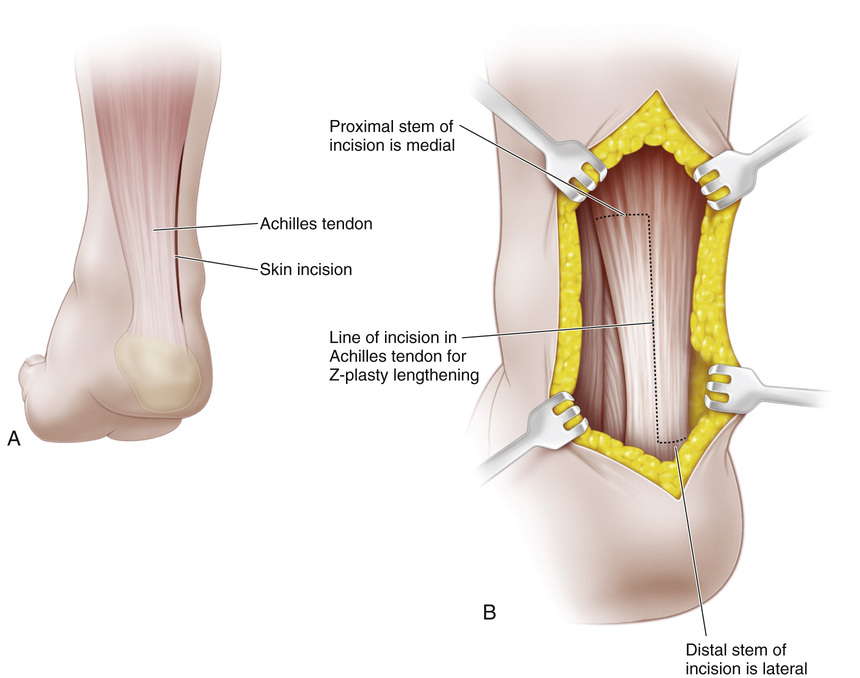
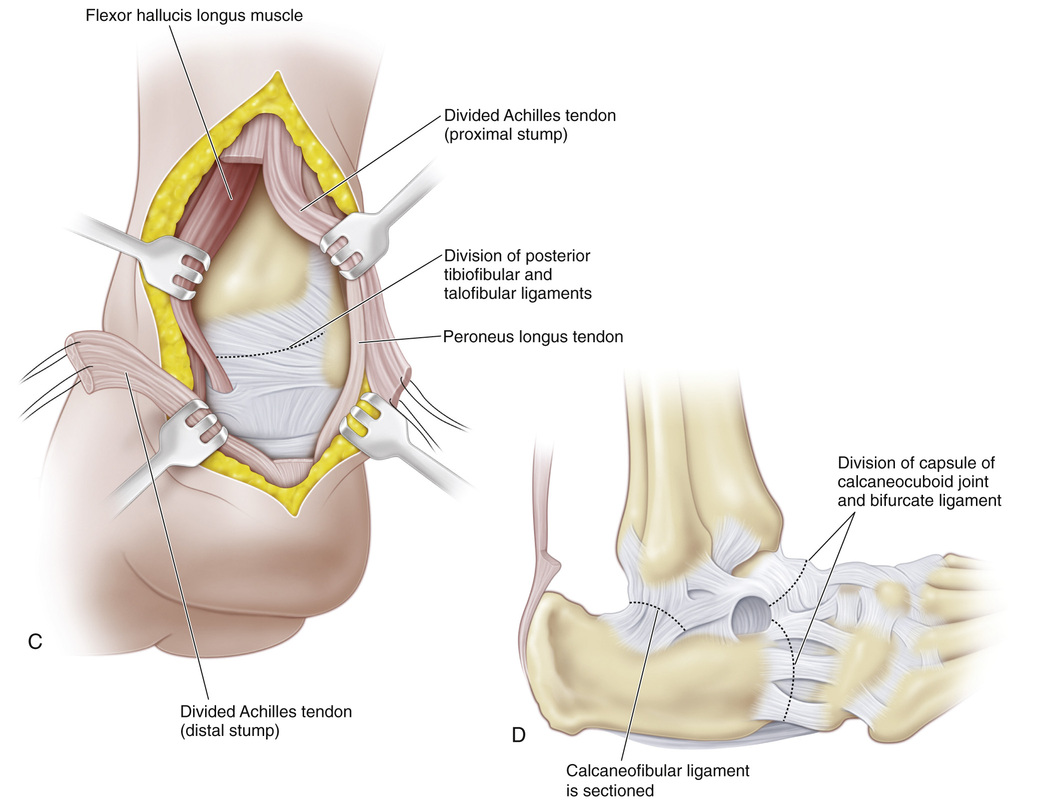
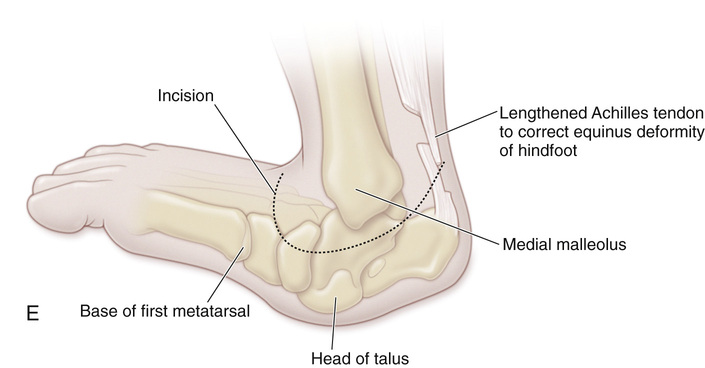
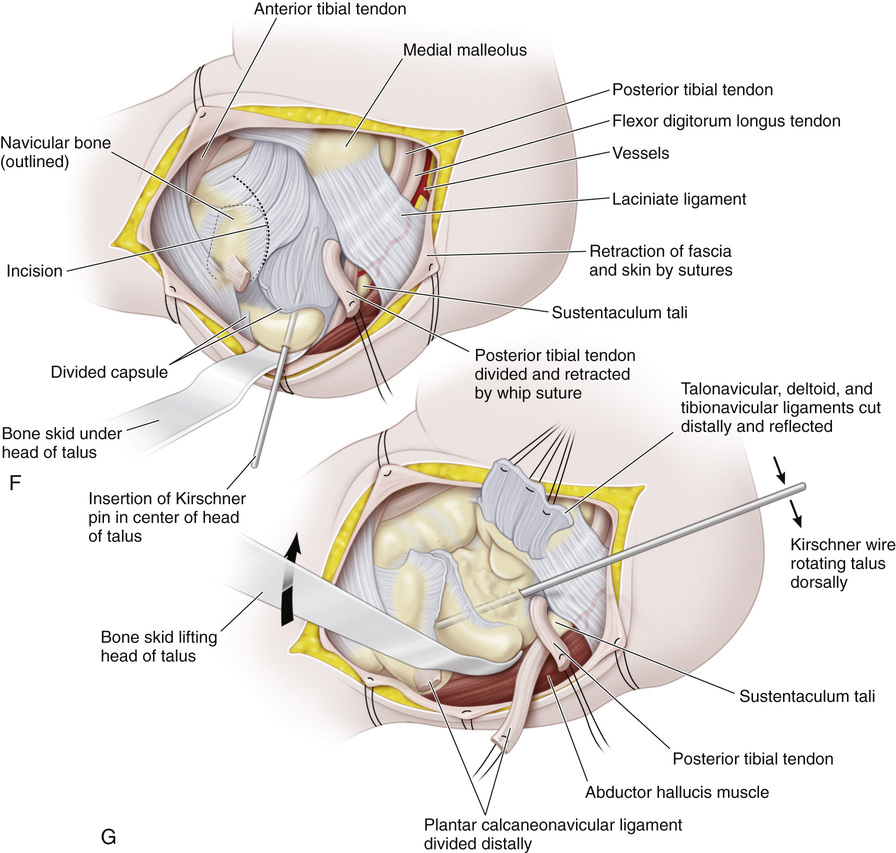
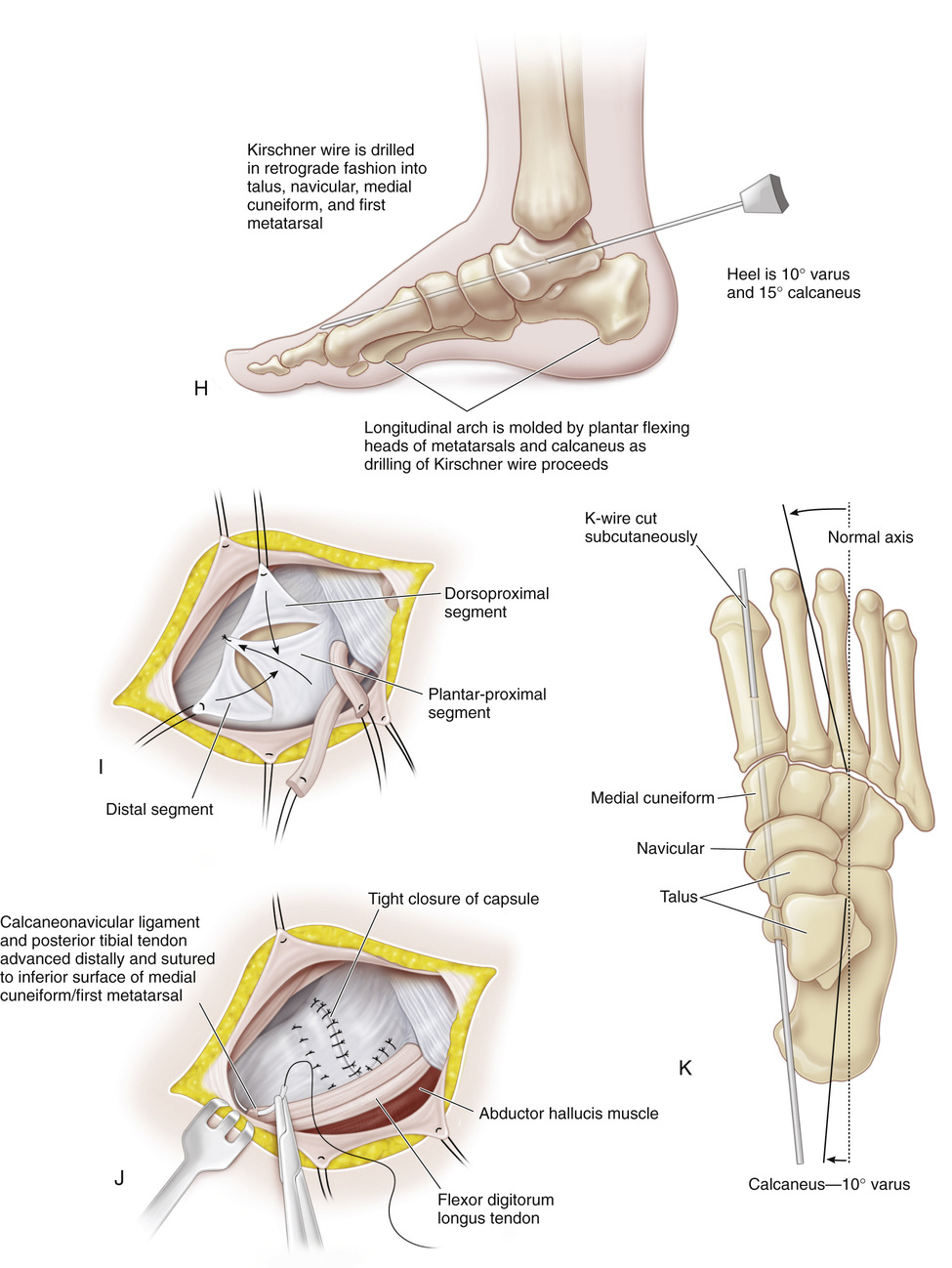
A, A longitudinal incision is made lateral to the tendo calcaneus, beginning at the heel and extending proximally for a distance of 7 to 10 cm. The subcutaneous tissue and tendon sheath are divided in line with the skin incision, and the wound flaps are retracted to expose the Achilles tendon. B, Z-plasty lengthening is performed in the anteroposterior plane. With a knife, the Achilles tendon is divided longitudinally into lateral and medial halves for a distance of 5 to 7 cm. The distal end of the lateral half is detached from the calcaneus to prevent recurrence of valgus deformity of the heel; the medial half is divided proximally. When the equinus deformity is not marked, sliding lengthening of the heel cord is performed. C and D, A posterior capsulotomy of the ankle and subtalar joint is performed if necessary. The calcaneofibular ligament is sectioned. The thickened capsule of the calcaneocuboid joint and the bifurcate ligament are divided through a separate lateral incision. The Cincinnati transverse incision is an alternative surgical approach; it is preferred by these authors. E, The incision is a modified Cincinnati incision that passes beneath the medial malleolus just past the Achilles tendon posteriorly and proceeds dorsally over the navicular just past the extensor tendons. F and G, The posterior tibial tendon is identified, dissected, and divided at its insertion to the tuberosity of the navicular. The end of the tendon is marked with 0 Mersilene suture for later reattachment. The articular surface of the head of the talus points steeply downward and medially to the sole