
Portals/Exposures
 A modified curvilinear thoracotomy incision is used, extending anteriorly between the ninth and tenth ribs.
A modified curvilinear thoracotomy incision is used, extending anteriorly between the ninth and tenth ribs.
 The trapezius, latissimus, and rhomboid muscles are sectioned in line with the skin incision.
The trapezius, latissimus, and rhomboid muscles are sectioned in line with the skin incision.
 After complete exposure of the rib cage, the paraspinal muscles are next reflected by cautery, lateral to medial, up to the tips of the transverse processes of the spine.
After complete exposure of the rib cage, the paraspinal muscles are next reflected by cautery, lateral to medial, up to the tips of the transverse processes of the spine.
 Care must be taken not to excessively expose the spine in order to prevent inadvertent fusion.
Care must be taken not to excessively expose the spine in order to prevent inadvertent fusion.
 The underlying chest wall deformity is then assessed for instability, fusion, and best sites for device attachment.
The underlying chest wall deformity is then assessed for instability, fusion, and best sites for device attachment.
 If a distal attachment for a hybrid device is needed, a separate longitudinal paraspinous skin incision, 5 cm long, is then made 1 cm lateral to the midline at the level of the proximal lumbar spine (Fig. 5).
If a distal attachment for a hybrid device is needed, a separate longitudinal paraspinous skin incision, 5 cm long, is then made 1 cm lateral to the midline at the level of the proximal lumbar spine (Fig. 5).
 A flap over the fascia is elevated medially to expose the midline of the spine. Cautery is used to longitudinally section the apophysis of the two posterior spinous processes at the correct interspace, and a Cobb elevator is used to strip the spine laterally. L2-3 is the most common interspace used.
A flap over the fascia is elevated medially to expose the midline of the spine. Cautery is used to longitudinally section the apophysis of the two posterior spinous processes at the correct interspace, and a Cobb elevator is used to strip the spine laterally. L2-3 is the most common interspace used.
 The ligamentum flavum is then resected. Gel foam is placed over the exposed dura.
The ligamentum flavum is then resected. Gel foam is placed over the exposed dura.
 If posterior elements are lacking, an S-hook over the central iliac crest may be used for hybrid attachment (Fig. 6).
If posterior elements are lacking, an S-hook over the central iliac crest may be used for hybrid attachment (Fig. 6).
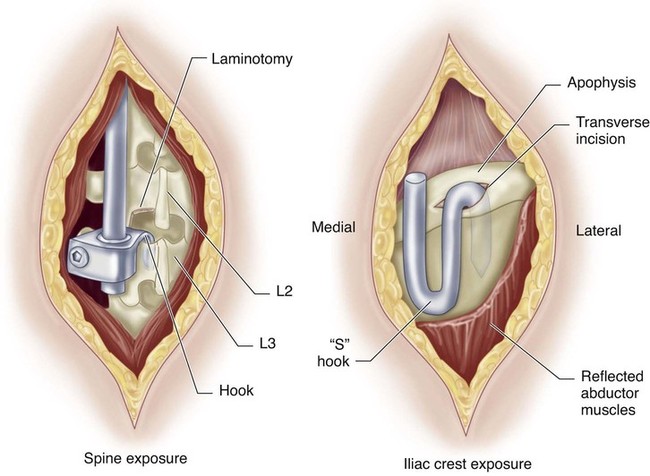
 A 5-cm longitudinal incision is made over the top of the central iliac crest. The apophysis is exposed by gentle use of a Cobb elevator.
A 5-cm longitudinal incision is made over the top of the central iliac crest. The apophysis is exposed by gentle use of a Cobb elevator.
 A 1-cm incision is made transversely by scalpel in the apophysis, with adequate cartilage below to cushion the S-hook over the crest. A Creigo retractor is inserted into the apophyseal incision to elevate the inner periosteum of the iliac crest and to probe correct position just lateral to the sacroiliac joint.
