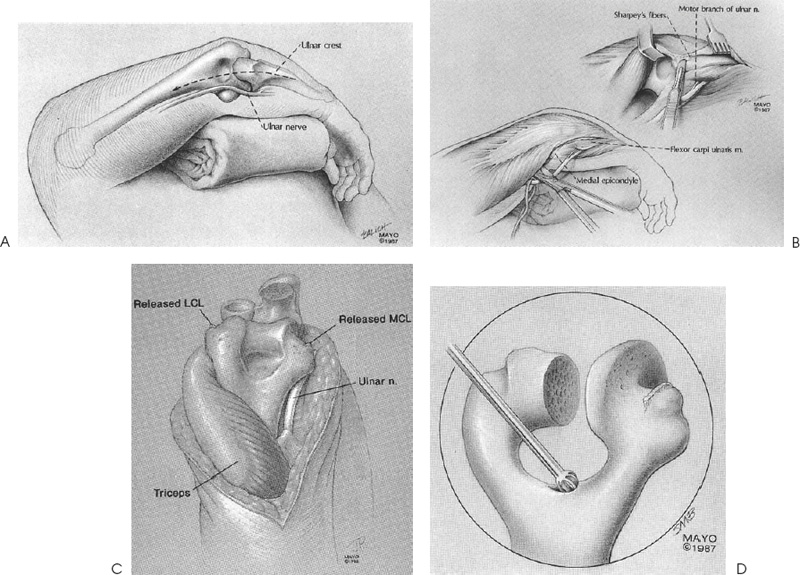
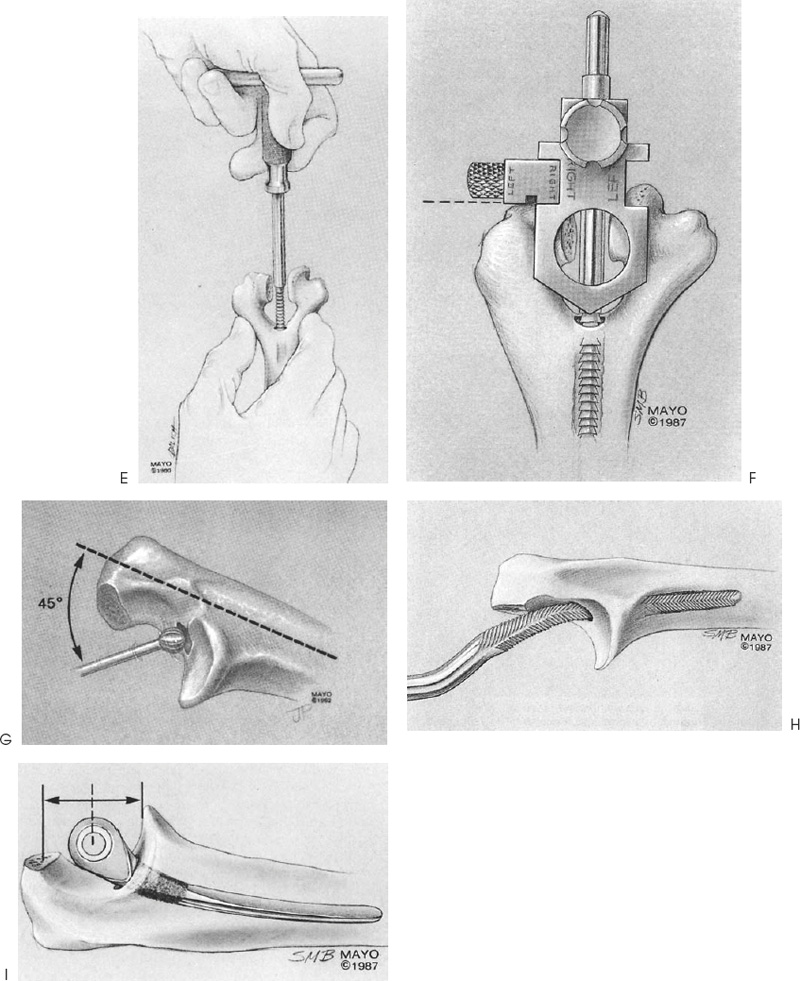
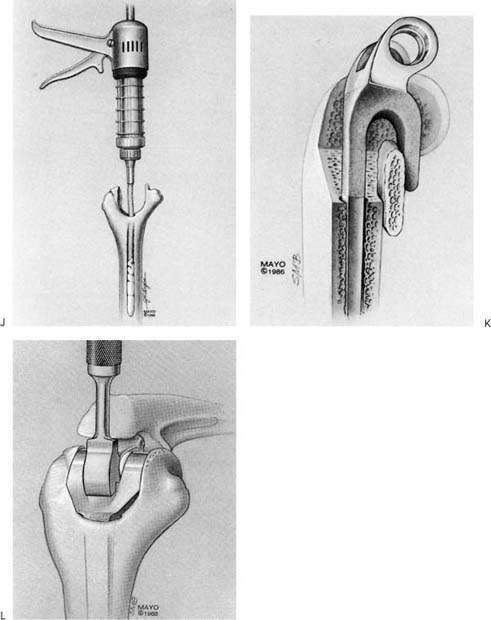
Case 51 A 66-year-old woman presents with a 5-year history of progressive elbow pain and loss of motion. Her history is significant for rheumatoid arthritis for 15 years. She denies any recent trauma to her elbow, although she says that her symptoms have worsened over the last 6 months. Range of motion of 40 to 90 degrees of the elbow is possible passively and actively. Moderate effusion and marked instability of the elbow to varus and valgus testing is present as well. Palpable crepitation to manipulation of the elbow is also present. Her ipsilateral hand function is good and she denies any significant ipsilateral shoulder problems. The patient is neurovascularly intact, has good range of motion of her neck, and demonstrates normal deep tendon reflexes. Figure 51–1. Anteroposterior (AP) (A) and lateral (B) radiographs of the elbow. 1. Elbow degeneration secondary to rheumatoid arthritis 2. Nonunion of a distal humerus fracture 3. Elbow synovitis Anteroposterior (AP) and lateral radiographs of the elbow are obtained (Fig. 51–1). Severe Elbow Degeneration. The marked instability present on examination and the long-standing history of arthritis suggests severe articular degeneration. Radiographs confirm the complete loss of articular congruity felt clinically. Diagnosis is made easy by radiographs and is not readily confused with other entities. The indications for total elbow arthroplasty include severe articular degeneration with pain and instability due to rheumatoid arthritis. The loss of function seen in this patient can cause the inability to perform activities of daily living because of pain, loss of motion, and instability. Rheumatoid arthritis is the most common disease necessitating total elbow replacement. However, to be considered a candidate for total elbow replacement, the patient should have marked joint destruction and have failed conservative treatment measures. These treatments include local cortisone injections and the administration of remittive drugs for rheumatoid arthritis. Also, only radiographic class III or IV changes should be evident. Patients with less significant destruction are probably better candidates for arthroscopic or open synovectomy, with or without radial head resection. A comprehensive examination of the patient’s upper extremity and neck should be performed prior to recommending total elbow replacement. A thorough cervical spine examination with neurologic testing should be performed. Both upper extremities should be evaluated and hand function is critical to establish. If lower extremity surgery is required, it should probably be performed before elbow replacement because of the requirement of the use of canes and walkers following surgery. Careful evaluation of the shoulder should also be accomplished. Elbow surgery should usually take place prior to shoulder surgery, except when severe limitation of shoulder motion is present. After careful evaluation of this patient, total elbow arthroplasty was recommended. One of the goals of the surgery is to achieve postoperative stability. The authors prefer the semiconstrained, Coonrad-Morrey total elbow arthroplasty, using the surgical exposure and technique recommended for this prosthesis (Fig. 51–2). The patient is placed supine on the operating table with the arm draped free. The Bryan-Morrey approach is used for this procedure. A 15- to 20-cm incision is made just lateral to the medial epicondyle and just medial to the tip of the olecranon. The medial aspect of the triceps is identified and the ulnar nerve isolated and protected throughout the procedure. The ulnar periosteum, the forearm fascia, and the triceps are all carefully elevated. The extensor musculature, including the anconeus, is reflected laterally, allowing complete exposure of the distal humerus, the proximal ulna, and the radial head. The lateral collateral ligament complex is released from the overlying anconeus. The tip of the olecranon is then removed. Exposure of the distal humerus allows for proper bone resection. First, the medullary canal of the humerus is identified and twist reamers used to expand the canal. Care is taken to visualize the medial and lateral aspects of the supracondylar columns as well as the medial and lateral epicondyles. An alignment stem is placed down the medullary canal and a cutting block attached to rest on the capitellum. An oscillating saw is used to make appropriate cuts. Trial components are then sized. Attention is next turned to the ulna, where the medullary canal is identified by using a high-speed burr. Sequential rasps are used to expand the canal and trial implants sized. The medullary cavities of both bones are cleansed with a lavage irrigation system and dried. The components are then assembled and inserted as a unit after cement is placed into the humeral and ulnar canals. The arm is extended until cement hardening has occurred. Prior to final seating of the humerus, a bone plug is placed posterior to the flange of the distal humeral component, as this increases its stability. Range of motion is confirmed and hemostasis is obtained. The ulnar nerve is routinely transposed into a subcutaneous position. Suction drains are placed in the wound and closure is routine. The patient is placed in a soft dressing. Postoperative radiographs are imperative to ensure appropriate alignment (Fig. 51–3). Figure 51–2. Recommended technique for Coonrad-Morrey total elbow arthroplasty. (A) A posterior elbow incision is made. (B) The ulnar nerve is identified and the posterior and lateral musculature and ligamentous structures are carefully elevated from the ulna. (C) The bony landmarks are identified on the humerus following excision of the olecranon tip. (D) The medullary canal of the humerus is identified using a high-speed burr. (E) An alignment stem is placed down the medullary canal of the humerus. (F) A cutting block is then placed at the appropriate height. (G) Attention is turned to the ulna and medullary canal is identified using a high-speed burr. (H) Sequential rasps are used to expand the canal. (I) The ulnar component is placed so that the arc of rotation coincides with the center of the greater sigmoid fossa. (J) Cement is placed down the humeral and ulnar canals. (K) An anterior bone block is used under the flange prior to final seating. (L) Final seating is accomplished. (Reprinted from Morrey BF, Adams RA. Semiconstrained elbow replacement arthroplasty: rationale, technique, and results. In: Morrey B, ed. The Elbow and Its Disorders, pp. 652–656. Philadelphia: WB Saunders, 1993. With permission.) No formal therapy is generally prescribed and gentle active range of motion and passive range of motion exercises are encouraged. Care is taken to avoid heavy lifting or demanding elbow extension for 3 to 4 weeks, but otherwise routine activities are allowed. • The authors always mix tobramycin powder with the cement at the time of implant placement to reduce the risk of postoperative deep infection. • In very osteopenic rheumatoid arthritis patients, intraoperative use of a fluoroscopic unit or radiographs can sometimes be helpful in confirming intramedullary placement of the rasps.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Postoperative Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree