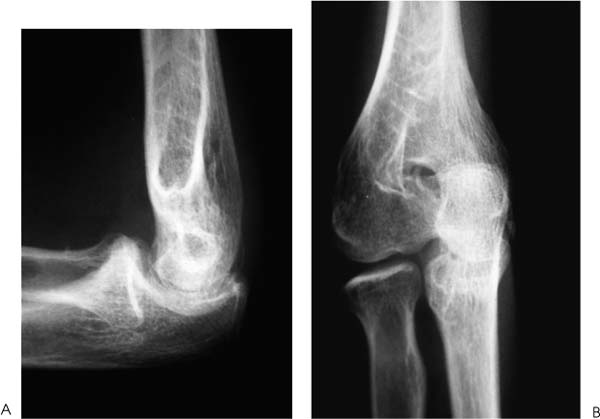
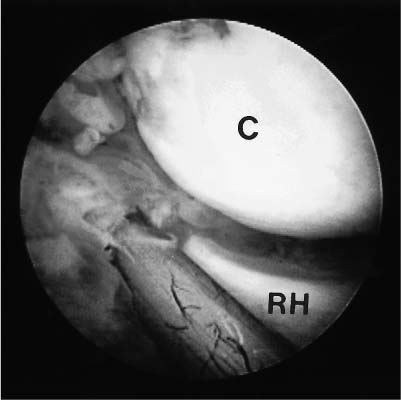
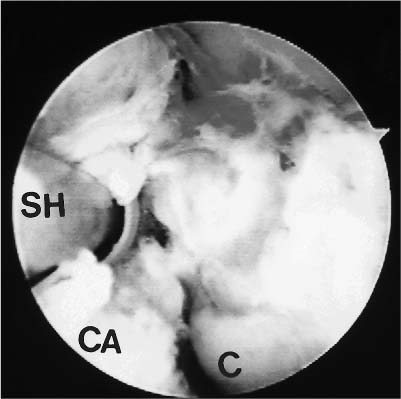
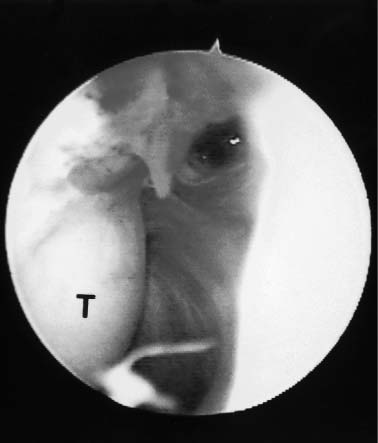
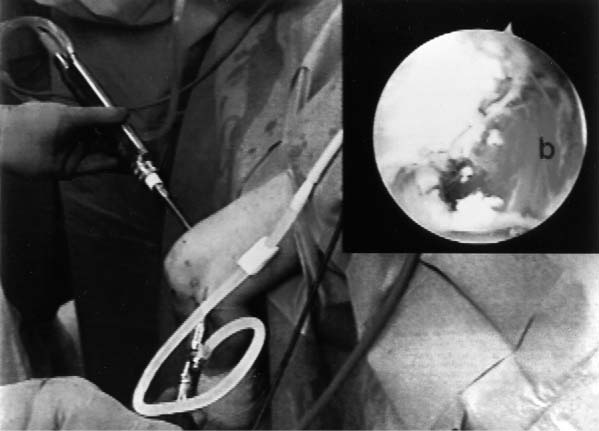
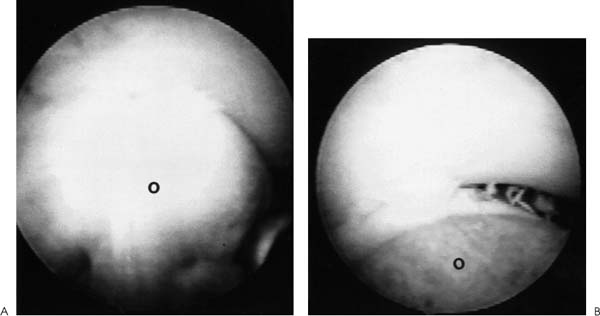
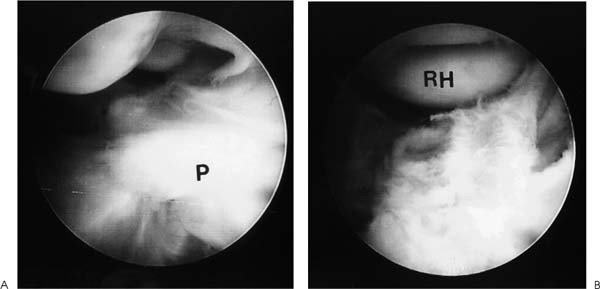
Case 52 A 23-year-old, right-hand–dominant woman presents 6 months after a posterior elbow fracture-dislocation reportedly involving the coronoid process. She reports cast immobilization for 4 weeks following her dislocation, after which time she underwent 5 months of organized physical therapy and daily exercises in an effort to improve her motion and function. She complains of elbow stiffness and pain. She denies any numbness or weakness of the hand. This young woman’s elbow range of motion is limited to 80 degrees of extension and 115 degrees of flexion. She has 45 degrees of supination and 40 degrees of pronation. No obvious elbow instability is present, and she is neurovascularly intact. Range of motion evaluation demonstrates no apparent bony block to either flexion or extension, but rather a stiff, rubbery end point. Figure 52–1. Anteroposterior (AP) (A) and lateral (B) radiographs of the elbow. 1. Chronic unreduced posterior elbow dislocation 2. Arthrofibrosis of the elbow 3. Reflex sympathetic dystrophy of the elbow Anteroposterior (AP) and lateral radiographs are obtained (Fig. 52–1). Arthrofibrosis of the Elbow. Arthrofibrosis of the elbow is diagnosed based on the severe limitations of motion of the elbow, the lack of signs and symptoms to suggest reflex sympathetic dystrophy, and the radiographic evidence of a congruent ulnohumeral joint. No obvious calcifications are present in the soft tissues or elbow capsule. This patient has undergone an extensive nonoperative treatment program following a rather extended period of strict immobilization for an elbow fracture-dislocation. Even after several months of organized therapy and exercises, her functional arc of motion is very limited. Although extensive exercises following a fracture-dislocation of the elbow are recommended, additional time and exercises are unlikely to improve this patient’s motion to a functional range. Surgical intervention will afford her the best opportunity to improve. Contracture of the elbow is best defined as loss of extension or flexion sufficient to cause functional limitation. It may be caused by fractures, dislocations, arthritic/osteochondritic conditions, burns, or cerebral problems such as stroke or head injury. These conditions may be arbitrarily grouped into intrinsic (intraarticular changes: fracture, bone spurs, loose bodies, synovitis), extrinsic (contracture/scarring of the capsule, collateral ligaments, flexor/extensor musculature, heterotopic bone, and/or skin) or peripheral (head injury, neurologic dysfunction) etiologies. In treating patients with elbow flexion contracture, the etiology of the contracture must be considered prior to treatment. Patients with skin contracture and muscle spasticity must obviously be managed in a different fashion from those with intraarticular fracture or arthritic conditions. Careful evaluation of the neurovascular structures and their potential involvement in the contracted tissue must be considered. The choice of surgical technique to accomplish release of this significant elbow contracture centers around an arthroscopic or open technique. The arthroscopic approach is technically demanding and should be performed only by surgeons with extensive experience in elbow arthroscopy. However, this approach does provide an excellent opportunity to address both the intrinsic and relevant extrinsic components of a combined elbow contracture problem, without the extensive dissection and iatrogenic trauma incurred with open release techniques. Nevertheless, open techniques have proven valuable and should be used in certain clinical situations that preclude the safe use of arthroscopic techniques. A relative contraindication to the use of the arthroscope in the treatment of significant elbow contracture is marked intrinsic deformity, such as severe malunions of the distal humerus or radial head, because normal anatomic landmarks will not be present to act as a guide for the arthroscopist. Also, extrinsic contractures due to muscle spasticity or skin contracture are not responsive to arthroscopic intraarticular releases. Furthermore, when neurovascular structures are intimately involved with the contractured tissue, such as would occur with the radial nerve and posterior interosseous nerve following a severely displaced and malunited radial head fracture, arthroscopic techniques for contracture release are not recommended. Arthroscopy for surgical release of elbow flexion contractures begins in the prone position. The 4.5- or 5.0-mm arthroscope and shaver are utilized, along with the standard camera and video recording equipment. The arm is elevated on a 4-inch block placed on a standard arm board oriented parallel to the operating room table to allow adequate mobility of the elbow and portal access. The limb is then exsanguinated and the tourniquet inflated to the prescribed setting, usually between 250 and 300 mm Hg. The patient is then prepped and draped in a sterile fashion. During draping the forearm distal to the elbow joint is firmly wrapped with Coban compressive wrapping material. This decreases the space for fluid extravasation during the procedure, and increases the space available for extravasated fluid after the conclusion of the procedure. Motion in the elbow is then tested in forearm pronation, neutral rotation, and supination. Insufflation of the elbow is then attempted using a standard soft spot portal. A proximal medial portal is established approximately 2 cm proximal to the medial epicondyle and just anterior to the medial intermuscular septum. As with all portal placement, care is taken to avoid injury to the cutaneous nerves by pulling the skin against the scalpel blade during this incision. A blunt trocar is used to palpate the intermuscular septum and then is directed anterior to this structure, penetrating the muscle layers overlying the capsule of the elbow joint. Joint entrance is then attempted utilizing the blunt trocar. Occasionally a sharp trocar is needed to penetrate the thickened, scarred capsule and allow adequate entrance into the elbow joint. The arthroscope is then introduced through this cannula and the anterior compartment of the elbow is evaluated. A proximal anterolateral portal is then established. An outside-in technique using a spinal needle is preferred, but in many cases an inside-out technique with the Wissinger rod is necessary. Protection of the posterior interosseous nerve is paramount during lateral portal placement. The portal should be placed just superior to the capitellum to establish safe placement. A second cannula is then inserted in this area and used to remove inflamed soft tissues and adhesions from the radial head and coronoid process. This debridement is continued with the elbow in pronation as well as supination, for complete debridement of the anterior radiocapitellar joint (Fig. 52–2). Anterior capsulectomy is then initiated. The scope remains in the proximal me-dial portal and the shaver in the proximal anterolateral portal. The capsule is released from the humerus, beginning near the coronoid fossa. Release is continued laterally until a complete release of the capsule from the midportion of the humerus to the lateral intermuscular septum has been accomplished (Fig. 52–3). The proximal 1 to 2 cm of the capsule are completely excised to prevent simple elevation of the capsule from the humerus. The arthroscope is then switched to the proximal anterolateral portal and the shaver introduced through the proximal medial portal. The capsular excision is continued medially, until the intermuscular septum at the medial humeral cortex has been visualized. Care must be taken not to extend the capsular excision past this point because of risk of injury to the ulnar nerve. The proximal 1 to 2 cm of the capsule is excised from septum to septum until brachialis fibers are visible (Figs. 52–3 to 52–5). Capsular release is continued until the capsular structures are no longer tight, a posterior block to extension is encountered, or brachialis muscle fibers are visible from medial to lateral under direct arthroscopic visualization (Fig. 52–5). To avoid potential neurovascular complications, it is very important to confirm that both the arthroscope and shaver are in the joint at all times, as well as to maintain proximity of the shaver blade to the anterior aspect of the humerus at all times. Figure 52–2. This view of the anterior lateral capsule from the proximal medial portal shows the early stages of debridement of the anterior radial capitellar joint. The capitellum (C) is above the radial head (RH) to the lower right. (See Color Plate 52–2.) Figure 52–3. The initial phase of the lateral capsular excision as viewed from the proximal medial portal. The proximal aspect of the capitellum (C) is in the lower right of the figure, the humeral cortex on the top right and the capsule to the left. SH, shaver; CA, capsule. (See Color Plate 52–3.) Figure 52–4. The arthroscope in the anterior superior lateral portal is used to visualize the initial phase of the resection of the medial capsular structures. The trochlea (T) is to the left. (See Color Plate 52–4.) Figure 52–5. Completed anterior capsular release showing brachialis (b) muscle fibers visible from within the joint. (See Color Plate 52–5.) Once maximum extension through anterior capsular release has been achieved, the instruments are removed from the anterior portals and a posterior lateral and posterior central portal established. The arthroscope is inserted through the posterior lateral portal with the shaver inserted through the posterior central portal. Scar tissue and adhesions are removed from the olecranon fossa utilizing a full radius soft tissue shaver blade. The olecranon itself is then debrided of osteophytes utilizing a burr or notchplasty-type blade. Olecranon excision is continued until full extension can be obtained (Fig. 52–6). It is important to resect all spurs from the medial and lateral aspects of the olecranon. To increase the point of maximum flexion, any posterior capsular adhesions are debrided from the posterior superior portion of the elbow joint. Removal of adhesions between the triceps tendon and the posterior humerus should allow increased flexion of the elbow. The final portion of the release is accomplished by debriding the medial and lateral gutters of scar tissue and adhesions. The arthroscope is placed in the posterior central portal and the shaver in the posterior lateral portal. Excision of adhesions in the lateral gutter is initiated proximally and continues distally. A straight lateral soft spot portal may be necessary to adequately debride the posterior radiocapitellar joint, posterior radioulnar joint, and posterolateral plica (Fig. 52–7). The arthroscope is then shifted to the posterior lateral portal and the shaver switched to the posterior central portal for debridement of the medial gutter. A fully hooded shaver should be utilized along the medial gutter to prevent injury to the ulnar nerve. Figure 52–6. (A) Olecranon (O) spur. (B) Completed excision of the olecranon spur. (See Color Plates 52–6A,B.) Figure 52–7. (A) Posterolateral plica (P) of the elbow. (B) Completed excision and debridement of the posterolateral plica adjacent to the radial head (RH). (See Color Plates 52–7A,B.) Following the procedure drains may be inserted in the proximal medial and posterior central or posterior lateral portal. The lateral soft spot portal is sutured, but the remaining portals are left open. Sterile bandages are applied after a final determination of range of motion. The elbow is placed in full extension and supination and held in this position by placement of anterior and posterior splints. For