A 1-cm incision is made transversely by scalpel in the apophysis, with adequate cartilage below to cushion the S-hook over the crest. A Creigo retractor is inserted into the apophyseal incision to elevate the inner periosteum of the iliac crest and to probe correct position just lateral to the sacroiliac joint.
VEPTR Expansion Thoracoplasty
 VEPTR expansion thoracoplasty is a general category of surgical procedures that can expand the volume-constricted thorax when there is three-dimensional deformity of the thorax due to spine deformity, as well as primary rib cage deformity.
VEPTR expansion thoracoplasty is a general category of surgical procedures that can expand the volume-constricted thorax when there is three-dimensional deformity of the thorax due to spine deformity, as well as primary rib cage deformity.
 Multiple types of expansion thoracoplasties address each type of VDD of the thorax.
Multiple types of expansion thoracoplasties address each type of VDD of the thorax.
 All the procedures have in common the ability to enlarge the constricted area of the hemithorax with the goals of restoring thoracic volume, stability, and symmetry, with correction of spinal deformity without fusion, in order to allow growth of the thorax afterward.
All the procedures have in common the ability to enlarge the constricted area of the hemithorax with the goals of restoring thoracic volume, stability, and symmetry, with correction of spinal deformity without fusion, in order to allow growth of the thorax afterward.
 In contrast to classic spine fusion, in which the instrumentation “drives” the deformity correction, in VEPTR surgery the thorax first undergoes acute surgical reconstruction to increase volume and correct deformity, then the VEPTR devices are added to stabilize the reconstruction.
In contrast to classic spine fusion, in which the instrumentation “drives” the deformity correction, in VEPTR surgery the thorax first undergoes acute surgical reconstruction to increase volume and correct deformity, then the VEPTR devices are added to stabilize the reconstruction.
 The VEPTR device is made by Synthes Spine Company of West Chester, PA, and is available as a Humanitarian Use Device under an FDA Humanitarian Device Exemption, with Institutional Review Board approval required for the use of the device at each institution.
The VEPTR device is made by Synthes Spine Company of West Chester, PA, and is available as a Humanitarian Use Device under an FDA Humanitarian Device Exemption, with Institutional Review Board approval required for the use of the device at each institution.
 The first step in VEPTR treatment is to classify the thoracic VDD so that the proper VEPTR surgical strategy is chosen.
The first step in VEPTR treatment is to classify the thoracic VDD so that the proper VEPTR surgical strategy is chosen.
Procedure: VDD Type II, Fused Ribs and Scoliosis
Step 1
 The VEPTR expansion thoracoplasty for this VDD is an opening wedge thoracostomy.
The VEPTR expansion thoracoplasty for this VDD is an opening wedge thoracostomy.
 After the exposure is completed, the superior rib cradle site is chosen. The rib should be thick enough to support the corrective forces, attached solidly to the spine, and no more proximal than the second rib to avoid brachial plexus impingement.
After the exposure is completed, the superior rib cradle site is chosen. The rib should be thick enough to support the corrective forces, attached solidly to the spine, and no more proximal than the second rib to avoid brachial plexus impingement.
 A 1-cm incision is made by cautery in the intercostal muscle, immediately beneath the rib of attachment.
A 1-cm incision is made by cautery in the intercostal muscle, immediately beneath the rib of attachment.
 A Freer elevator is then inserted, pushing through the intercostal muscle to the lower edge of the rib, stripping the combined pleura/periosteum layer off from the rib anteriorly.
A Freer elevator is then inserted, pushing through the intercostal muscle to the lower edge of the rib, stripping the combined pleura/periosteum layer off from the rib anteriorly.
 A second portal is then placed by cautery above the rib of attachment. A second Freer elevator is inserted in this portal, pointing distally to strip off the periosteum of the rib anteriorly.
A second portal is then placed by cautery above the rib of attachment. A second Freer elevator is inserted in this portal, pointing distally to strip off the periosteum of the rib anteriorly.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


54: Vertical Expandable Prosthetic Titanium Rib (VEPTR) Expansion Thoracoplasty