of the foot and is covered by the capsule and ligament. The navicular will be found against the dorsal aspect of the neck of the talus, where it locks the talus in a vertical position. The pathologic anatomy of the ligaments and capsule is noted, and the incisions are planned so that a secure capsuloplasty can be performed and the talus maintained in its normal anatomic position. Circulation to the talus is another important consideration; it should be disturbed as little as possible by exercising great care and gentleness during dissection. Avascular necrosis of the talus is always a potential serious complication of open reduction. The plantar calcaneonavicular ligament is identified and divided distally from its attachment to the sustentaculum tali, and 00 Mersilene suture is inserted in its end for later reattachment. The talonavicular articulation is exposed by a T incision. The transverse limb of the T is made distally over the tibionavicular ligament (the anterior portion of the deltoid ligament) and over the dorsal and medial portions of the talonavicular ligament. A cuff of capsule is kept attached to the navicular for plication on completion of surgery. The longitudinal limb of the incision is made over the head and neck of the talus inferiorly. The articular surface of the head of the talus is identified, and a large threaded Kirschner wire is inserted in its center. With a skid and the leverage of the Kirschner wire, the head and neck of the talus are lifted dorsally and the forefoot is manipulated into plantar flexion and inversion to bring the articular surfaces of the navicular and head of the talus into normal anatomic position. H, The Kirschner wire is drilled retrograde into the navicular, cuneiform, and first metatarsal bones to maintain the reduction. Radiographs of the foot are obtained at this time to verify the reduction. In severe cases, the calcaneocuboid and talocalcaneal interosseous ligaments may prevent reduction of the laterally subluxated Chopart and subtalar joints. They are divided when necessary to allow reduction. In addition, the extensor hallucis, extensor digitorum longus, and occasionally the peroneals may be contracted. They should be Z-lengthened to allow reduction of the foot into plantar flexion. These releases require extension of the incision over the dorsum of the foot. I and J, A careful capsuloplasty is very important for maintaining the reduction and normal anatomic relationship of the talus and navicular. The redundant inferior part of the capsule should be tightened by plication and overlapping of its free edges. First, the plantar-proximal segment of the T of the capsule is pulled dorsally and distally and sutured to the dorsal corner of the inner surface of the distal capsule. Next, the dorsoproximal segment of the T is brought plantarward and distally over the plantar-proximal segment of the capsule and sutured to the plantar corner on the inner surface of the distal capsule. Interrupted sutures are then used to tighten the capsule on its plantar and medial aspects by bringing the distal segment over the proximal segments. The plantar calcaneonavicular ligament is sutured under tension to the base of the first metatarsal. To tighten the posterior tibial tendon under the head of the talus, it is advanced distally and sutured to the inferior surface of the first cuneiform. The anterior tibial tendon may be transferred to provide additional dynamic force for maintaining the navicular in correct relation to the talus. The tendon is detached from its insertion to the medial cuneiform and first metatarsal bone, and dissected free proximally and medially for a distance of 5 cm. It is then redirected to pass along the medial aspect of the neck of the talus and beneath the head of the talus, where it is fixed to the inferior aspects of the talus and navicular with 00 Mersilene sutures. Normally, the lower end of the anterior tibial tendon may be split near its insertion. Often the authors leave the attachment to the first metatarsal intact and divide only the insertion to the medial cuneiform. The tendon is split (if not normally bifurcated), and the portion to the medial cuneiform bone is transferred to the head of the talus and the navicular. Sometimes, after adequate capsuloplasty, the reduction of the talonavicular joint is so stable that anterior tibial transfer is not necessary to restore support to the head of the talus. K, The wounds are then closed in routine fashion. The Kirschner wire across the talonavicular joint is cut subcutaneously. To maintain the normal anatomic relationship of the os calcis to the talus, a Kirschner wire is inserted transversely in the os calcis and incorporated into the cast. An alternative method is to pass the wire from the sole of the foot upward through the calcaneus into the talus. The authors prefer the former because it controls the heel in the cast and prevents recurrence of both equinus deformity and eversion of the hindfoot. An above-knee cast is applied with the knee in 45 degrees of flexion, the ankle in 10 to 15 degrees of dorsiflexion, the heel in 10 degrees of inversion, and the forefoot in plantar flexion and inversion. The longitudinal arch and the heel in the cast are well molded.
Open Reduction of Dorsolateral Dislocation of the Talocalcaneonavicular Joint (Congenital Vertical Talus)
Operative Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