patients who are not candidates for arthroscopic release of their contracture, or when the surgeon does not have adequate expertise for this technically demanding surgery, open release is performed. The type of surgical correction with an open release will depend on the nature of the contracture. Contractures usually result from a combination of intrinsic and extrinsic factors including muscle imbalance, soft tissue scarring, bony or mechanical impingement, and degenerative articular changes. Most open releases can be accomplished through an extended Kocher approach. This lateral incision is made after tourniquet inflation and proceeds along the lateral supracondylar ridge of the humerus. It passes directly over the lateral epicondyle and proceeds distally between the anconeus and extensor carpi ulnaris. This incision is generally extended distally down to the subcutaneous border of the ulna. Dissection is carried out through the subcutaneous tissues. The brachioradialis, extensor carpi radialis longus, and a portion of the extensor carpi radialis brevis are sharply elevated from the anterior humeral cortex. The anterior capsule can then be exposed and is resected widely. This capsular excision is important, as simple release of the capsule will lead to recurrent contracture. The surgeon must take extreme care medially along the capsule to ensure that the medial ulnar collateral ligament is not incised and that the ulnar nerve is not injured. Osteophytes from the coronoid process should also be excised at this time. The lateral approach also allows for simultaneous posterior exposure when necessary. The triceps can be elevated from the posterior humerus. Frequently the olecranon fossa is filled with fibrotic tissue and osteophytes. These must be excised so as to allow for movement of the olecranon process without impingement. If more extensive release medially is required, a small separate posteromedial incision can be made. Likewise, when significant ulnar neuritis is present, a separate medial incision is made so as to transpose the ulnar nerve. Alternatively, an extended medial approach with capsular release and ulnar nerve transposition can be carried out, instead of performing a lateral approach. The indications for medial, lateral, or combined incisions depend on the clinical situation and the etiology of the elbow contracture. Elbow contractures can sometimes be primarily due to malunion of a distal humerus fracture. Release of the soft tissue component of the contracture alone may not restore adequate motion. Low supracondylar or transcondylar fractures that malunite can eliminate the normal anterior projection of the distal humerus. Loss of normal anterior humeral projection will often preclude full flexion. Partial excision of the coronoid process and soft tissue release can improve motion, but is sometimes inadequate. In these situations, correctional osteotomy may be required in addition to contracture release. Such osteotomies necessitate rigid plate fixation so as to allow for immediate motion following release and reconstruction. Extensive dissection and exposure is required to perform these osteotomies adequately. The choice of approach is dictated by the contracture and/or malunion. • Static or dynamic splinting, or both, are extremely valuable in the early postoperative period. • Deterioration of motion in the first few weeks following release should be treated by manipulation in the operating room. If arthroscopic release of elbow contracture is attempted, a low threshold for cessation of the arthroscopic technique should be maintained. Open release can always be performed. At best, a poorly performed arthroscopic release will be inadequate and at worst will cause catastrophic neurovascular injury.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Surgical Technique for Arthroscopic Release for Elbow Contracture
Surgical Technique for Open Release of Elbow Flexion Contracture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree